J Pathol Transl Med.
2022 Mar;56(2):103-108. 10.4132/jptm.2021.10.29.
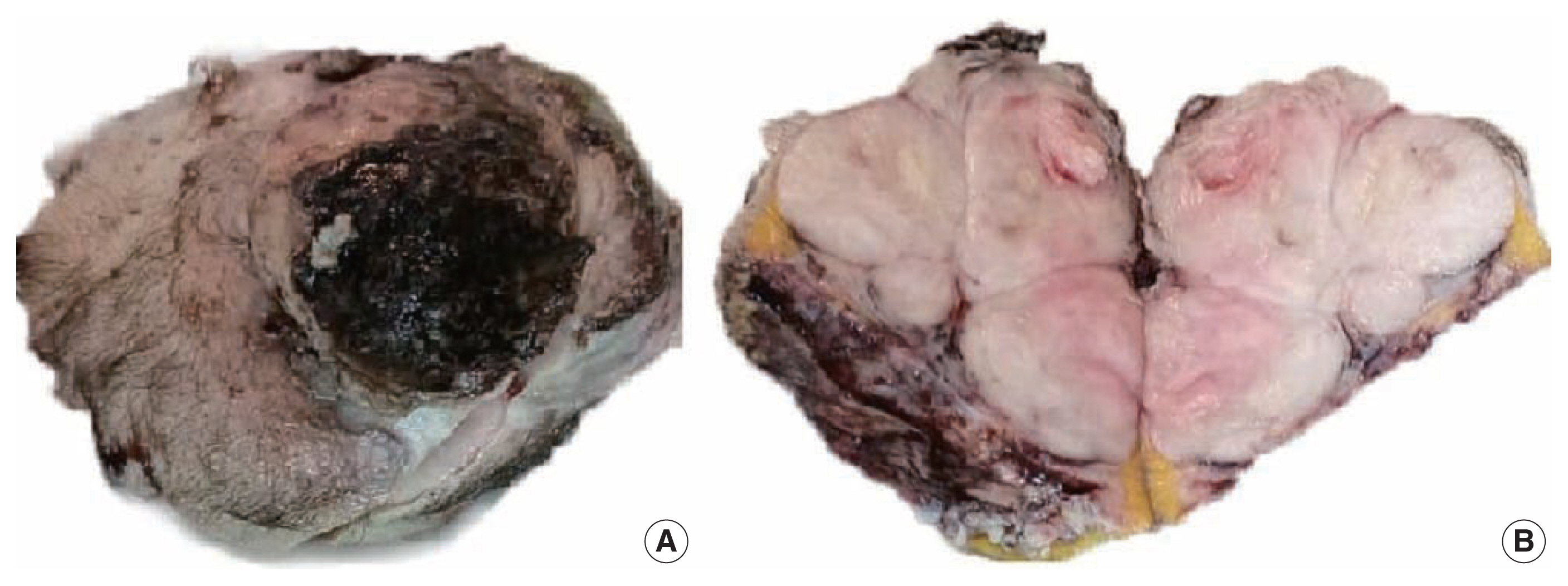
Recurrent malignant solitary fibrous tumor of the scalp: a case report and literature review
- Affiliations
-
- 1Department of Pathology, Faculty of Medicine, Al-Azhar University, Damietta Branch, Damietta, Egypt
- 2Department of Pathology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
- 3Mansoura Dermatology, Venereology and Leprosy Hospital, Mansoura, Egypt
- 4Molecular Diagnostic Laboratory, Johns Hopkins Aramco Healthcare Dhahran, Dhahran, Saudi Arabia
- KMID: 2527195
- DOI: http://doi.org/10.4132/jptm.2021.10.29
Abstract
- Solitary fibrous tumor (SFT) is a rare type of mesenchymal neoplasm that first was discovered in the pleura but can also affect the peritoneum, lungs, mediastinum, and skin. Cutaneous malignant SFT is an extremely rare tumor that resembles dermatofibrosacoma protuberance (DFSP) histologically and immunohistochemically. Herein, we describe a case of malignant SFT that presented as a recurrent mass on the scalp. The first lesion was totally excised one year before recurrence and was diagnosed as a DFSP based on the histopathology and cluster of differentiation 34 immunostaining positivity. Re-examination of the previously examined specimen was considered. Activator of transcription 6 positivity was also detected in the tissue, confirming the diagnosis of a recurrent malignant SFT rather than DFSP. There was no evidence of recurrence, locoregional, or distant metastases at six months after lesion removal with a safety margin.
