Korean J Gastroenterol.
2022 Mar;79(3):109-117. 10.4166/kjg.2021.149.
Comparison between Wound Closure Methods in the Reversal of Diverting Ileostomy
- Affiliations
-
- 1Department of Colorectal Surgery, Presbyterian Medical Center, Jeonju, Korea
- 2Department of Surgery, Chungnam National University Hospital, Daejeon, Korea
- KMID: 2527478
- DOI: http://doi.org/10.4166/kjg.2021.149
Abstract
- Background/Aims
The objective of this study was to determine the more appropriate wound-closure method by comparing the effectiveness of two methods in a group of patients who underwent ileostomy repair.
Methods
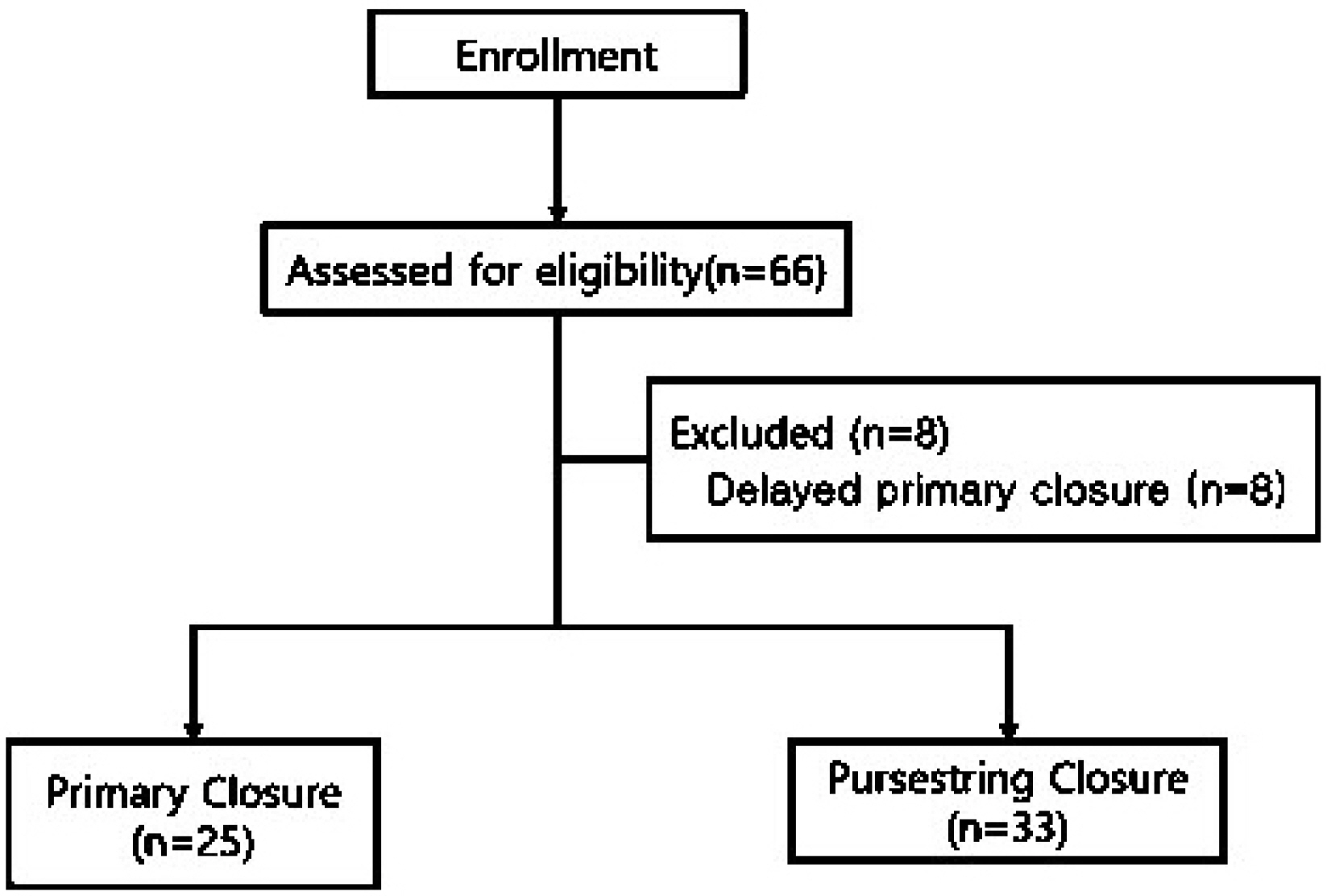
The study conducted after obtaining the approval of the Institutional Review Board (IRB) included 58 patients ≥19 years of age who underwent ileostomy at the Department of Surgery at the Presbyterian Medical Center. This was a retrospective, single-center trial. Patients who underwent ileostomy closure between January 2011 and September 2017 were assigned to the primary wound-closure (PC, n=25) group and the purse-string wound-closure (PSC, n=33) group. Post-repair complications, such as wound infection, delayed healing, and patient satisfaction related to wound management, were investigated and compared according to the wound-closure method.
