Clin Endosc.
2022 Mar;55(2):215-225. 10.5946/ce.2021.051.
Perception of Gastrointestinal Endoscopy Personnel on Society Recommendations on Personal Protective Equipment, Case Selection, and Scope Cleaning During Covid-19 Pandemic: An International Survey Study
- Affiliations
-
- 1Division of Gastroenterology, Department of Medicine, Faculty of Medicine, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Thai Red Cross, Bangkok, Thailand
- 2Center of Excellence for Innovation and Endoscopy in Gastrointestinal Oncology, Chulalongkorn University, Bangkok, Thailand
- 3Division of Radiology, Jinnah Hospital, Lahore, Pakistan
- 4Division of Gastroenterology, Lahore General Hospital, Lahore, Pakistan
- 5Division of Digestive Diseases, Department of Internal Medicine, Emory University, Atlanta, GA, USA
- 6Gastroenterology and Hepatology Unit, Department of Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia
- 7Department of Surgery, Rajavithi Hospital, Bangkok, Thailand
- 8Division of Gastroenterology, Department of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand
- KMID: 2527565
- DOI: http://doi.org/10.5946/ce.2021.051
Abstract
- Background/Aims
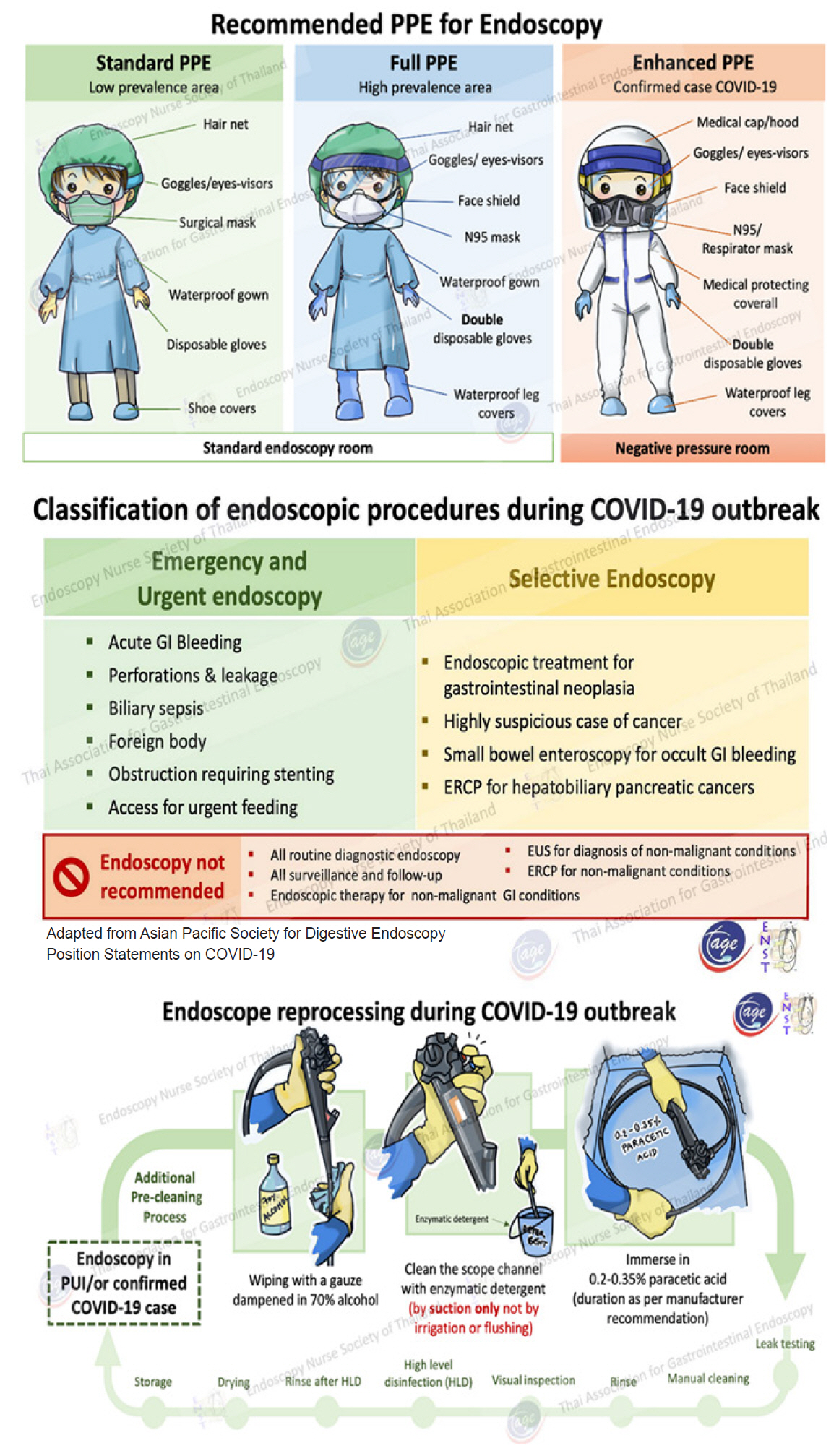
The Thai Association for Gastrointestinal Endoscopy published recommendations on safe endoscopy during the coronavirus disease 2019 (COVID-19) pandemic. This study aimed to assess the practicality and applicability of the recommendations and the perceptions of endoscopy personnel on them.
Methods
A validated questionnaire was sent to 1290 endoscopy personnel globally. Of these, the data of all 330 responders (25.6%) from 15 countries, related to the current recommendations on proper personal protective equipment (PPE), case selection, scope cleaning, and safety perception, were analyzed. Ordinal logistic regression was used to determine the relationships between the variables.
Results
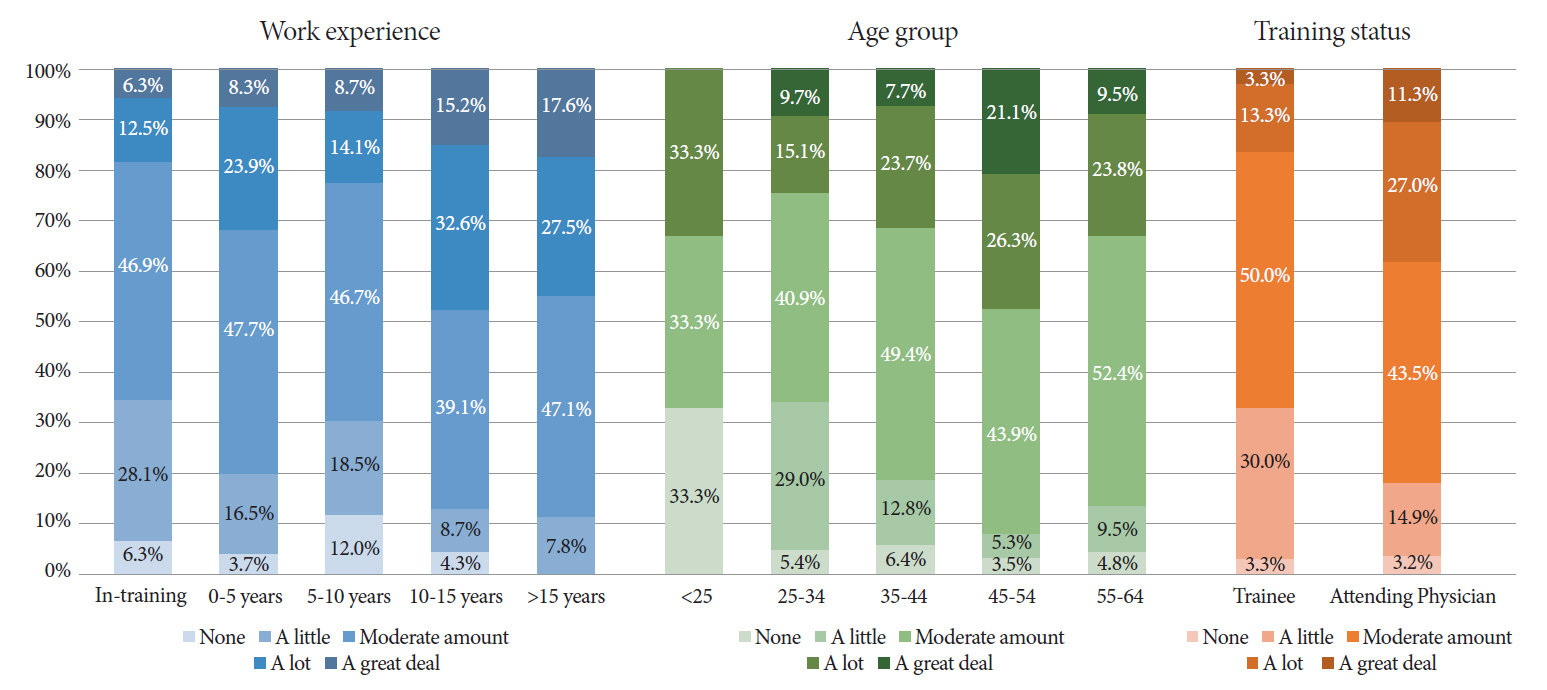
