Obstet Gynecol Sci.
2022 Mar;65(2):133-144. 10.5468/ogs.21345.
Preemptive pregabalin for postoperative analgesia during minimally invasive hysterectomy: a systematic review and meta-analysis of randomized controlled trials
- Affiliations
-
- 1Department of Obstetrics and Gynecology, College of Medicine, Alfaisal University, Riyadh, Saudi Arabia
- 2Department of Obstetrics and Gynecology, College of Graduate Health Sciences, University of Tennessee Health Science Center, Memphis, TN, USA
- 3Department of Obstetrics and Gynecology, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia
- 4Department of Obstetrics and Gynecology, King Faisal Specialist Hospital and Research Center, Jeddah, Saudi Arabia
- 5Department of Obstetrics and Gynecology, College of Medicine, Prince Sattam Bin Abdulaziz University, AlKharj, Saudi Arabia
- KMID: 2527265
- DOI: http://doi.org/10.5468/ogs.21345
Abstract
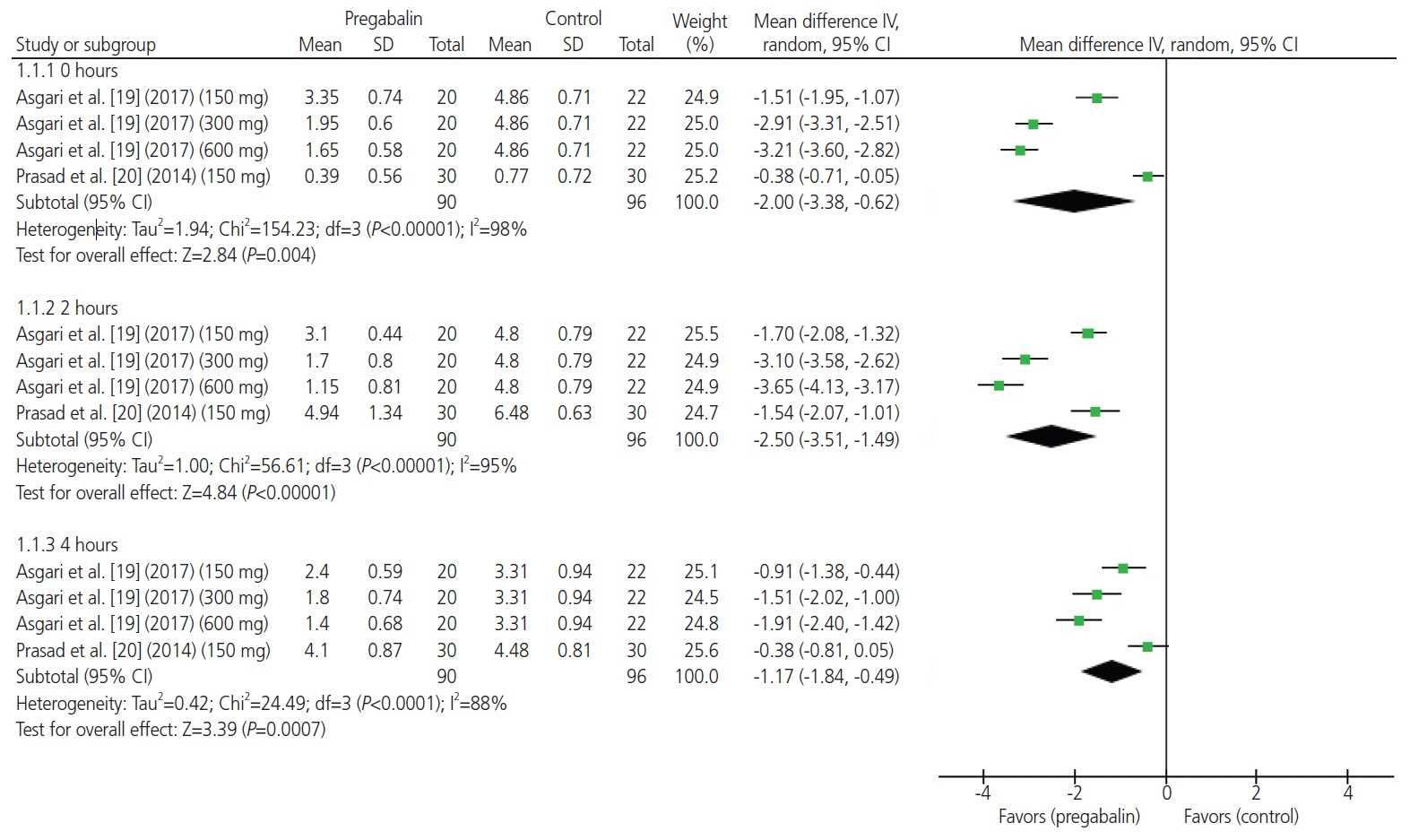
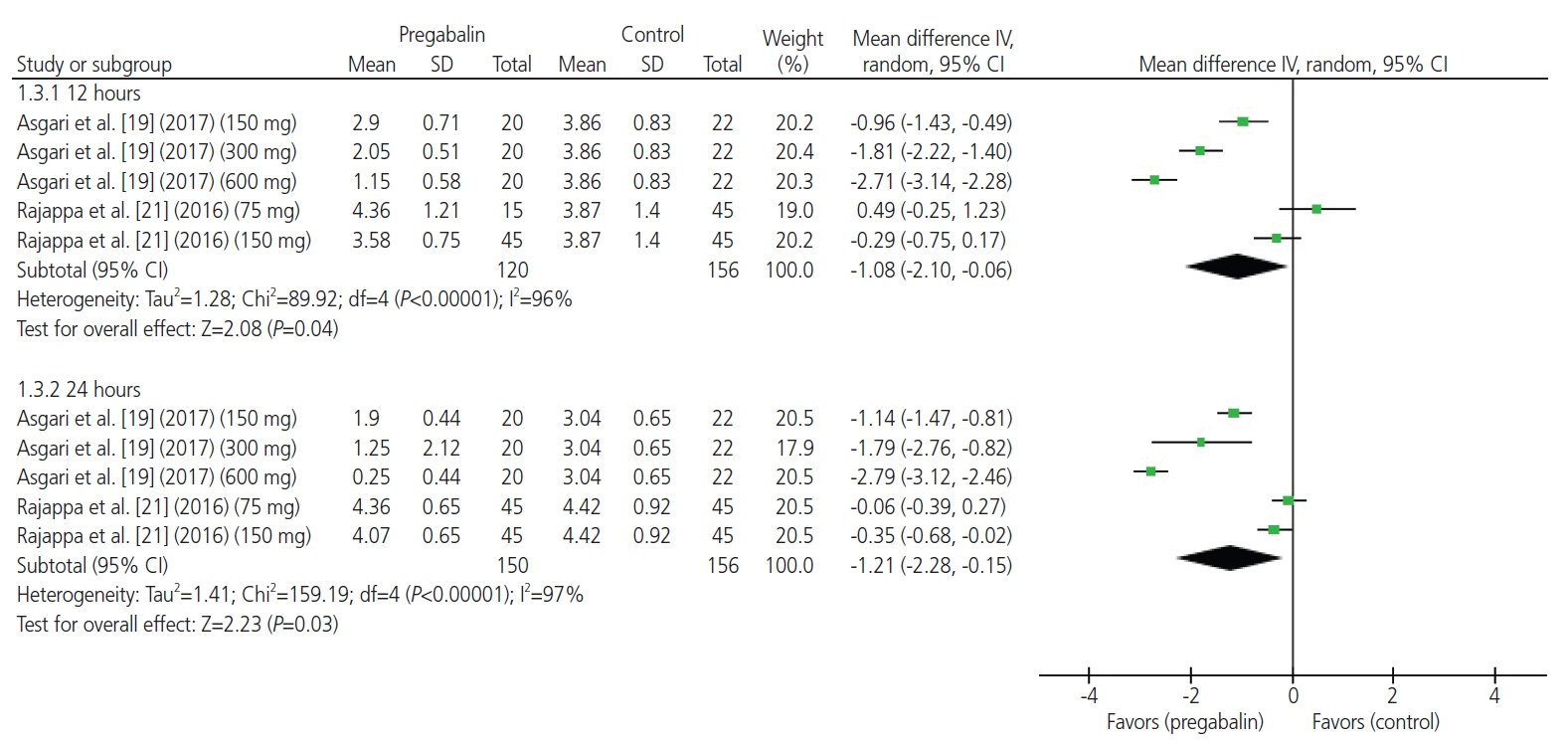
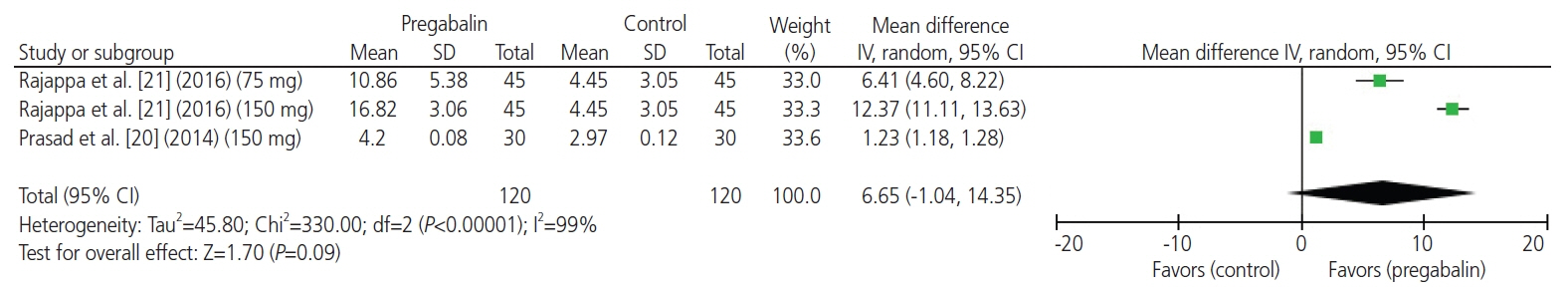