Results
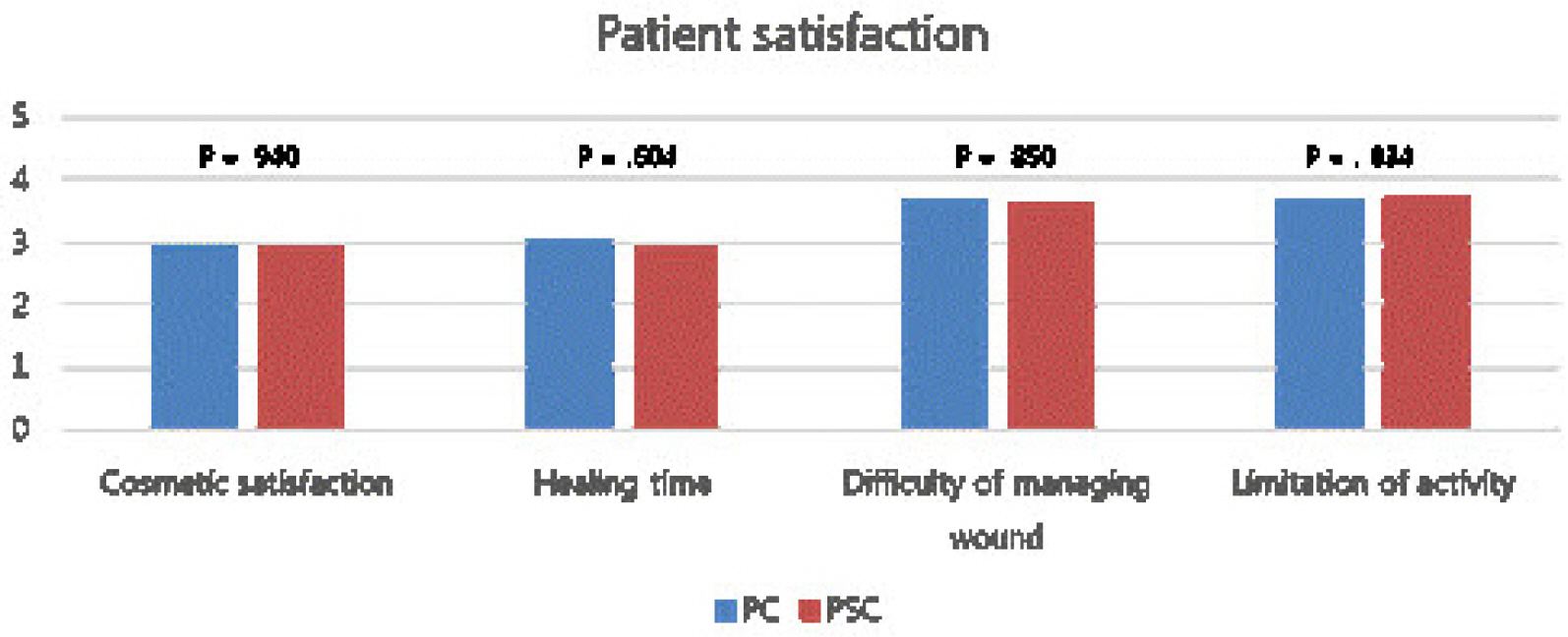
The PSC group had a significantly lower surgical site infection rate than the PC group (0% vs. 44%, p<0.001). The wound-healing period was also significantly different between the PC and PSC groups (mean 27.18 days vs. 20.96 days, p=0.023). However, the postoperative wound-healing delay of >30 days was not significantly different (39% vs. 20%, p=0.114). In addition, there were no significant differences in the response to questionnaires on patient satisfaction between the two groups.