Despite an overwhelming agreement with the recommendations on PPE (94.5%) and case selection (95.5%), their practicality and applicability on PPE recommendations and case selection were significantly lower (p=0.001, p=0.047, p<0.001, and p=0.032, respectively). Factors that were associated with lower sense of safety in endoscopy units were younger age (p=0.004), less working experience (p=0.008), in-training status (p=0.04), and higher national prevalence of COVID-19 (p=0.003). High prevalent countries also had more difficulty implementing the guidelines (p<0.001) and they considered the PPE recommendations less practical and showed lower agreement with them (p<0.001 and p=0.008, respectively). A higher number of in-hospital COVID-19 patients was associated with less agreement with PPE recommendations (p=0.039).
Conclusions
Using appropriate PPE and case selection in endoscopic practice during a pandemic remains a challenge. Resource availability and local prevalence are critical factors influencing the adoption of the current guidelines.
Keyword
Figure
Reference
-
1. Bai Y, Yao L, Wei T, et al. Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA. 2020; 323:1406–1407.2. Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science. 2020; 368:489–493.3. Gu J, Han B, Wang J. COVID-19: Gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020; 158:1518–1519.4. Song Y, Liu P, Shi XL, et al. SARS-CoV-2 induced diarrhoea as onset symptom in patient with COVID-19. Gut. 2020; 69:1143–1144.5. Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020; 158:1831–1833.e3.6. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020; 382:1564–1567.7. Chiu PWY, Ng SC, Inoue H, et al. Practice of endoscopy during COVID-19 pandemic: position statements of the Asian Pacific Society for Digestive Endoscopy (APSDE-COVID statements). Gut. 2020; 69:991–996.8. Soetikno R, Teoh AYB, Kaltenbach T, et al. Considerations in performing endoscopy during the COVID-19 pandemic. Gastrointest Endosc. 2020; 92:176–183.9. Chapman S. Hot air? BMJ. 2001; 323:1449.10. Johnston ER, Habib-Bein N, Dueker JM, et al. Risk of bacterial exposure to the endoscopist’s face during endoscopy. Gastrointest Endosc. 2019; 89:818–824.11. Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012; 7:e35797.12. American Society for Gastrointestinal Endoscopy. JOINT GI SOCIETY MESSAGE: COVID-19 clinical insights for our community of gastroenterologists and gastroenterology care providers [Internet]. Downers Grove (IL): ASGE;c2020. [cited Apr 21, 2021]. Available from: https://www.asge.org/home/joint-gi-society-message-covid-19.13. Kongkam P, Tiankanon K, Ratanalert S, et al. The practice of endoscopy during the COVID-19 pandemic: recommendations from the Thai association for gastrointestinal endoscopy (TAGE) in collaboration with the endoscopy nurse society (Thailand). Siriraj Medical Journal. 2020; 72.14. Philip M, Lakhtakia S, Aggarwal R, Madan K, Saraswat V, Makharia G. Joint guidance from SGEI, ISG and INASL for gastroenterologists and gastrointestinal endoscopists on the prevention, care, and management of patients with COVID-19. J Clin Exp Hepatol. 2020; 10:266–270.15. Repici A, Maselli R, Colombo M, et al. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc. 2020; 92:192–197.16. Pryor A. SAGES and EAES Recommendations Regarding Surgical Response to COVID-19 Crisis [Internet]. Los Angeles, (CA): SAGES;c2020. [cited 2021 Apr 21]. Available from: https://www.sages.org/recommendations-surgical-response-covid-19/.17. Rerknimitr R, Soetikno R, Ratanachu-Ek T, Tiankanon K, Kongkam P, Ridtitid W. Additional measures for bedside endoscope cleaning to prevent contaminated splash during COVID-19 pandemic. Endoscopy. 2020; 52:706–707.18. WHO Coronavirus (COVID-19) Dashboard [Internet]. Geneva: WHO;c2020. [cited 2021 June 2]. Available from: https://covid19.who.int/.19. Barlett JE, Kotrlik J, Higgins C. Organizational research: determining appropriate sample size in survey research. Information Technology, Learning, and Performance Journal. 2001; 19.20. World Health Organization. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages: interim guidance, 6 April 2020 [Internet]. Geneva: WHO;c2020. [cited 2021 Apr 21]. Available from: https://apps.who.int/iris/handle/10665/331695.21. National Center for Immunization and Respiratory Diseases. Centers for disease control and prevention [Internet]. Atlanta (GA): CDC;c2020. [updated 2020 Jul 16; cited 2021 Apr 21]. Available frrom: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/index.html.22. BBC. Coronavirus: Medics to be asked to reuse