- We aimed to perform a systematic review and meta-analysis of all randomized placebo-controlled trials (RCTs) that examined the analgesic benefits of preemptive pregabalin among patients undergoing minimally invasive hysterectomy. Five major databases were systematically screened from inception until August 29, 2021 Relevant studies were evaluated for risk of bias. Endpoints were analyzed using the random-effects model and pooled as the mean difference or risk ratio with a 95% confidence interval. Four studies with seven treatment arms met the inclusion criteria. The total sample size was 304 patients: 193 and 111 patients were allocated to the pregabalin and placebo groups, respectively. Overall, the included studies revealed a low risk of bias. The summary results revealed that the mean postoperative pain scores at rest were significantly lower in the pregabalin group than in the control group at 0, 2, 4, 6, 12, and 24 hours. Moreover, the mean postoperative pain scores on movement/coughing were significantly lower in the pregabalin group than in the control group at 12 and 24 hours. The rate of patients who were opioid-free postoperatively was significantly higher in the pregabalin group than in the control group. There was no significant difference between the groups in terms of the mean postoperative time to first rescue analgesic and the rates of adverse events. Compared with placebo, preemptive pregabalin was largely safe, and was correlated with superior analgesic effects in terms of lower postoperative pain scores and higher opioid-sparing effects. Additional RCTs are needed to confirm these findings.
Keyword
Figure
Reference
-
References
1. Committee Opinion No 701: choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2017; 129:e155–9.2. Johnson N, Barlow D, Lethaby A, Tavender E, Curr L, Garry R. Methods of hysterectomy: systematic review and meta-analysis of randomised controlled trials. BMJ. 2005; 330:1478.
Article3. O’Neill M, Moran PS, Teljeur C, O’Sullivan OE, O’Reilly BA, Hewitt M, et al. Robot-assisted hysterectomy compared to open and laparoscopic approaches: systematic review and meta-analysis. Arch Gynecol Obstet. 2013; 287:907–18.
Article4. Tulandi T, Krishnamurthy S, Mansour F, Suarthana E, Al-Malki G, Ballesteros LER, et al. A triple-blind randomized trial of preemptive use of gabapentin before laparoscopic hysterectomy for benign gynaecologic conditions. J Obstet Gynaecol Can. 2019; 41:1282–8.
