Clin Exp Otorhinolaryngol.
2022 Feb;15(1):24-48. 10.21053/ceo.2021.00633.
Care and Management of Voice Change in Thyroid Surgery: Korean Society of Laryngology, Phoniatrics and Logopedics Clinical Practice Guideline
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, National Cancer Center, Goyang, Korea
- 2Division of Speech Pathology and Audiology, Research Institute of Audiology and Speech Pathology, College of Natural Sciences, Hallym University, Chuncheon, Korea
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Korea University College of Medicine, Seoul, Korea
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Korea Cancer Center Hospital, Korea Institute of Radiological and Medical Sciences, Seoul, Korea
- 5Department of Otorhinolaryngology-Head and Neck Surgery, Yeungnam University College of Medicine, Daegu, Korea
- 6Department of Otorhinolaryngology-Head and Neck Surgery, Jeonbuk National University Hospital, Jeonbuk National University Medical School, Jeonju, Korea
- 7Department of Otorhinolaryngology-Head and Neck Surgery, Ewha Womans University College of Medicine, Seoul, Korea
- 8Department of Otorhinolaryngology-Head and Neck Surgery, Inha University College of Medicine, Incheon, Korea
- 9Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea
- 10Department of Otorhinolaryngology-Head and Neck Surgery, Dong-A University College of Medicine, Busan, Korea
- 11Department of Otorhinolaryngology-Head and Neck Surgery, Kyungpook National University, School of Medicine, Daegu, Korea
- 12Department of Otorhinolaryngology-Head and Neck Surgery, Dankook University College of Medicine, Cheonan, Korea
- 13Department of Otorhinolaryngology-Head and Neck Surgery, Kyung Hee University School of Medicine, Seoul, Korea
- 14Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- 15Department of Otorhinolaryngology-Head and Neck Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 16Department of Otorhinolaryngology-Head and Neck Surgery, Soonchunhyang University College of Medicine, Bucheon, Korea
- 17Department of Otorhinolaryngology-Head and Neck Surgery, Yonsei University College of Medicine, Seoul, Korea