Figure
Reference
-
References
1. Hasegawa T, Matsuno Y, Shimoda T, Hasegawa F, Sano T, Hirohashi S. Extrathoracic solitary fibrous tumors: their histological variability and potentially aggressive behavior. Hum Pathol. 1999; 30:1464–73.
Article2. Zhou Y, Chu X, Yi Y, Tong L, Dai Y. Malignant solitary fibrous tumor in retroperitoneum: a case report and literature review. Medicine (Baltimore). 2017; 96:e6373.3. Shin K, Kim TW, Lee HJ, et al. A case of malignant solitary fibrous tumor of the skin. Ann Dermatol. 2019; 31:226–8.
Article4. Fletcher CD, Bridge JA, Lee JC. Extrapleural solitary fibrous tumour. Fletcher CD, Bridge JA, Hogendoorn PC, Meertens F, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press;2013. p. 80–2.5. Lococo F, Cesario A, Cardillo G, et al. Malignant solitary fibrous tumors of the pleura: retrospective review of a multicenter series. J Thorac Oncol. 2012; 7:1698–706.
Article6. Creytens D, Ferdinande L, Van Dorpe J. Histopathologically malignant solitary fibrous tumor of the skin: a report of an unusual case. J Cutan Pathol. 2016; 43:629–31.
Article7. Ronchi A, La Mantia E, Gigantino V, et al. A rare case of malignant solitary fibrous tumor in prostate with review of the literature. Diagn Pathol. 2017; 12:50.
Article8. Geramizadeh B, Marzban M, Churg A. Role of immunohistochemistry in the diagnosis of solitary fibrous tumor, a review. Iran J Pathol. 2016; 11:195–203.9. Kwon JH, Song JS, Jung HW, Lee JS, Cho KJ. Malignant solitary fibrous tumor with heterologous rhabdomyosarcomatous differentiation: a case report. J Pathol Transl Med. 2017; 51:171–5.
Article10. Klemperer P, Coleman BR. Primary neoplasms of the pleura: a report of five cases. Am J Ind Med. 1992; 22:1–31.
Article11. Guo W, Xiao HL, Jiang YG, et al. Retrospective analysis for thirty-nine patients with solitary fibrous tumor of pleura and review of the literature. World J Surg Oncol. 2011; 9:134.
Article12. Geramizadeh B, Banani A, Moradi A, Hosseini SM, Foroutan H. Intrapulmonary solitary fibrous tumor with bronchial involvement: a rare case report in a child. J Pediatr Surg. 2010; 45:249–51.
Article13. Vasile G, Mancuso C, White R, et al. Rare meningeal-derived malignant hemangiopericytoma/solitary fibrous tumor grade II–III presenting as a subcutaneous mass on the scalp. JAAD Case Rep. 2020; 6:861–3.
Article14. Mori S, Lezcano C, Miraflor AP, Busam KJ, Lee EH. Solitary fibrous tumor presenting on the scalp: a potential diagnostic pitfall. J Cutan Pathol. 2018; 45:557–60.
Article15. Feasel P, Al-Ibraheemi A, Fritchie K, et al. Superficial solitary fibrous tumor: a series of 26 cases. Am J Surg Pathol. 2018; 42:778–85.16. Kim JH, Kim DC, Lee R, et al. Myxoid solitary fibrous tumor on the scalp. Arch Craniofac Surg. 2017; 18:269–72.
Article17. Shirley BM, Kang DR, Sakamoto AH. Malignant solitary fibrous tumor of the scalp. J Maxillofac Oral Surg. 2016; 15:245–8.