Article5. Benton A, Harkins G, Stetter C, Kunselman A, Deimling T, Riley K. Administration of preoperative gabapentin to patients undergoing laparoscopy: a double-blinded, placebo-controlled randomized trial. J Gynecol Surg. 2020; 36:173–8.
Article6. As-Sanie S, Till SR, Mowers EL, Lim CS, Skinner BD, Fritsch L, et al. Opioid prescribing patterns, patient use, and postoperative pain after hysterectomy for benign indications. Obstet Gynecol. 2017; 130:1261–8.
Article7. Weston E, Raker C, Huang D, Parker A, Cohen M, Robison K, et al. Opioid use after minimally invasive hysterectomy in gynecologic oncology patients. Gynecol Oncol. 2019; 155:119–25.
Article8. Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, Sehgal N, et al. Opioid complications and side effects. Pain Physician. 2008; 11(2 Suppl):S105–20.
Article9. Sills GJ. The mechanisms of action of gabapentin and pregabalin. Curr Opin Pharmacol. 2006; 6:108–13.
Article10. Bockbrader HN, Wesche D, Miller R, Chapel S, Janiczek N, Burger P. A comparison of the pharmacokinetics and pharmacodynamics of pregabalin and gabapentin. Clin Pharmacokinet. 2010; 49:661–9.
Article11. Calandre EP, Rico-Villademoros F, Slim M. Alpha2delta ligands, gabapentin, pregabalin and mirogabalin: a review of their clinical pharmacology and therapeutic use. Expert Rev Neurother. 2016; 16:1263–77.
Article12. Dauri M, Faria S, Gatti A, Celidonio L, Carpenedo R, Sabato AF. Gabapentin and pregabalin for the acute postoperative pain management. A systematic-narrative review of the recent clinical evidences. Curr Drug Targets. 2009; 10:716–33.
Article13. Clarke H, Bonin RP, Orser BA, Englesakis M, Wijeysundera DN, Katz J. The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. Anesth Analg. 2012; 115:428–42.14. Chang CC, Yen WT, Lin YT, Wang LK, Hung KC, Wu ZF, et al. Perioperative pregabalin for preventive analgesia in breast cancer surgery: a meta-analysis of randomized controlled trials. Clin J Pain. 2020; 36:968–77.15. Hannon CP, Fillingham YA, Browne JA, Schemitsch EH, Mullen K, Casambre F, et al. The efficacy and safety of gabapentinoids in total joint arthroplasty: systematic review and direct meta-analysis. J Arthroplasty. 2020; 35:2730–8e6.
Article16. Yu Y, Liu N, Zeng Q, Duan J, Bao Q, Lei M, et al. The efficacy of pregabalin for the management of acute and chronic postoperative pain in thoracotomy: a meta-analysis with trial sequential analysis of randomized-controlled trials. J Pain Res. 2018; 12:159–70.
Article17. Wang SL, Wang H, Nie HY, Bu G, Shen XD, Wang H. The efficacy of pregabalin for acute pain control in herpetic neuralgia patients: a meta-analysis. Medicine (Baltimore). 2017; 96:e9167.18. Ni J, Jiang J, Mao S, Sun RF. Pregabalin does not decrease acute pain or postoperative nausea and vomiting after hysterectomy: a meta-analysis. J Int Med Res. 2020; 48:300060520954720.
Article19. Asgari Z, Rouholamin S, Nataj M, Sepidarkish M, Hosseini R, Razavi M. Dose ranging effects of pregabalin on pain in patients undergoing laparoscopic hysterectomy: a randomized, double blinded, placebo controlled, clinical trial. J Clin Anesth. 2017; 38:13–7.
Article20. Prasad A, Bhattacharyya S, Biswas A, Saha M, Mondal S, Saha D. A comparative study of pre-operative oral clonidine and pregabalin on post-operative analgesia after spinal anesthesia. Anesth Essays Res. 2014; 8:41–7.
Article21. Rajappa GC, Vig S, Bevanaguddaiah Y, Anadaswamy TC. Efficacy of pregabalin as premedication for post-operative analgesia in vaginal hysterectomy. Anesth Pain Med. 2016; 6:e34591.
