J Korean Med Sci.
2022 Mar;37(12):e97. 10.3346/jkms.2022.37.e97.
New-Onset Seizures in Patients With COVID-19: A Case Series From a Single Public Hospital in Korea
- Affiliations
-
- 1Department of Neurology, National Medical Center, Seoul, Korea
- KMID: 2527638
- DOI: http://doi.org/10.3346/jkms.2022.37.e97
Abstract
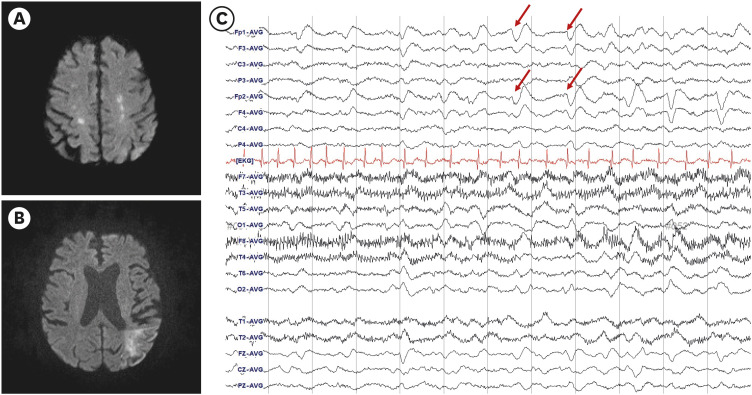
- Seizure is an uncommon complication of coronavirus disease 2019 (COVID-19). The frequency and characteristics of new-onset seizures in hospitalized patients with COVID-19 were investigated. Of a total of 1,487 patients with confirmed COVID-19, six (0.4%) developed new-onset seizures. All six had severe or critical COVID-19 requiring intensive care and mechanical ventilation or high-flow oxygen therapy. Among COVID-19 patients admitted to the intensive care unit (n = 169), the incidence of new-onset seizures was 3.6%. Underlying structural lesions (acute infarction and remote hemorrhage), hypoxia, sepsis, and metabolic derangements were associated with the development of seizures. Of the six patients, three patients died, and, at the time of discharge, one patient had a severe disability, while the remaining two were well recovered.
Keyword
Figure
Reference
-
1. World Health Organization. Living guidance for clinical management of COVID-19. Updated 2021. Accessed December 11, 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2 .2. Misra S, Kolappa K, Prasad M, Radhakrishnan D, Thakur KT, Solomon T, et al. Frequency of neurologic manifestations in COVID-19: a systematic review and meta-analysis. Neurology. 2021; 97(23):e2269–e2281. PMID: 34635561.3. Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020; 77(6):683–690. PMID: 32275288.4. Pizzi MA. Acute neurologic manifestations of respiratory viruses. Continuum (Minneap Minn). 2021; 27(5):1365–1381. PMID: 34618764.5. Frontera JA, Sabadia S, Lalchan R, Fang T, Flusty B, Millar-Vernetti P, et al. A prospective study of neurologic disorders in hospitalized patients with COVID-19 in New York City. Neurology. 2021; 96(4):e575–e586. PMID: 33020166.6. Emami A, Fadakar N, Akbari A, Lotfi M, Farazdaghi M, Javanmardi F, et al. Seizure in patients with COVID-19. Neurol Sci. 2020; 41(11):3057–3061. PMID: 32949289.7. Eskandar EN, Altschul DJ, de la Garza Ramos R, Cezayirli P, Unda SR, Benton J, et al. Neurologic syndromes predict higher in-hospital mortality in COVID-19. Neurology. 2021; 96(11):e1527–e1538. PMID: 33443111.8. Vohora D, Jain S, Tripathi M, Potschka H. COVID-19 and seizures: is there a link? Epilepsia. 2020; 61(9):1840–1853. PMID: 32944929.9. Bhagat R, Kwiecinska B, Smith N, Peters M, Shafer C, Palade A, et al. New-onset seizure with possible limbic encephalitis in a patient with COVID-19 infection: a case report and review. J Investig Med High Impact Case Rep. 2021; 9:2324709620986302.10. Keyhanian K, Umeton RP, Mohit B, Davoudi V, Hajighasemi F, Ghasemi M. SARS-CoV-2 and nervous system: From pathogenesis to clinical manifestation. J Neuroimmunol. 2020; 350:577436. PMID: 33212316.11. Le Guennec L, Devianne J, Jalin L, Cao A, Galanaud D, Navarro V, et al. Orbitofrontal involvement in a neuroCOVID-19 patient. Epilepsia. 2020; 61(8):e90–e94. PMID: 32589794.12. Narula N, Joseph R, Katyal N, Daouk A, Acharya S, Avula A, et al. Seizure and COVID-19: association and review of potential mechanism. Neurol Psychiatry Brain Res. 2020; 38:49–53. PMID: 33071468.13. Matschke J, Lütgehetmann M, Hagel C, Sperhake JP, Schröder AS, Edler C, et al. Neuropathology of patients with COVID-19 in Germany: a post-mortem case series. Lancet Neurol. 