- 18Department of Otorhinolaryngology-Head and Neck Surgery, Pusan National University School of Medicine, Busan, Korea
- 19Department of Otorhinolaryngology-Head and Neck Surgery, Dongnam Institute Of Radiological and Medical Sciences, Busan, Korea
- 20Voice and Speech Clinic, Department of Otorhinolaryngology-Head and Neck Surgery, Dankook University College of Medicine, Cheonan, Korea
- 21Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- KMID: 2527111
- DOI: http://doi.org/10.21053/ceo.2021.00633
Abstract
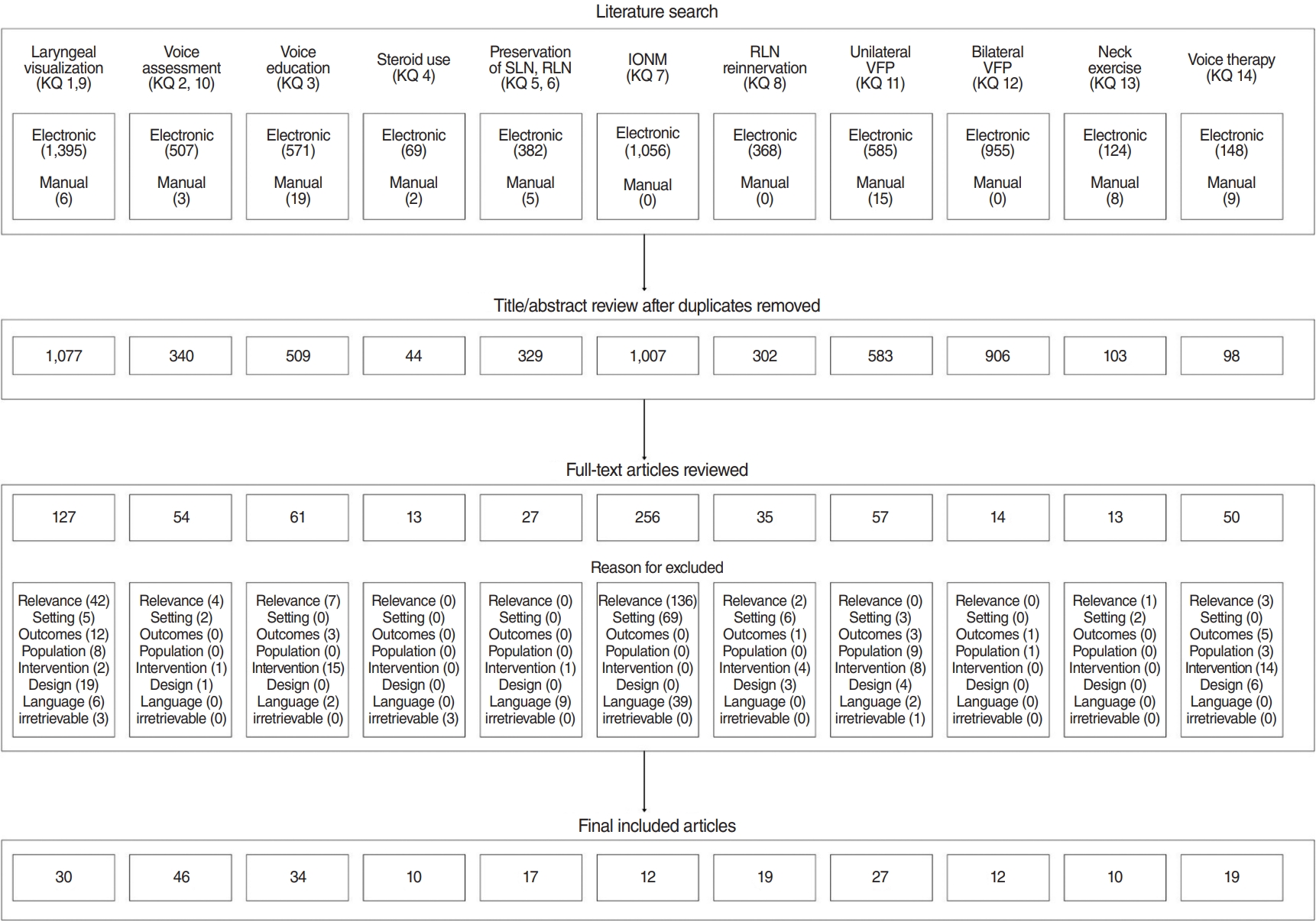
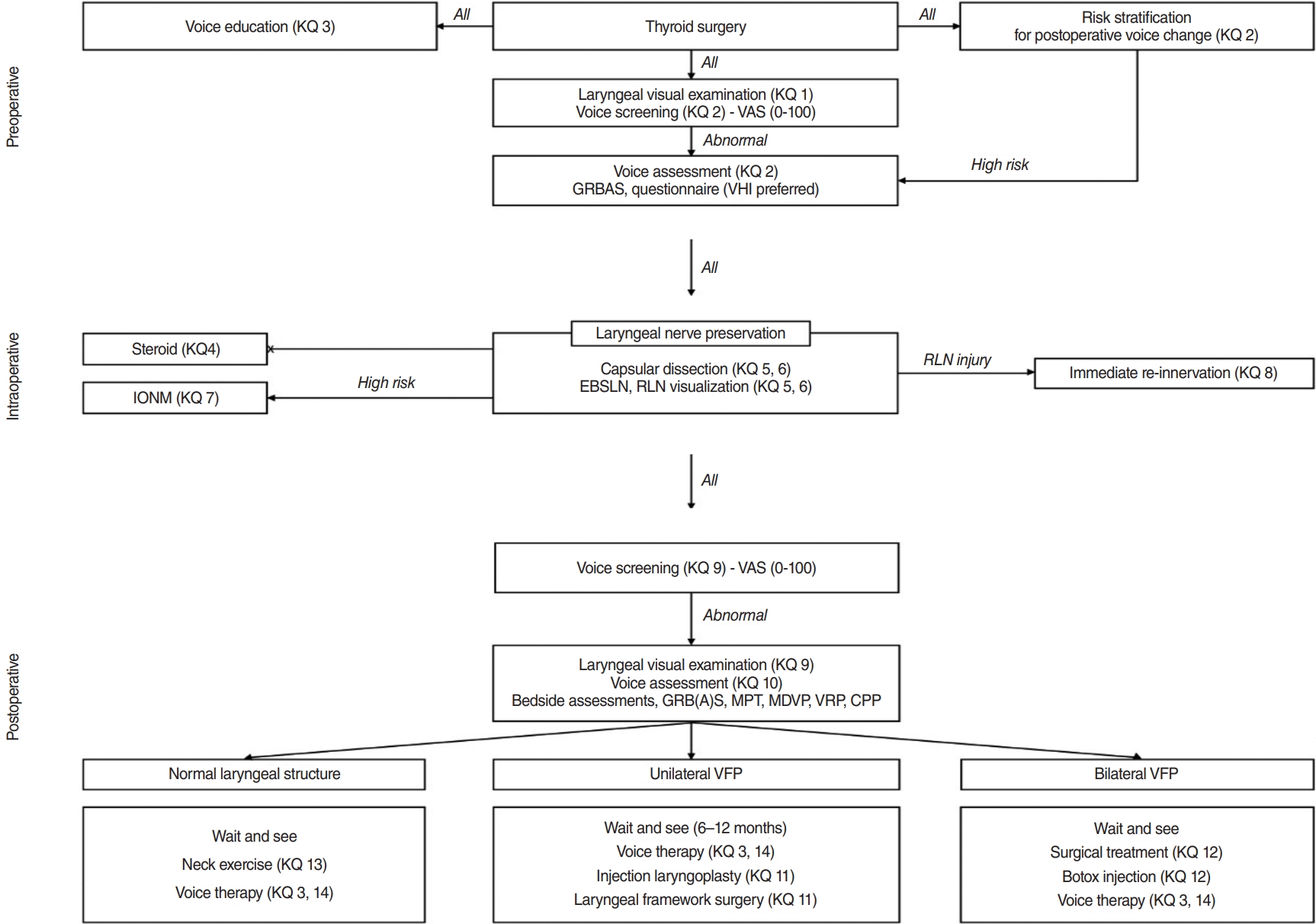
- Voice change is a common complaint after thyroid surgery and has a significant impact on quality of life. The Korean Society of Laryngology, Phoniatrics and Logopedics assembled a task force to establish guideline recommendations on education, care, and management related to thyroid surgery. The guideline recommendations encompass preoperative voice education, management of anticipated voice change during surgery, and comprehensive voice care after thyroid surgery, and include in-depth information and up-to-date knowledge based on validated literature. The committee constructed 14 key questions (KQs) in three categories—preoperative (KQ 1–2), intraoperative (KQ 3–8), and postoperative (KQ 9–14) management—and developed 18 evidence-based recommendations. The Delphi survey reached an agreement on each recommendation. A detailed evidence profile is presented for each recommendation. The level of evidence for each recommendation was classified as high-quality, moderate-quality, or low-quality. The strength of each recommendation was designated as strong or weak considering the level of evidence supporting the recommendation. The guidelines are primarily targeted toward physicians who treat thyroid surgery patients and speech-language pathologists participating in patient care. These guidelines will also help primary care physicians, nurses, healthcare policymakers, and patients improve their understanding of voice changes and voice care after thyroid surgery.