Conclusions
PSC has a lower surgical site infection rate and the wound-healing delay was not very different from that of PC. Therefore, if patients are at risk of wound infection, such as in severe wound contamination, long operating time, and immunocompromised conditions, we should consider PSC as a wound closure method of choice.
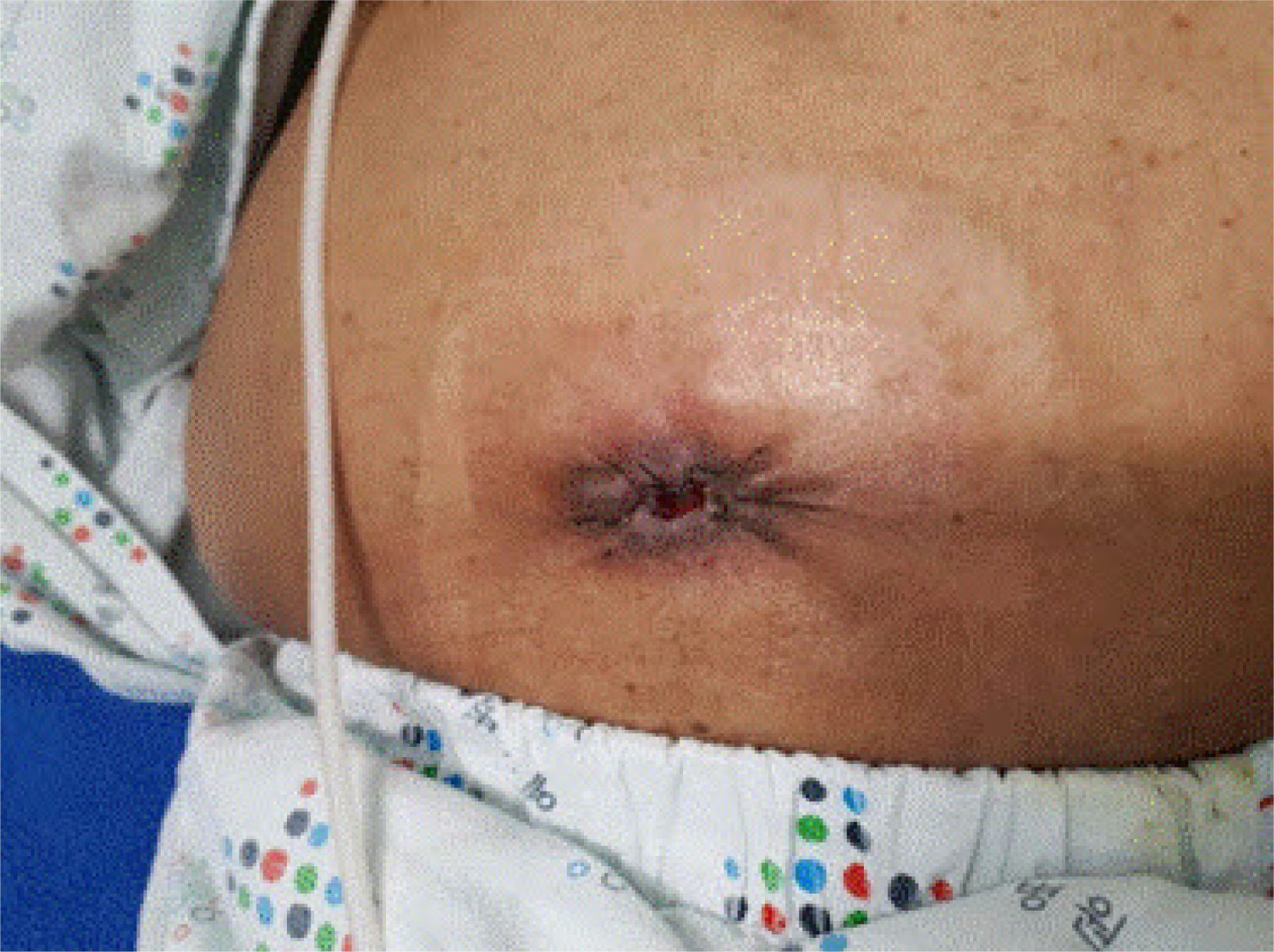
Figure
Reference
-
1. Song GW, Yu CS, Lee HO, et al. 2003; Ileostomy related complications. J Korean Soc Coloproctol. 19:82–89. DOI: 10.1245/s10434-013-3287-9,. PMID: 24085329. PMCID: PMC4026258.2. Kim HY, Kim IY, Kim SH, Yoon KS. 1997; Evaluation of the usefulness of loop ileostomy during low anterior resection or. J Korean Soc Coloproctol. 13:397–402.3. Cipe G, Erkek B, Kuzu A, Gecim E. 2012; Morbidity and mortality after the closure of a protective loop ileostomy: analysis of possible predictors. Hepatogastroenterology. 59:2168–2172. DOI: 10.5754/hge12115. PMID: 22440245.
