Diabetes Metab J.
2022 Mar;46(2):327-336. 10.4093/dmj.2021.0046.
Changes in Patterns of Physical Activity and Risk of Heart Failure in Newly Diagnosed Diabetes Mellitus Patients
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Statistics and Actuarial Science, Soongsil University, Seoul, Korea
- 3Department of Biostatistics, Biomedicine & Health Sciences, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2527725
- DOI: http://doi.org/10.4093/dmj.2021.0046
Abstract
- Background
Exercise is recommended for type 2 diabetes mellitus (T2DM) patients to prevent cardiovascular disease. However, the effects of physical activity (PA) for reducing the risk of heart failure (HF) has yet to be elucidated. We aimed to assess the effect of changes in patterns of PA on incident HF, especially in newly diagnosed diabetic patients.
Methods
We examined health examination data and claims records of 294,528 participants from the Korean National Health Insurance Service who underwent health examinations between 2009 and 2012 and were newly diagnosed with T2DM. Participants were classified into the four groups according to changes in PA between before and after the diagnosis of T2DM: continuously inactive, inactive to active, active to inactive, and continuously active. The development of HF was analyzed until 2017.
Results
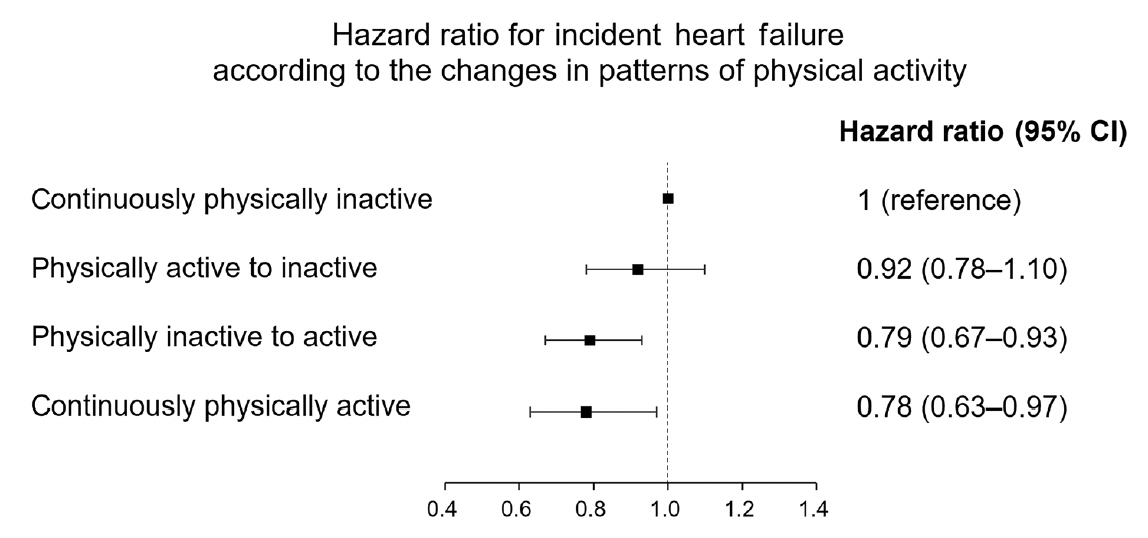
As compared with those who were continuously inactive, those who became physically active after diagnosis showed a reduced risk for HF (adjusted hazard ratio [aHR], 0.79; 95% confidence interval [CI], 0.66 to 0.93). Those who were continuously active had the lowest risk for HF (aHR, 0.77; 95% CI, 0.62 to 0.96). As compared with those who were inactive, those who exercised regularly, either performing vigorous or moderate PA, had a lower HF risk (aHR, 0.79; 95% CI, 0.69 to 0.91).
Conclusion
Among individuals with newly diagnosed T2DM, the risk of HF was reduced in those with higher levels of PA after diagnosis was made. Our results suggest either increasing or maintaining the frequency of PA after the diagnosis of T2DM may lower the risk of HF.