2020; 19(11):919–929. PMID: 33031735.14. Lewis A, Frontera J, Placantonakis DG, Lighter J, Galetta S, Balcer L, et al. Cerebrospinal fluid in COVID-19: a systematic review of the literature. J Neurol Sci. 2021; 421:117316. PMID: 33561753.15. Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 2020; 92(6):552–555. PMID: 32104915.16. Yachou Y, El Idrissi A, Belapasov V, Ait Benali S. Neuroinvasion, neurotropic, and neuroinflammatory events of SARS-CoV-2: understanding the neurological manifestations in COVID-19 patients. Neurol Sci. 2020; 41(10):2657–2669. PMID: 32725449.17. Tancheva L, Petralia MC, Miteva S, Dragomanova S, Solak A, Kalfin R, et al. Emerging neurological and psychobiological aspects of COVID-19 infection. Brain Sci. 2020; 10(11):E852. PMID: 33198412.18. Carroll E, Melmed KR, Frontera J, Placantonakis DG, Galetta S, Balcer L, et al. Cerebrospinal fluid findings in patients with seizure in the setting of COVID-19: A review of the literature. Seizure. 2021; 89:99–106. PMID: 34044299.19. Beghi E, Carpio A, Forsgren L, Hesdorffer DC, Malmgren K, Sander JW, et al. Recommendation for a definition of acute symptomatic seizure. Epilepsia. 2010; 51(4):671–675. PMID: 19732133.20. Karceski S.. Acute symptomatic seizures and systemic illness. Continuum (Minneap Minn). 2014; 20(3):614–623. PMID: 24893237.21. Chua TH, Xu Z, King NK. Neurological manifestations in COVID-19: a systematic review and meta-analysis. Brain Inj. 2020; 34(12):1549–1568. PMID: 33074036.22. Anand P, Al-Faraj A, Sader E, Dashkoff J, Abdennadher M, Murugesan R, et al. Seizure as the presenting symptom of COVID-19: a retrospective case series. Epilepsy Behav. 2020; 112:107335. PMID: 32739397.23. Mithani F, Poursheykhi M, Ma B, Smith RG, Hsu SH, Gotur D. New-onset seizures in three COVID-19 patients: a case series. J Clin Neurophysiol. 2021; 38(2):e5–10. PMID: 33315693.24. Pellinen J, Carroll E, Friedman D, Boffa M, Dugan P, Friedman DE, et al. Continuous EEG findings in patients with COVID-19 infection admitted to a New York academic hospital system. Epilepsia. 2020; 61(10):2097–2105. PMID: 32875578.25. Oddo M, Carrera E, Claassen J, Mayer SA, Hirsch LJ. Continuous electroencephalography in the medical intensive care unit. Crit Care Med. 2009; 37(6):2051–2056. PMID: 19384197.26. Gilmore EJ, Gaspard N, Choi HA, Cohen E, Burkart KM, Chong DH, et al. Acute brain failure in severe sepsis: a prospective study in the medical intensive care unit utilizing continuous EEG monitoring. Intensive Care Med. 2015; 41(4):686–694. PMID: 25763756.27. Bleck TP, Smith MC, Pierre-Louis SJ, Jares JJ, Murray J, Hansen CA. Neurologic complications of critical medical illnesses. Crit Care Med. 1993; 21(1):98–103. PMID: 8420739.28. Ferlisi M, Shorvon S. Seizure precipitants (triggering factors) in patients with epilepsy. Epilepsy Behav. 2014; 33:101–105. PMID: 24632482.29. Hepburn M, Mullaguri N, George P, Hantus S, Punia V, Bhimraj A, et al. Acute symptomatic seizures in critically ill patients with COVID-19: is there an association? Neurocrit Care. 2021; 34(1):139–143. PMID: 32462412.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early-Onset Myasthenia Gravis Following COVID-19 Vaccination
- A Hidden Key to COVID-19 Management in Korea: Public Health Doctors
- A Chinese Case of Coronavirus Disease 2019 (COVID-19) Did Not Show Infectivity During the Incubation Period: Based on an Epidemiological Survey
- Coronavirus Disease-19: The First 7,755 Casesin the Republic of Korea
- The Delay in Confirming COVID-19 Cases Linked to a Religious Group in Korea