Article4. Phang PT, Hain JM, Perez-Ramirez JJ, Madoff RD, Gemlo BT. 1999; Techniques and complications of ileostomy takedown. Am J Surg. 177:463–466. DOI: 10.1016/S0002-9610(99)00091-4. PMID: 10414694.
Article5. Hsieh MC, Kuo LT, Chi CC, Huang WS, Chin CC. 2015; Pursestring closure versus conventional primary closure following stoma reversal to reduce surgical site infection rate: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 58:808–815. DOI: 10.1097/DCR.0000000000000401. PMID: 26163961.
Article6. Lee JT, Marquez TT, Clerc D, et al. 2014; Pursestring closure of the stoma site leads to fewer wound infections: results from a multicenter randomized controlled trial. Dis Colon Rectum. 57:1282–1289. DOI: 10.1097/DCR.0000000000000209. PMID: 25285695.7. Camacho-Mauries D, Rodriguez-Díaz JL, Salgado-Nesme N, González QH, Vergara-Fernández O. 2013; Randomized clinical trial of intestinal ostomy takedown comparing pursestring wound closure vs conventional closure to eliminate the risk of wound infection. Dis Colon Rectum. 56:205–211. DOI: 10.1097/DCR.0b013e31827888f6. PMID: 23303149.
Article8. Lee DH, Yun JA, Jung KU, et al. 2012; Comparison of morbidity between preventive and therapeutic ileostomy repair. Korean J Clin Oncol. 8:44–49. DOI: 10.14216/kjco.12006.
Article9. Williams LA, Sagar PM, Finan PJ, Burke D. 2008; The outcome of loop ileostomy closure: a prospective study. Colorectal Dis. 10:460–464. DOI: 10.1111/j.1463-1318.2007.01385.x. PMID: 17953706.
Article10. El-Hussuna A, Lauritsen M, Bülow S. 2012; Relatively high incidence of complications after loop ileostomy reversal. Dan Med J. 59:A4517. PMID: 23158893.11. Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E, Purkayastha S. 2009; The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis. 24:711–723. DOI: 10.1007/s00384-009-0660-z. PMID: 19221766.
Article12. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. 1999; Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 27:97–96. DOI: 10.1016/S0196-6553(99)70088-X. PMID: 10196487.13. Perez RO, Habr-Gama A, Seid VE, et al. 2006; Loop ileostomy morbidity: timing of closure matters. Dis Colon Rectum. 49:1539–1545. DOI: 10.1007/s10350-006-0645-8. PMID: 16897328.
Article14. Banerjee A. 1997; Pursestring skin closure after stoma reversal. Dis Colon Rectum. 40:993–994. DOI: 10.1007/BF02051210. PMID: 9269819.
Article15. Li LT, Hicks SC, Davila JA, et al. 2014; Circular closure is associated with the lowest rate of surgical site infection following stoma reversal: a systematic review and multiple treatment meta-analysis. Colorectal Dis. 16:406–416. DOI: 10.1111/codi.12556. PMID: 24422861.
Article16. Reid K, Pockney P, Pollitt T, Draganic B, Smith SR. 2010; Randomized clinical trial of short-term outcomes following purse-string versus conventional closure of ileostomy wounds. Br J Surg. 97:1511–1517. DOI: 10.1002/bjs.7151. PMID: 20575111.
