Kosin Med J.
2022 Mar;37(1):75-82. 10.7180/kmj.22.010.
New approach to learning medical procedures using a smartphone and the Moodle platform to facilitate assessments and written feedback
- Affiliations
-
- 1Department of Psychiatry, Kosin University College of Medicine, Busan, Korea
- 2Department of Thoracic and Cardiovascular Surgery, Kosin University College of Medicine, Busan, Korea
- 3Department of Laboratory Medicine, Kosin University College of Medicine, Busan, Korea
- KMID: 2527698
- DOI: http://doi.org/10.7180/kmj.22.010
Abstract
- Background
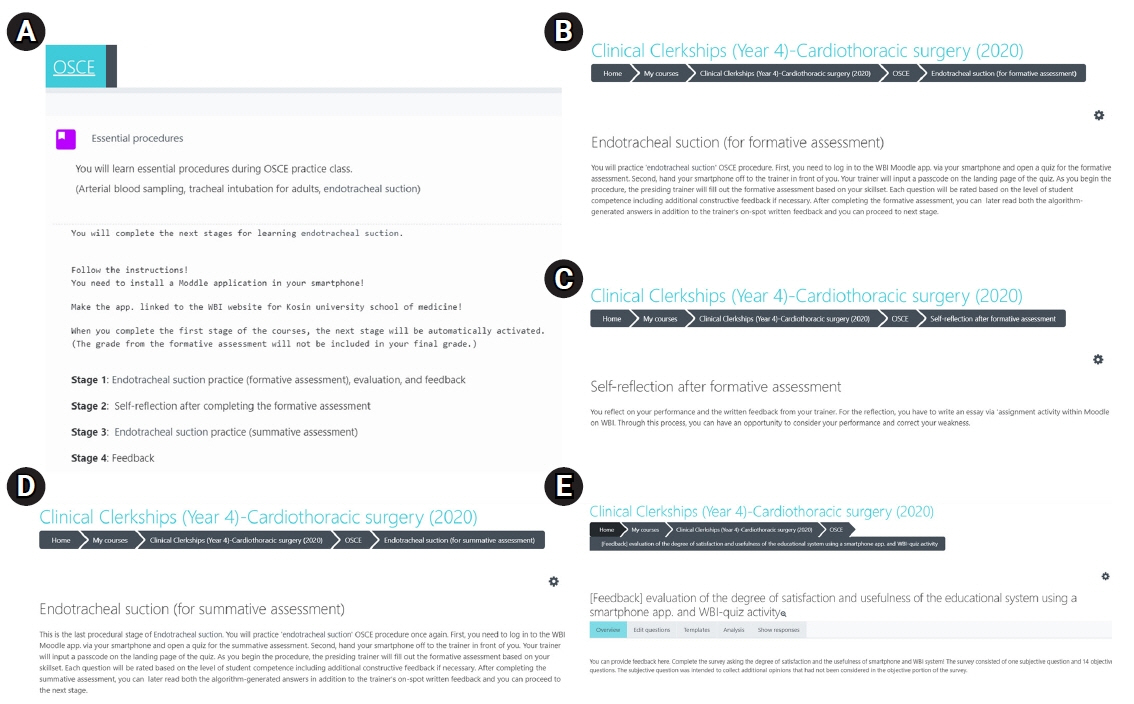
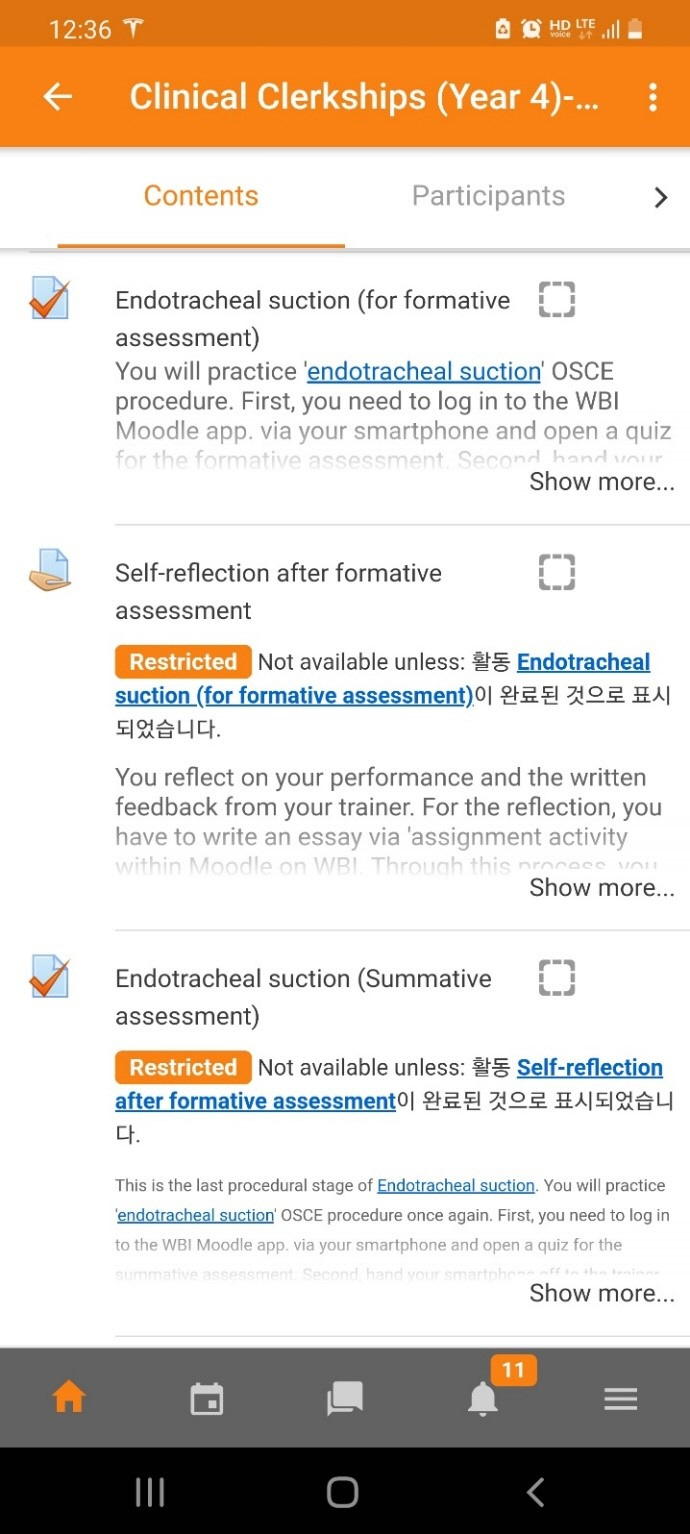
To overcome communication obstacles between medical students and trainers, we designed serial learning activities utilizing a smartphone and web-based instruction (WBI) on the Moodle platform to provide clear and retrievable trainer feedback to students on an objective structured clinical examination (OSCE) item.
Methods
We evaluated students’ learning achievement and satisfaction with the new learning tool. A total of 80 fourth-year medical students participated. They installed the Moodle app (the WBI platform) on their smartphones and practiced an endotracheal suction procedure on a medical simulation mannequin while being evaluated by a trainer regarding competence in clinical skills on the smartphone app. Students’ competency was evaluated by comparing the scores between the formative assessment and the summative assessment. The degree of satisfaction and usefulness for the smartphone and WBI system were analyzed.
Results
The means (standard deviations, SDs) of the formative and summative assessments were 8.80 (2.53) and 14.24 (1.97) out of a total of 17 points, respectively, reflecting a statistically significant difference (P<0.05). The degree of satisfaction and perceived usefulness of the smartphone app and WBI system were excellent, with means (SDs) of 4.60 (0.58), and 4.60 (0.65), respectively.
Conclusion