Article18. Omori Y, Saeki H, Ito K, et al. Solitary fibrous tumour of the scalp. Clin Exp Dermatol. 2014; 39:539–41.
Article19. Rizk T, Awada A, Sebaaly A, Hourani R. Solitary fibrous tumor of the scalp in a child. J Neurosurg Pediatr. 2013; 11:79–81.
Article20. Tourabi K, Moussaoui A, Khaless A, et al. Solitary fibrous tumor of the scalp: a case report. Ann Chir Plast Esthet. 2008; 53:526–30.21. Erdag G, Qureshi HS, Patterson JW, Wick MR. Solitary fibrous tumors of the skin: a clinicopathologic study of 10 cases and review of the literature. J Cutan Pathol. 2007; 34:844–50.
Article22. Ramdial PK, Madaree A. Aggressive CD34-positive fibrous scalp lesion of childhood: extrapulmonary solitary fibrous tumor. Pediatr Dev Pathol. 2001; 4:267–75.
Article23. Cowper SE, Kilpatrick T, Proper S, Morgan MB. Solitary fibrous tumor of the skin. Am J Dermatopathol. 1999; 21:213–9.
Article24. Okamura JM, Barr RJ, Battifora H. Solitary fibrous tumor of the skin. Am J Dermatopathol. 1997; 19:515–8.
Article25. Hasan A, Nafie K, Monazea K, Othman A, Salem A, Ismail A. A rare case of recurrent eccrine poroma underlying gluteal abscess. Int J Surg Case Rep. 2020; 75:29–31.
Article26. Wallace SJ, Teixeira R, Miller NF, Raj M, Sheikh H, Sharma R. Extrapleural superficial solitary fibrous tumor on the posterior shoulder: a case report and review of the literature. Eplasty. 2018; 18:e31.27. Hasan A, Deyab A, Monazea K, et al. Clinico-pathological assessment of surgically removed abdominal wall endometriomas following cesarean section. Ann Med Surg (Lond). 2021; 62:219–24.
Article28. Gupta N, Barwad A, Katamuthu K, et al. Solitary fibrous tumour: a diagnostic challenge for the cytopathologist. Cytopathology. 2012; 23:250–5.
Article29. Galed-Placed I, Lopez-Solache L, Reguera-Arias A. Solitary fibrous tumor of the tongue: cytopathologic fine needle aspiration findings. J Cytol. 2019; 36:186–7.
Article30. Demicco EG, Wagner MJ, Maki RG, et al. Risk assessment in solitary fibrous tumors: validation and refinement of a risk stratification model. Mod Pathol. 2017; 30:1433–42.
Article31. Bishop JA, Rekhtman N, Chun J, Wakely PE Jr, Ali SZ. Malignant solitary fibrous tumor: cytopathologic findings and differential diagnosis. Cancer Cytopathol. 2010; 118:83–9.32. Paner GP, Aron M, Hansel DE, Amin MB. Non-epithelial neoplasms of the prostate. Histopathology. 2012; 60:166–86.
Article33. Masuda Y, Kurisaki-Arakawa A, Hara K, et al. A case of dedifferentiated solitary fibrous tumor of the thoracic cavity. Int J Clin Exp Pathol. 2014; 7:386–93.34. Robinson DR, Wu YM, Kalyana-Sundaram S, et al. Identification of recurrent NAB2-STAT6 gene fusions in solitary fibrous tumor by integrative sequencing. Nat Genet. 2013; 45:180–5.
Article35. Doyle LA, Vivero M, Fletcher CD, Mertens F, Hornick JL. Nuclear expression of STAT6 distinguishes solitary fibrous tumor from histologic mimics. Mod Pathol. 2014; 27:390–5.
Article36. Cardillo G, Lococo F, Carleo F, Martelli M. Solitary fibrous tumors of the pleura. Curr Opin Pulm Med. 2012; 18:339–46.
Article37. Martin-Broto J, Stacchiotti S, Lopez-Pousa A, et al. Pazopanib for treatment of advanced malignant and dedifferentiated solitary fibrous tumour: a multicentre, single-arm, phase 2 trial. Lancet Oncol. 2019; 20:134–44.
Article