Keyword
Figure
Cited by 2 articles
-
Management of Bilateral Vocal Fold Paralysis, Injury of External Branch of Superior Laryngeal Nerve after Thyroid Surgery
Seo Jun Kang, Ji Won Kim
Int J Thyroidol. 2023;16(2):152-156. doi: 10.11106/ijt.2023.16.2.152.Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part I. Initial Management of Differentiated Thyroid Cancers - Chapter 3. Perioperative Assessment of Surgical Complications 2024
Chang Hwan Ryu, Ho-Cheol Kang, Bon Seok Koo, Sun Wook Kim, Dong Gyu Na, Young Joo Park, Jun-Ook Park, Young Shin Song, Seung Hoon Woo, Ho-Ryun Won, Sihoon Lee, Eun Kyung Lee, Dong-Jun Lim, Yun Kyung Jeon, Yun Jae Chung, Jae-Yol Lim, A Ram Hong
Int J Thyroidol. 2024;17(1):53-60. doi: 10.11106/ijt.2024.17.1.53.
Reference
-
1. Jung KW, Won YJ, Kong HJ, Lee ES. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2016. Cancer Res Treat. 2019; Apr. 51(2):417–30.
Article2. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016; Jan. 26(1):1–133.
Article3. Yi KH, Lee EK, Kang HC, Koh Y, Kim SW, Kim IJ, et al. 2016 Revised Korean Thyroid Association management guidelines for patients with thyroid nodules and thyroid cancer. Int J Thyroidol. 2016; Nov. 9(2):59–126.
Article4. Ryu CH, Park B, Ryu J, Ryu YM, Jo SA, Lee YJ, et al. Development and evaluation of a Korean version of a thyroid-specific quality-of-life questionnaire scale in thyroid cancer patients. Cancer Res Treat. 2018; Apr. 50(2):405–15.
Article5. Ryu CH, Ryu J, Ryu YM, Lee YJ, Lee EK, Kim SK, et al. Administration of radioactive iodine therapy within 1 year after total thyroidectomy does not affect vocal function. J Nucl Med. 2015; Oct. 56(10):1480–6.
Article6. Chandrasekhar SS, Randolph GW, Seidman MD, Rosenfeld RM, Angelos P, Barkmeier-Kraemer J, et al. Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg. 2013; Jun. 148(6 Suppl):S1–37.7. de Pedro Netto I, Fae A, Vartanian JG, Barros AP, Correia LM, Toledo RN, et al. Voice and vocal self-assessment after thyroidectomy. Head Neck. 2006; Dec. 28(12):1106–14.
Article8. Delgado-Vargas B, Lloris Romero-Salazar A, Cobeta I. Vocal changes following thyroid surgery: prospective study of objective and subjective parameters. J Voice. 2019; Jan. 33(1):27–32.
Article9. Akyildiz S, Ogut F, Akyildiz M, Engin EZ. A multivariate analysis of objective voice changes after thyroidectomy without laryngeal nerve injury. Arch Otolaryngol Head Neck Surg. 2008; Jun. 134(6):596–602.
Article10. Chun BJ, Bae JS, Chae BJ, Hwang YS, Shim MR, Sun DI. Early postoperative vocal function evaluation after thyroidectomy using thyroidectomy related voice questionnaire. World J Surg. 2012; Oct. 36(10):2503–8.
Article11. Dixon H, Amin N, Lindisfarne E, Gibbins N, Harries M. Pre- and post-operative assessment of voice in thyroidectomy patients: an audit cycle. Clin Otolaryngol. 2012; Jul. 37(S1):34–5.12. Park JO, Bae JS, Chae BJ, Kim CS, Nam IC, Chun BJ, et al. How can we screen voice problems effectively in patients undergoing thyroid surgery. Thyroid. 2013; Nov. 23(11):1437–44.
Article13. Jeannon JP, Orabi AA, Bruch GA, Abdalsalam HA, Simo R. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract. 2009; Apr. 63(4):624–9.
Article14. Kierner AC, Aigner M, Burian M. The external branch of the superior laryngeal nerve: its topographical anatomy as related to surgery of the neck. Arch Otolaryngol Head Neck Surg. 1998; Mar. 124(3):301–3.
Article15. Orestes MI, Chhetri DK. Superior laryngeal nerve injury: effects, clinical findings, prognosis, and management options. Curr Opin Otolaryngol Head Neck Surg. 2014; Dec. 22(6):439–43.16. Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007; Feb. 7:10.