We believe that the learning process using a smartphone and the Moodle platform offers good guidance for OSCE skill development because trainers’ written feedback is recorded online and is retrievable at all times, enabling students to build and maintain competency through frequent feedback review.
Figure
Cited by 1 articles
-
Do we need Moodle in medical education? A review of its impact and utility
Seri Jeong, Hyunyong Hwang
Kosin Med J. 2023;38(3):159-168. doi: 10.7180/kmj.23.139.
Reference
-
References
1. Fromme HB, Karani R, Downing SM. Direct observation in medical education: a review of the literature and evidence for validity. Mt Sinai J Med. 2009; 76:365–71.
Article2. Holmboe ES, Kogan JR. Observation in medical education: time for a broader conversation? Fam Syst Health. 2018; 36:17–9.
Article3. Johnson CE, Weerasuria MP, Keating JL. Effect of face-to-face verbal feedback compared with no or alternative feedback on the objective workplace task performance of health professionals: a systematic review and meta-analysis. BMJ Open. 2020; 10:e030672.
Article4. Burr SA, Brodier E, Wilkinson S. Delivery and use of individualised feedback in large class medical teaching. BMC Med Educ. 2013; 13:63.
Article5. Ende J. Feedback in clinical medical education. JAMA. 1983; 250:777–81.
Article6. Roediger HL 3rd, Butler AC. The critical role of retrieval practice in long-term retention. Trends Cogn Sci. 2011; 15:20–7.
Article7. Calleja P, Harvey T, Fox A, Carmichael M. Feedback and clinical practice improvement: a tool to assist workplace supervisors and students. Nurse Educ Pract. 2016; 17:167–73.
Article8. Branch WT Jr, Paranjape A. Feedback and reflection: teaching methods for clinical settings. Acad Med. 2002; 77(12 Pt 1):1185–8.9. Hewson MG, Little ML. Giving feedback in medical education: verification of recommended techniques. J Gen Intern Med. 1998; 13:111–6.10. Ference K, Mackesy BL, Reinert P, Foote EF. The Importance of written feedback on the individual and team performance of student pharmacists. Am J Pharm Educ. 2020; 84:ajpe7870.