Keyword
Figure
Cited by 1 articles
-
Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes Metab J. 2023;47(1):10-26. doi: 10.4093/dmj.2022.0420.
Reference
-
1. Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013; 6:606–19.2. Lee JH, Lim NK, Cho MC, Park HY. Epidemiology of heart failure in Korea: present and future. Korean Circ J. 2016; 46:658–64.
Article3. Shiba N, Nochioka K, Miura M, Kohno H, Shimokawa H; CHART-2 Investigators. Trend of westernization of etiology and clinical characteristics of heart failure patients in Japan: first report from the CHART-2 study. Circ J. 2011; 75:823–33.
Article4. Rhee EJ, Kwon H, Park SE, Han KD, Park YG, Kim YH, et al. Associations among obesity degree, glycemic status, and risk of heart failure in 9,720,220 Korean adults. Diabetes Metab J. 2020; 44:592–601.
Article5. Florido R, Kwak L, Lazo M, Nambi V, Ahmed HM, Hegde SM, et al. Six-year changes in physical activity and the risk of incident heart failure: ARIC study. Circulation. 2018; 137:2142–51.
Article6. Florido R, Kwak L, Lazo M, Michos ED, Nambi V, Blumenthal RS, et al. Physical activity and incident heart failure in high-risk subgroups: the ARIC study. J Am Heart Assoc. 2020; 9:e014885.
Article7. Chun MY. Validity and reliability of Korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med. 2012; 33:144–51.
Article8. Jeong HG, Kim DY, Kang DW, Kim BJ, Kim CK, Kim Y, et al. Physical activity frequency and the risk of stroke: a nationwide cohort study in Korea. J Am Heart Assoc. 2017; 6:e005671.
Article9. Yun JS, Park YM, Han K, Cha SA, Ahn YB, Ko SH. Severe hypoglycemia and the risk of cardiovascular disease and mortality in type 2 diabetes: a nationwide population-based cohort study. Cardiovasc Diabetol. 2019; 18:103.
Article10. Seo MH, Kim YH, Han K, Jung JH, Park YG, Lee SS, et al. Prevalence of obesity and incidence of obesity-related comorbidities in Koreans based on national health insurance service health checkup data 2006-2015. J Obes Metab Syndr. 2018; 27:46–52.11. Kim MK, Han K, Koh ES, Kim ES, Lee MK, Nam GE, et al. Blood pressure and development of cardiovascular disease in Koreans with type 2 diabetes mellitus. Hypertension. 2019; 73:319–26.
Article12. Kim MK, Han K, Kim HS, Park YM, Kwon HS, Yoon KH, et al. Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: a nationwide population-based study. Eur Heart J. 2017; 38:3560–6.
Article13. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999; 130:461–70.
Article14. Kim YH, Kim SM, Han KD, Son JW, Lee SS, Oh SW, et al. Change in weight and body mass index associated with allcause mortality in Korea: a nationwide longitudinal study. J Clin Endocrinol Metab. 2017; 102:4041–50.
Article15. Johnson JL, Slentz CA, Ross LM, Huffman KM, Kraus WE. Ten-year legacy effects of three eight-month exercise training programs on cardiometabolic health parameters. Front Physiol. 2019; 10:452.
Article16. Swain DP, Franklin BA. Comparison of cardioprotective benefits of vigorous versus moderate intensity aerobic exercise. Am J Cardiol. 2006; 97:141–7.
Article17. Slentz CA, Tanner CJ, Bateman LA, Durheim MT, Huffman KM, Houmard JA, et al. Effects of exercise training intensity on pancreatic beta-cell function. Diabetes Care. 2009; 32:1807–11.18. Johnson JL, Slentz CA, Houmard JA, Samsa GP, Duscha BD, Aiken LB, et al. Exercise training amount and intensity effects on metabolic syndrome (from Studies of a Targeted Risk Reduction Intervention through Defined Exercise). Am J Cardiol. 2007; 100:1759–66.