Article17. Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013; Apr. 66(4):408–14.
Article18. Farrag TY, Samlan RA, Lin FR, Tufano RP. The utility of evaluating true vocal fold motion before thyroid surgery. Laryngoscope. 2006; Feb. 116(2):235–8.
Article19. Randolph GW, Kamani D. The importance of preoperative laryngoscopy in patients undergoing thyroidectomy: voice, vocal cord function, and the preoperative detection of invasive thyroid malignancy. Surgery. 2006; Mar. 139(3):357–62.
Article20. Nam IC, Bae JS, Shim MR, Hwang YS, Kim MS, Sun DI. The importance of preoperative laryngeal examination before thyroidectomy and the usefulness of a voice questionnaire in screening. World J Surg. 2012; Feb. 36(2):303–9.
Article21. Bilimoria KY, Bentrem DJ, Ko CY, Stewart AK, Winchester DP, Talamonti MS, et al. Extent of surgery affects survival for papillary thyroid cancer. Ann Surg. 2007; Sep. 246(3):375–81.
Article22. Hiramatsu H, Tokashiki R, Nakamura M, Motohashi R, Yoshida T, Suzuki M. Characterization of arytenoid vertical displacement in unilateral vocal fold paralysis by three-dimensional computed tomography. Eur Arch Otorhinolaryngol. 2009; Jan. 266(1):97–104.
Article23. Laeeq K, Pandian V, Skinner M, Masood H, Stewart CM, Weatherly R, et al. Learning curve for competency in flexible laryngoscopy. Laryngoscope. 2010; Oct. 120(10):1950–3.
Article24. Paul BC, Rafii B, Achlatis S, Amin MR, Branski RC. Morbidity and patient perception of flexible laryngoscopy. Ann Otol Rhinol Laryngol. 2012; Nov. 121(11):708–13.
Article25. Woodson GE. Configuration of the glottis in laryngeal paralysis. I: clinical study. Laryngoscope. 1993; Nov. 103(11 Pt 1):1227–34.26. Simpson CB, Cheung EJ, Jackson CJ. Vocal fold paresis: clinical and electrophysiologic features in a tertiary laryngology practice. J Voice. 2009; May. 23(3):396–8.
Article27. Sinclair CF, Bumpous JM, Haugen BR, Chala A, Meltzer D, Miller BS, et al. Laryngeal examination in thyroid and parathyroid surgery: an American Head and Neck Society consensus statement: AHNS Consensus Statement. Head Neck. 2016; Jun. 38(6):811–9.
Article28. Perros P, Boelaert K, Colley S, Evans C, Evans RM, Gerrard Ba G, et al. Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf). 2014; Jul. 81 Suppl 1:1–122.
Article29. Dralle H, Musholt TJ, Schabram J, Steinmuller T, Frilling A, Simon D, et al. German Association of Endocrine Surgeons practice guideline for the surgical management of malignant thyroid tumors. Langenbecks Arch Surg. 2013; Mar. 398(3):347–75.
Article30. Randolph GW, Dralle H; International Intraoperative Monitoring Study Group, Abdullah H, Barczynski M, Bellantone R, et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. 2011; Jan. 121 Suppl 1:S1–16.
Article31. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines® ): thyroid carcinoma. version 2.2020. Plymouth Meeting (PA): National Comprehensive Cancer Network;2020.32. Maher DI, Goare S, Forrest E, Grodski S, Serpell JW, Lee JC. Routine preoperative laryngoscopy for thyroid surgery is not necessary without risk factors. Thyroid. 2019; Nov. 29(11):1646–52.
Article33. Zanocco K, Kaltman DJ, Wu JX, Fingeret A, Heller KS, Lee JA, et al. Cost effectiveness of routine laryngoscopy in the surgical treatment of differentiated thyroid cancer. Ann Surg Oncol. 2018; Apr. 25(4):949–56.
Article34. McIvor NP, Flint DJ, Gillibrand J, Morton RP. Thyroid surgery and voice-related outcomes. Aust N Z J Surg. 2000; Mar. 70(3):179–83.
Article35. Meek P, Carding PN, Howard DH, Lennard TW. Voice change following thyroid and parathyroid surgery. J Voice. 2008; Nov. 22(6):765–72.
Article36. Ryu CH, Han S, Lee MS, Kim SY, Nam SY, Roh JL, et al. Voice changes in elderly adults: prevalence and the effect of social, behavioral, and health status on voice quality. J Am Geriatr Soc. 2015; Aug. 63(8):1608–14.
Article37. Stojadinovic A, Henry LR, Howard RS, Gurevich-Uvena J, Makashay MJ, Coppit GL, et al. Prospective trial of voice outcomes after thyroidectomy: evaluation of patient-reported and clinician-determined voice assessments in identifying postthyroidectomy dysphonia. Surgery. 2008; Jun. 143(6):732–42.
Article38. Dejonckere PH, Bradley P, Clemente P, Cornut G, Crevier-Buchman L, Friedrich G, et al. A basic protocol for functional assessment of voice pathology, especially for investigating the efficacy of (phonosurgical) treatments and evaluating new assessment techniques. Guideline elaborated by the Committee on Phoniatrics of the European Laryngological Society (ELS). Eur Arch Otorhinolaryngol. 2001; Feb. 258(2):77–82.