Article17. Sutton CD, Williams N, Marshall LJ, Lloyd G, Thomas WM. 2002; A technique for wound closure that minimizes sepsis after stoma closure. ANZ J Surg. 72:766–767. DOI: 10.1046/j.1445-2197.2002.02514.x. PMID: 12534395.
Article18. McCartan DP, Burke JP, Walsh SR, Coffey JC. 2013; Purse-string approximation is superior to primary skin closure following stoma reversal: a systematic review and meta-analysis. Tech Coloproctol. 17:345–351. DOI: 10.1007/s10151-012-0970-y. PMID: 23354904.
Article19. Mirbagheri N, Dark J, Skinner S. 2013; Factors predicting stomal wound closure infection rates. Tech Coloproctol. 17:215–220. DOI: 10.1007/s10151-012-0908-4. PMID: 23076288.
Article20. Harold DM, Johnson EK, Rizzo JA, Steele SR. 2010; Primary closure of stoma site wounds after ostomy takedown. Am J Surg. 199:621–624. DOI: 10.1016/j.amjsurg.2010.01.008. PMID: 20466105.
Article21. Lahat G, Tulchinsky H, Goldman G, Klauzner JM, Rabau M. 2005; Wound infection after ileostomy closure: a prospective randomized study comparing primary vs. delayed primary closure techniques. Tech Coloproctol. 9:206–208. DOI: 10.1007/s10151-005-0228-z. PMID: 16328128.
Article22. Townsend CM, Beauchamp RD, Evers BM. 2016. Sabiston textbook of surgery. 20th ed. Elsevier;Amsterdam:23. Haase O, Raue W, Böhm B, Neuss H, Scharfenberg M, Schwenk W. 2005; Subcutaneous gentamycin implant to reduce wound infections after loop-ileostomy closure: a randomized, double-blind, placebo-controlled trial. Dis Colon Rectum. 48:2025–2031. DOI: 10.1007/s10350-005-0164-z. PMID: 16228839.
Article24. Milanchi S, Nasseri Y, Kidner T, Fleshner P. 2009; Wound infection after ileostomy closure can be eliminated by circumferential subcuticular wound approximation. Dis Colon Rectum. 52:469–474. DOI: 10.1007/DCR.0b013e31819acc90. PMID: 19333048.
Article25. Murray BW, Cipher DJ, Pham T, Anthony T. 2011; The impact of surgical site infection on the development of incisional hernia and small bowel obstruction in colorectal surgery. Am J Surg. 202:558–560. DOI: 10.1016/j.amjsurg.2011.06.014. PMID: 21924402.
Article26. Chapel JM, Ritchey MD, Zhang D, Wang G. 2017; Prevalence and medical costs of chronic diseases among adult medicaid beneficiaries. Am J Prev Med. 53:S143–S154. DOI: 10.1016/j.amepre.2017.07.019. PMID: 29153115. PMCID: PMC5798200.
Article27. Lataillade L, Chabal L. 2021; Therapeutic patient education: a multifaceted approach to ostomy care. Adv Skin Wound Care. 34:36–42. DOI: 10.1097/01.ASW.0000722756.35017.02. PMID: 33323801.
Article28. Keating J, Kelly EW, Hunt I. 2003; Save the skin and improve the scar: a simple technique to minimize the scar from a temporary stoma. Dis Colon Rectum. 46:1428–1429. DOI: 10.1007/s10350-004-6763-2. PMID: 14530688.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Conventional Linear versus Purse-string Skin Closure after Loop Ileostomy Reversal: Comparison of Wound Infection Rates and Operative Outcomes
- Predictors of Fecal Incontinence and Related Quality of Life After a Total Mesorectal Excision With Primary Anastomosis for Patients With Rectal Cancer
- Effects of anchoring sutures at diverting ileostomy after rectal cancer surgery on peritoneal adhesion at following ileostomy reversal
- Feasibility and Safety of a Fold-Over Diverting Ileostomy Reversal After Rectal Cancer Surgery: Case-Matched Comparison to the Resection Technique
- Fortune of temporary ileostomies in patients treated with laparoscopic low anterior resection for rectal cancer