Article22. Sanguanwongthong K, Imruetaicharoenchok A, Phaloprakarn C, Vitayaburananont P. A randomized, double-blind, placebo-controlled trial of pre-emptive pregabalin for postoperative pain after laparoscopic hysterectomy in benign gynecologic diseases. J Med Assoc Thai. 2019; 102:39.23. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6:e1000097.
Article24. Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane handbook for systematic reviews of interventions version 5.1.0 [Internet]. London (UK): The Cochrane Collaboration;c2021. [cited 2011 Sep 4]. Available from: www.handbook.cochrane.org .25. Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974; 2:656–9.
Article26. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928.
Article27. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–60.
Article28. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–34.
Article29. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014; 14:135.
Article30. Kutbi EH, Sohouli MH, Fatahi S, Lari A, Shidfar F, Aljhdali MM, et al. The beneficial effects of cinnamon among patients with metabolic diseases: a systematic review and dose-response meta-analysis of randomized-controlled trials. Crit Rev Food Sci Nutr. 2021. Mar. 19. [Epub]. https://doi.org/10.1080/10408398.2021.1896473 .
Article31. Abu-Zaid A, Altowairqi AK, Dissanayaka T, Oganesyan A, Bhagavathul AS, Alhabeeb H, et al. A systematic review and dose-response meta-analysis on the efficacy of dapagliflozin in patients with type 1 diabetes mellitus. Pharmacol Res. 2021; 165:105456.
Article32. Gottschalk A, Smith DS. New concepts in acute pain therapy: preemptive analgesia. Am Fam Physician. 2001; 63:1979–84.33. Zhang D, You G, Yao X. Influence of pregabalin on postoperative pain after laparoscopic cholecystectomy: a meta-analysis of randomised controlled trials. J Minim Access Surg. 2019; 16:99–105.
Article34. Blanton E, Lamvu G, Patanwala I, Barron KI, Witzeman K, Tu FF, et al. Non-opioid pain management in benign minimally invasive hysterectomy: a systematic review. Am J Obstet Gynecol. 2017; 216:557–67.
Article35. Myles PS, Myles DB, Galagher W, Boyd D, Chew C, MacDonald N, et al. Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth. 2017; 118:424–9.
Article36. Hu J, Huang D, Li M, Wu C, Zhang J. Effects of a single dose of preoperative pregabalin and gabapentin for acute postoperative pain: a network meta-analysis of randomized controlled trials. J Pain Res. 2018; 11:2633–43.
Article37. White PF, Tufanogullari B, Taylor J, Klein K. The effect of pregabalin on preoperative anxiety and sedation levels: a dose-ranging study. Anesth Analg. 2009; 108:1140–5.
Article38. Li XD, Han C, Yu WL. Is gabapentin effective and safe in open hysterectomy? A PRISMA compliant meta-analysis of randomized controlled trials. J Clin Anesth. 2017; 41:76–83.
Article39. Noor N, Roy KK, Zangmo R, Das A, Rai R, Kumari A, et al. Role of para-cervical block in reducing immediate postoperative pain after total laparoscopic hysterectomy: a prospective randomized placebo-controlled trial. Obstet Gynecol Sci. 2021; 64:122–9.
Article40. Terrin N, Schmid CH, Lau J. In an empirical evaluation of the funnel plot, researchers could not visually identify publication bias. J Clin Epidemiol. 2005; 58:894–901.
Article41. Lau J, Ioannidis JP, Terrin N, Schmid CH, Olkin I. The case of the misleading funnel plot. BMJ. 2006; 333:597–600.
Article42. Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000; 53:1119–29.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidural analgesia versus intravenous analgesia after minimally invasive repair of pectus excavatum in pediatric patients: a systematic review and meta-analysis
- Introduction to systematic review and meta-analysis
- Effect of Preoperative Infiltration on Postoperative Analgesic Requirements in Total Abdominal Hysterectomy Patients
- The Efficacy of Preemptive Analgesia With Pregabalin in Septoplasty
- Erector spinae plane block for spinal surgery: a systematic review and meta-analysis