Article39. Biddle AK, Watson LR, Hooper CR, Lohr KN, Sutton SF. Criteria for determining disability in speech-language disorders. Evid Rep Technol Assess (Summ). 2002; Jan. (52):1–4.40. Rosen CA, Lee AS, Osborne J, Zullo T, Murry T. Development and validation of the voice handicap index-10. Laryngoscope. 2004; Sep. 114(9):1549–56.
Article41. Morzaria S, Damrose EJ. A comparison of the VHI, VHI-10, and VRQOL for measuring the effect of botox therapy in adductor spasmodic dysphonia. J Voice. 2012; May. 26(3):378–80.
Article42. Ma EP, Yiu EM. Voice activity and participation profile: assessing the impact of voice disorders on daily activities. J Speech Lang Hear Res. 2001; Jun. 44(3):511–24.43. Nanjundeswaran C, Jacobson BH, Gartner-Schmidt J, Verdolini Abbott K. Vocal Fatigue Index (VFI): development and validation. J Voice. 2015; Jul. 29(4):433–40.
Article44. Ko DH. Experimental phonetics for speech-language pathologists. Seoul: Hakjisa Publisher;2015.45. Korean Society of Laryngology, Phoniatrics and Logopedics. Understanding of laryngology: voice, speech and swallowing. Seoul: Panmun Education;2016.46. Kempster GB, Gerratt BR, Verdolini Abbott K, Barkmeier-Kraemer J, Hillman RE. Consensus auditory-perceptual evaluation of voice: development of a standardized clinical protocol. Am J Speech Lang Pathol. 2009; May. 18(2):124–32.
Article47. Kark AE, Kissin MW, Auerbach R, Meikle M. Voice changes after thyroidectomy: role of the external laryngeal nerve. Br Med J (Clin Res Ed). 1984; Nov. 289(6456):1412–5.
Article48. Hong KH, Kim YK. Phonatory characteristics of patients undergoing thyroidectomy without laryngeal nerve injury. Otolaryngol Head Neck Surg. 1997; Oct. 117(4):399–404.
Article49. Choi SH. Development of Korean standardized sentences on voice quality evaluation for dysphonia. Audiol Speech Res. 2018; Apr. 14(2):128–42.
Article50. Aluffi P, Policarpo M, Cherovac C, Olina M, Dosdegani R, Pia F. Post-thyroidectomy superior laryngeal nerve injury. Eur Arch Otorhinolaryngol. 2001; Nov. 258(9):451–4.
Article51. Song CM, Kim H, Kwon TK, Sung MW, Kim KH, Hah JH. Investigation on patients’ understanding and concern about the disease and recovery rate in thyroidectomy patients to enhance satisfaction of hospitalization. Korean J Otorhinolaryngol-Head Neck Surg. 2010; Sep. 53(9):557–63.
Article52. Chung EJ. Voice care for the post-thyroidectomy dysphonia. J Korean Soc Laryngol Phoniatr Logoped. 2016; Jun. 27(1):14–7.
Article53. Feldman-Stewart D, Capirci C, Brennenstuhl S, Tong C, Abacioglu U, Gawkowska-Suwinska M, et al. Information for decision making by patients with early-stage prostate cancer: a comparison across 9 countries. Med Decis Making. 2011; Sep-Oct. 31(5):754–66.
Article54. Street RL Jr, Voigt B. Patient participation in deciding breast cancer treatment and subsequent quality of life. Med Decis Making. 1997; Jul-Sep. 17(3):298–306.
Article55. El-Banna M, Youssef G. Early voice therapy in patients with unilateral vocal fold paralysis. Folia Phoniatr Logop. 2014; 66(6):237–43.
Article56. Abdul-Sater L, Henry M, Majdan A, Mijovic T, Franklin JH, Brandt MG, et al. What are thyroidectomy patients really concerned about. Otolaryngol Head Neck Surg. 2011; May. 144(5):685–90.
Article57. SFORL Work Group, Santini J, Alfonsi JP, Bonichon F, Bozec A, Giovanni A, et al. Patient information ahead of thyroid surgery: Guidelines of the French Society of Oto-Rhino-Laryngology and Head and Neck Surgery (SFORL). Eur Ann Otorhinolaryngol Head Neck Dis. 2013; Dec. 130(6):363–8.
Article58. Chen X, Wan P, Yu Y, Li M, Xu Y, Huang P, et al. Types and timing of therapy for vocal fold paresis/paralysis after thyroidectomy: a systematic review and meta-analysis. J Voice. 2014; Nov. 28(6):799–808.
Article59. Chan Y, Irish JC, Wood SJ, Rotstein LE, Brown DH, Gullane PJ, et al. Patient education and informed consent in head and neck surgery. Arch Otolaryngol Head Neck Surg. 2002; Nov. 128(11):1269–74.
Article60. Awan SN, Helou LB, Stojadinovic A, Solomon NP. Tracking voice change after thyroidectomy: application of spectral/cepstral analyses. Clin Linguist Phon. 2011; Apr. 25(4):302–20.
Article61. Alsaffar H, Wilson L, Kamdar DP, Sultanov F, Enepekides D, Higgins KM. Informed consent: do information pamphlets improve post-operative risk-recall in patients undergoing total thyroidectomy. Prospective randomized control study. J Otolaryngol Head Neck Surg. 2016; Feb. 45:14.