Article19. Maack C, Lehrke M, Backs J, Heinzel FR, Hulot JS, Marx N, et al. Heart failure and diabetes: metabolic alterations and therapeutic interventions: a state-of-the-art review from the Translational Research Committee of the Heart Failure Association-European Society of Cardiology. Eur Heart J. 2018; 39:4243–54.
Article20. Rodrigues B, Cam MC, McNeill JH. Metabolic disturbances in diabetic cardiomyopathy. Mol Cell Biochem. 1998; 180:53–7.
Article21. Stewart KJ. Exercise training and the cardiovascular consequences of type 2 diabetes and hypertension: plausible mechanisms for improving cardiovascular health. JAMA. 2002; 288:1622–31.
Article22. Gademan MG, Swenne CA, Verwey HF, van der Laarse A, Maan AC, van de Vooren H, et al. Effect of exercise training on autonomic derangement and neurohumoral activation in chronic heart failure. J Card Fail. 2007; 13:294–303.
Article23. Napoli C, Williams-Ignarro S, De Nigris F, Lerman LO, Rossi L, Guarino C, et al. Long-term combined beneficial effects of physical training and metabolic treatment on atherosclerosis in hypercholesterolemic mice. Proc Natl Acad Sci U S A. 2004; 101:8797–802.
Article24. Nunes RB, Tonetto M, Machado N, Chazan M, Heck TG, Veiga AB, et al. Physical exercise improves plasmatic levels of IL-10, left ventricular end-diastolic pressure, and muscle lipid peroxidation in chronic heart failure rats. J Appl Physiol (1985). 2008; 104:1641–7.
Article25. Conraads VM, Beckers P, Bosmans J, De Clerck LS, Stevens WJ, Vrints CJ, et al. Combined endurance/resistance training reduces plasma TNF-alpha receptor levels in patients with chronic heart failure and coronary artery disease. Eur Heart J. 2002; 23:1854–60.
Article26. Lavie CJ, Thomas RJ, Squires RW, Allison TG, Milani RV. Exercise training and cardiac rehabilitation in primary and secondary prevention of coronary heart disease. Mayo Clin Proc. 2009; 84:373–83.
Article27. Lavie CJ, Alpert MA, Ventura HO. Risks and benefits of weight loss in heart failure. Heart Fail Clin. 2015; 11:125–31.
Article28. Laughlin MH, McAllister RM. Exercise training-induced coronary vascular adaptation. J Appl Physiol (1985). 1992; 73:2209–25.
Article29. Loney T, Standage M, Thompson D, Sebire SJ, Cumming S. Self-report vs. objectively assessed physical activity: which is right for public health? J Phys Act Health. 2011; 8:62–70.
Article30. Ko SH, Kim DJ, Park JH, Park CY, Jung CH, Kwon HS, et al. Trends of antidiabetic drug use in adult type 2 diabetes in Korea in 2002-2013: nationwide population-based cohort study. Medicine (Baltimore). 2016; 95:e4018.31. Ko SH, Han K, Lee YH, Noh J, Park CY, Kim DJ, et al. Past and current status of adult type 2 diabetes mellitus management in Korea: a national health insurance service database analysis. Diabetes Metab J. 2018; 42:93–100.
Article32. Kim JY, Kim SJ, Nam CM, Moon KT, Park EC. Changes in prescription pattern, pharmaceutical expenditure and quality of care after introduction of reimbursement restriction in diabetes in Korea. Eur J Public Health. 2018; 28:209–14.
Article33. Chaudhry SI, Wang Y, Concato J, Gill TM, Krumholz HM. Patterns of weight change preceding hospitalization for heart failure. Circulation. 2007; 116:1549–54.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Maintaining Physical Activity Is Associated with Reduced Major Adverse Cardiovascular Events in People Newly Diagnosed with Diabetes
- Heart Failure: Complications of Type 2 Diabetes
- Heart Failure and Diabetes Mellitus: Dangerous Liaisons
- Diabetes Management in Patients with Heart Failure
- A Case of Newly Diagnosed Type 2 Diabetes Mellitus with Daily Headaches