gowns amid shortage fears. [Internet]. London: BBC NEWS;c2020. [updated 2020 Apr 17; cited 2021 Apr 21]. Available from: https://www.bbc.com/news/uk52333157.23. CNN. Doctors and nurses alarmed about lack of supplies [Internet]. Atlanta (GA): CNN;c2020. [updated 2020 Mar 27; cited Apr 21 2021]. Available from: https://edition.cnn.com/videos/health/2020/03/27/medical-workers-shortage-of-protective-equipment-griffin-dnt-vpx.cnn.24. CNN. Faced with shortages, hospitals and companies work to extend use of N95 masks [Internet]. Atlanta (GA): CNN;c2020. [updated Apr 10; cited Apr 21 2021]. Available from: https://edition.cnn.com/2020/04/10/politics/n95-masks-coronavirus-pandemic/index.html.25. Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients. J Infect. 2020; 80:e14–e8.26. Martin SD, Bush AC, Lynch JA. A national survey of terrorism preparedness training among pediatric, family practice, and emergency medicine programs. Pediatrics. 2006; 118:e620–e626.27. Niska RW, Burt CW. Bioterrorism and mass casualty preparedness in hospitals: United States, 2003. Adv Data. 2005; 1–14.28. World Health Organization. COVID-19: operational guidance for maintaining essential health services during an outbreak: interim guidance, 25 March 2020. Geneva: WHO;c2020. [cited 2021 Apr 21]; Available at: https://apps.who.int/iris/handle/10665/331561.29. Becker B, Brill FHH, Todt D, et al. Virucidal efficacy of peracetic acid for instrument disinfection. Antimicrob Resist Infect Control. 2017; 6:114.30. Costa D de M, Lopes LK de O, Hu H, Tipple AFV, Vickery K. Alcohol fixation of bacteria to surgical instruments increases cleaning difficulty and may contribute to sterilization inefficacy. Am J Infect Control. 2017; 45:e81–e86.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Personal Protective Equipment for Healthcare Workers during the COVID-19 Pandemic
- Laryngoscopy During the COVID-19 Pandemic
- Clinical Gastroenterology and Gastrointestinal Endoscopy Practices during the Coronavirus Disease 2019 Pandemic in Indonesia: An Online Nationwide Survey
- Assessment and Management of Dysphagia during the COVID-19 Pandemic
- How to Cope with COVID-19 in the Endoscopy Room