Article62. Patel CR, Cherla DV, Sanghvi S, Baredes S, Eloy JA. Readability assessment of online thyroid surgery patient education materials. Head Neck. 2013; Oct. 35(10):1421–5.
Article63. Yeo H, Roman S, Air M, Maser C, Trapasso T, Kinder B, et al. Filling a void: thyroid cancer surgery information on the internet. World J Surg. 2007; Jun. 31(6):1185–91.
Article64. Temiz Z, Ozturk D, Ugras GA, Oztekin SD, Sengul E. Determination of patient learning needs after thyroidectomy. Asian Pac J Cancer Prev. 2016; 17(3):1479–83.
Article65. Hosoya M, Kobayashi R, Ishii T, Senarita M, Kuroda H, Misawa H, et al. Vocal hygiene education program reduces surgical interventions for benign vocal fold lesions: a randomized controlled trial. Laryngoscope. 2018; Nov. 128(11):2593–9.
Article66. Belafsky PC, Postma GN, Reulbach TR, Holland BW, Koufman JA. Muscle tension dysphonia as a sign of underlying glottal insufficiency. Otolaryngol Head Neck Surg. 2002; Nov. 127(5):448–51.
Article67. Krouse HJ, Reavis CC, Stachler RJ, Francis DO, O’Connor S. Plain language summary: hoarseness (dysphonia). Otolaryngol Head Neck Surg. 2018; Mar. 158(3):427–31.
Article68. Rubin AD, Sataloff RT. Vocal fold paresis and paralysis: what the thyroid surgeon should know. Surg Oncol Clin N Am. 2008; Jan. 17(1):175–96.
Article69. D’Alatri L, Galla S, Rigante M, Antonelli O, Buldrini S, Marchese MR. Role of early voice therapy in patients affected by unilateral vocal fold paralysis. J Laryngol Otol. 2008; Sep. 122(9):936–41.
Article70. Mattioli F, Bergamini G, Alicandri-Ciufelli M, Molteni G, Luppi MP, Nizzoli F, et al. The role of early voice therapy in the incidence of motility recovery in unilateral vocal fold paralysis. Logoped Phoniatr Vocol. 2011; Apr. 36(1):40–7.
Article71. Tang SS, Thibeault SL. Timing of voice therapy: a primary investigation of voice outcomes for surgical benign vocal fold lesion patients. J Voice. 2017; Jan. 31(1):129.e1–129.e7.
Article72. Al-Yahya SN, Muhammad R, Suhaimi S, Azman M, Mohamed AS, Baki MM. Selective laryngeal examination: sensitivity of endocrine surgeons in screening voice abnormality. J Voice. 2020; Sep. 34(5):811.e13–811.e20.
Article73. Park JO, Bae JS, Lee SH, Shim MR, Hwang YS, Joo YH, et al. Multivariate analysis of risk factors in the development of a lower-pitched voice after thyroidectomy. Ann Otol Rhinol Laryngol. 2017; Feb. 126(2):117–23.
Article74. Vetshev PS, Yankin PL, Zhivotov VA, Poddubniy EI, Drozhzhin AY, Prokhorov VD. Risk factors and prognosis of voice disorders after surgical treatment of thyroid and parathyroid diseases. Khirurgiia (Mosk). 2019; (4):5–14.
Article75. Park JO, Bae JS, Lee SH, Shim MR, Hwang YS, Joo YH, et al. The long-term prognosis of voice pitch change in female patients after thyroid surgery. World J Surg. 2016; Oct. 40(10):2382–90.
Article76. Papadakis CE, Asimakopoulou P, Proimos E, Perogamvrakis G, Papoutsaki E, Chimona T. Subjective and objective voice assessments after recurrent laryngeal nerve-preserved total thyroidectomy. J Voice. 2017; Jul. 31(4):515.e15–515.e21.
Article77. Sahli Z, Canner JK, Najjar O, Schneider EB, Prescott JD, Russell JO, et al. Association between age and patient-reported changes in voice and swallowing after thyroidectomy. Laryngoscope. 2019; Feb. 129(2):519–24.
Article78. Dhillon VK, Rettig E, Noureldine SI, Genther DJ, Hassoon A, Al Khadem MG, et al. The incidence of vocal fold motion impairment after primary thyroid and parathyroid surgery for a single high-volume academic surgeon determined by pre- and immediate postoperative fiberoptic laryngoscopy. Int J Surg. 2018; Aug. 56:73–8.
Article79. Ryu J, Ryu YM, Jung Y, Kim S, Lee YJ, Lee E, et al. Extent of thyroidectomy affects vocal and throat functions: a prospective observational study of lobectomy versus total thyroidectomy. 2013; Sep. 154(3):611–20.
Article80. Park YM, Oh KH, Cho JG, Baek SK, Kwon SY, Jung KY, et al. Changes in voice- and swallowing-related symptoms after thyroidectomy: one-year follow-up study. Ann Otol Rhinol Laryngol. 2018; Mar. 127(3):171–7.
Article81. Scerrino G, Inviati A, Di Giovanni S, Paladino NC, Di Paola V, Lo Re G, et al. Esophageal motility changes after thyroidectomy: possible associations with postoperative voice and swallowing disorders: preliminary results. Otolaryngol Head Neck Surg. 2013; Jun. 148(6):926–32.