Article11. Kim JY, Na BJ, Yun J, Kang J, Han S, Hwang W, et al. What kind of feedback do medical students want? Korean J Med Educ. 2014; 26:231–4.
Article12. Chick RC, Clifton GT, Peace KM, Propper BW, Hale DF, Alseidi AA, et al. Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. 2020; 77:729–32.
Article13. Sahi PK, Mishra D, Singh T. Medical education amid the COVID-19 pandemic. Indian Pediatr. 2020; 57:652–7.
Article14. Jamieson S. Likert scales: how to (ab)use them. Med Educ. 2004; 38:1217–8.
Article15. Anderson PA. Giving feedback on clinical skills: are we starving our young? J Grad Med Educ. 2012; 4:154–8.
Article16. Klaber B. Effective feedback: an essential skill. Postgrad Med J. 2012; 88:187–8.
Article17. Lerchenfeldt S, Mi M, Eng M. The utilization of peer feedback during collaborative learning in undergraduate medical education: a systematic review. BMC Med Educ. 2019; 19:321.
Article18. Watling CJ, Ginsburg S. Assessment, feedback and the alchemy of learning. Med Educ. 2019; 53:76–85.
Article19. Popovic N, Popovic T, Rovcanin Dragovic I, Cmiljanic O. A Moodle-based blended learning solution for physiology education in Montenegro: a case study. Adv Physiol Educ. 2018; 42:111–7.
Article20. Seluakumaran K, Jusof FF, Ismail R, Husain R. Integrating an open-source course management system (Moodle) into the teaching of a first-year medical physiology course: a case study. Adv Physiol Educ. 2011; 35:369–77.
Article21. Martínez F, Tobar C, Taramasco C. Implementation of a smartphone application in medical education: a randomised trial (iSTART). BMC Med Educ. 2017; 17:168.
Article22. Payne KB, Wharrad H, Watts K. Smartphone and medical related App use among medical students and junior doctors in the United Kingdom (UK): a regional survey. BMC Med Inform Decis Mak. 2012; 12:121.
Article23. Valle J, Godby T, Paul DP 3rd, Smith H, Coustasse A. Use of smartphones for clinical and medical education. Health Care Manag (Frederick). 2017; 36:293–300.
Article24. Hwang H. A computer-assisted, real-time feedback system for medical students as a tool for web-based learning. Kosin Med J. 2016; 31:134–45.
Article25. Pelgrim EA, Kramer AW, Mokkink HG, van der Vleuten CP. Reflection as a component of formative assessment appears to be instrumental in promoting the use of feedback; an observational study. Med Teach. 2013; 35:772–8.
Article26. Ahmed S, Zimba O, Gasparyan AY. Moving towards online rheumatology education in the era of COVID-19. Clin Rheumatol. 2020; 39:3215–22.
Article27. Seymour-Walsh AE, Bell A, Weber A, Smith T. Adapting to a new reality: COVID-19 coronavirus and online education in the health professions. Rural Remote Health. 2020; 20:6000.
Article28. Singhi EK, Dupuis MM, Ross JA, Rieber AG, Bhadkamkar NA. Medical hematology/oncology fellows’ perceptions of online medical education during the COVID-19 pandemic. J Cancer Educ. 2020; 35:1034–40.
Article29. Gaur U, Majumder MA, Sa B, Sarkar S, Williams A, Singh K. Challenges and opportunities of preclinical medical education: COVID-19 crisis and beyond. SN Compr Clin Med. 2020; 2:1992–7.
Article30. Radu MC, Schnakovszky C, Herghelegiu E, Ciubotariu VA, Cristea I. The impact of the COVID-19 pandemic on the quality of educational process: a student survey. Int J Environ Res Public Health. 2020; 17:7770.
Article31. Kuhn S, Frankenhauser S, Tolks D. Digital learning and teaching in medical education: already there or still at the beginning? Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2018; 61:201–9.32. Dalton CL, Wilson A, Agius S. Twelve tips on how to compile a medical educator’s portfolio. Med Teach. 2018; 40:140–5.
Article33. Heeneman S, Driessen EW. The use of a portfolio in postgraduate medical education: reflect, assess and account, one for each or all in one? GMS J Med Educ. 2017; 34:Doc57.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Do we need Moodle in medical education? A review of its impact and utility
- The effectiveness of Moodle's “Lesson” feature in pre-learning about arterial puncture and blood transfusion procedures
- What steps are necessary to create written or web-based selected-response assessments?
- Discovering social learning ecosystems during clinical clerkship from United States medical students’ feedback encounters: a content analysis
- Relationships between Smartphone Usage, Sleep Patterns and Nursing Students' Learning Engagement