Article82. Cohen SM, Lee HJ, Roy N, Misono S. Pharmacologic management of voice disorders by general medicine providers and otolaryngologists. Laryngoscope. 2018; Mar. 128(3):682–9.
Article83. Holland NJ, Weiner GM. Recent developments in Bell’s palsy. BMJ. 2004; Sep. 329(7465):553–7.
Article84. Stachler RJ, Chandrasekhar SS, Archer SM, Rosenfeld RM, Schwartz SR, Barrs DM, et al. Clinical practice guideline: sudden hearing loss. Otolaryngol Head Neck Surg. 2012; Mar. 146(3 Suppl):S1–35.
Article85. Wang LF, Lee KW, Kuo WR, Wu CW, Lu SP, Chiang FY. The efficacy of intraoperative corticosteroids in recurrent laryngeal nerve palsy after thyroid surgery. World J Surg. 2006; Mar. 30(3):299–303.
Article86. Worni M, Schudel HH, Seifert E, Inglin R, Hagemann M, Vorburger SA, et al. Randomized controlled trial on single dose steroid before thyroidectomy for benign disease to improve postoperative nausea, pain, and vocal function. Ann Surg. 2008; Dec. 248(6):1060–6.
Article87. Feroci F, Rettori M, Borrelli A, Lenzi E, Ottaviano A, Scatizzi M. Dexamethasone prophylaxis before thyroidectomy to reduce postoperative nausea, pain, and vocal dysfunction: a randomized clinical controlled trial. Head Neck. 2011; Jun. 33(6):840–6.
Article88. Nasiri S, Shafag S, Khorgami Z, Sodagari N, Aminian A, Hedayat A. Does corticosteroid have any beneficial effect on voice change after thyroidectomy. Am Surg. 2013; Dec. 79(12):1258–62.
Article89. Cheng SP, Liu TP, Yang PS, Lee KS, Liu CL. Effect of perioperative dexamethasone on subjective voice quality after thyroidectomy: a meta-analysis and systematic review. Langenbecks Arch Surg. 2015; Dec. 400(8):929–36.
Article90. Kim JS, Kwon SH, Lee SE, Lee EJ, Lee MH. Effect of single-dose intravenous dexamethasone on subjective voice quality after thyroidectomy: a meta-analysis. Medicine (Baltimore). 2018; Sep. 97(36):e11832.91. Noel JE, Kligerman MP, Megwalu UC. Intraoperative corticosteroids for voice outcomes among patients undergoing thyroidectomy: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2018; Nov. 159(5):811–6.
Article92. Roy N, Smith ME, Dromey C, Redd J, Neff S, Grennan D. Exploring the phonatory effects of external superior laryngeal nerve paralysis: an in vivo model. Laryngoscope. 2009; Apr. 119(4):816–26.
Article93. Cernea CR, Ferraz AR, Nishio S, Dutra A Jr, Hojaij FC, dos Santos LR. Surgical anatomy of the external branch of the superior laryngeal nerve. Head Neck. 1992; Sep-Oct. 14(5):380–3.
Article94. Bliss RD, Gauger PG, Delbridge LW. Surgeon’s approach to the thyroid gland: surgical anatomy and the importance of technique. World J Surg. 2000; Aug. 24(8):891–7.
Article95. Garas G, Okabayashi K, Ashrafian H, Shetty K, Palazzo F, Tolley N, et al. Which hemostatic device in thyroid surgery? A network meta-analysis of surgical technologies. Thyroid. 2013; Sep. 23(9):1138–50.
Article96. Aytac B, Karamercan A. Recurrent laryngeal nerve injury and preservation in thyroidectomy. Saudi Med J. 2005; Nov. 26(11):1746–9.97. Rathi PK, Shaikh AR, Shaikh GA. Identification of recurrent laryngeal nerve during thyroidectomy decreases the risk of nerve injury. Pak J Med Sci. 2010; 26(1):148–51.98. Steurer M, Passler C, Denk DM, Schneider B, Niederle B, Bigenzahn W. Advantages of recurrent laryngeal nerve identification in thyroidectomy and parathyroidectomy and the importance of preoperative and postoperative laryngoscopic examination in more than 1000 nerves at risk. Laryngoscope. 2002; Jan. 112(1):124–33.
Article99. Sturniolo G, D’Alia C, Tonante A, Gagliano E, Taranto F, Lo Schiavo MG. The recurrent laryngeal nerve related to thyroid surgery. Am J Surg. 1999; Jun. 177(6):485–8.
Article100. Shao T, Qiu W, Yang W. Anatomical variations of the recurrent laryngeal nerve in Chinese patients: a prospective study of 2,404 patients. Sci Rep. 2016; May. 6:25475.
Article101. Delbridge L, Reeve TS, Khadra M, Poole AG. Total thyroidectomy: the technique of capsular dissection. Aust N Z J Surg. 1992; Feb. 62(2):96–9.
Article102. Pelizzo MR, Toniato A, Gemo G. Zuckerkandl’s tuberculum: an arrow pointing to the recurrent laryngeal nerve (constant anatomical landmark). J Am Coll Surg. 1998; Sep. 187(3):333–6.
Article103. Mao XC, Chen C, Wang KJ. Efficacy and safety of LigaSureTM small jaw instrument in thyroidectomy: a 1-year prospective observational study. Eur Arch Otorhinolaryngol. 2018; May. 275(5):1257–63.
Article104. Zhang L, Li N, Yang X, Chen J. A meta-analysis comparing the outcomes of LigaSure Small Jaw versus clamp-and-tie technique or Harmonic Focus Scalpel in thyroidectomy. Medicine (Baltimore). 2017; Mar. 96(11):e6141.
Article105. Bhargav PR, Amar V. Operative technique of endoscopic thyroidectomy: a narration of general principles. Indian J Surg. 2013; Jun. 75(3):216–9.
Article106. Chang E, Kim HY, Koh YW, Chung WY. Overview of robotic thyroidectomy. Gland Surg. 2017; Jun. 6(3):218–28.
Article107. Bai B, Chen W. Protective effects of intraoperative nerve monitoring (IONM) for recurrent laryngeal nerve injury in thyroidectomy: meta-analysis. Sci Rep. 2018; May. 8(1):7761.
Article108. Cirocchi R, Arezzo A, D’Andrea V, Abraha I, Popivanov GI, Avenia N, et al. Intraoperative neuromonitoring versus visual nerve identification for prevention of recurrent laryngeal nerve injury in adults undergoing thyroid surgery. Cochrane Database Syst Rev. 2019; Jan. 1(1):CD012483.
Article109. Higgins TS, Gupta R, Ketcham AS, Sataloff RT, Wadsworth JT, Sinacori JT. Recurrent laryngeal nerve monitoring versus identification alone on post-thyroidectomy true vocal fold palsy: a meta-analysis. Laryngoscope. 2011; May. 121(5):1009–17.
Article110. Lombardi CP, Carnassale G, Damiani G, Acampora A, Raffaelli M, De Crea C, et al. “The final countdown”: is intraoperative, intermittent neuromonitoring really useful in preventing permanent nerve palsy? Evidence from a meta-analysis. Surgery. 2016; Dec. 160(6):1693–706.
Article111. Malik R, Linos D. Intraoperative neuromonitoring in thyroid surgery: a systematic review. World J Surg. 2016; Aug. 40(8):2051–8.
Article112. Rulli F, Ambrogi V, Dionigi G, Amirhassankhani S, Mineo TC, Ottaviani F, et al. Meta-analysis of recurrent laryngeal nerve injury in thyroid surgery with or without intraoperative nerve monitoring. Acta Otorhinolaryngol Ital. 2014; Aug. 34(4):223–9.113. Sanabria A, Ramirez A, Kowalski LP, Silver CE, Shaha AR, Owen RP, et al. Neuromonitoring in thyroidectomy: a meta-analysis of effectiveness from randomized controlled trials. Eur Arch Otorhinolaryngol. 2013; Aug. 270(8):2175–89.
Article114. Sun W, Liu J, Zhang H, Zhang P, Wang Z, Dong W, et al. A metaanalysis of intraoperative neuromonitoring of recurrent laryngeal nerve palsy during thyroid reoperations. Clin Endocrinol (Oxf). 2017; Nov. 87(5):572–80.
Article115. Yang S, Zhou L, Lu Z, Ma B, Ji Q, Wang Y. Systematic review with meta-analysis of intraoperative neuromonitoring during thyroidectomy. Int J Surg. 2017; Mar. 39:104–13.
Article116. Zheng S, Xu Z, Wei Y, Zeng M, He J. Effect of intraoperative neuromonitoring on recurrent laryngeal nerve palsy rates after thyroid surgery: a meta-analysis. J Formos Med Assoc. 2013; Aug. 112(8):463–72.117. Dralle H, Sekulla C, Haerting J, Timmermann W, Neumann HJ, Kruse E, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery. 2004; Dec. 136(6):1310–22.
Article118. Wong KP, Mak KL, Wong CK, Lang BH. Systematic review and meta-analysis on intra-operative neuro-monitoring in high-risk thyroidectomy. Int J Surg. 2017; Feb. 38:21–30.
Article119. Lorenz RR, Esclamado RM, Teker AM, Strome M, Scharpf J, Hicks D, et al. Ansa cervicalis-to-recurrent laryngeal nerve anastomosis for unilateral vocal fold paralysis: experience of a single institution. Ann Otol Rhinol Laryngol. 2008; Jan. 117(1):40–5.
Article120. Miyauchi A, Inoue H, Tomoda C, Fukushima M, Kihara M, Higashiyama T, et al. Improvement in phonation after reconstruction of the recurrent laryngeal nerve in patients with thyroid cancer invading the nerve. Surgery. 2009; Dec. 146(6):1056–62.
Article121. Miyauchi A, Matsusaka K, Kihara M, Matsuzuka F, Hirai K, Yokozawa T, et al. The role of ansa-to-recurrent-laryngeal nerve anastomosis in operations for thyroid cancer. Eur J Surg. 1998; Dec. 164(12):927–33.
Article122. Su WF, Hsu YD, Chen HC, Sheng H. Laryngeal reinnervation by ansa cervicalis nerve implantation for unilateral vocal cord paralysis in humans. J Am Coll Surg. 2007; Jan. 204(1):64–72.
Article123. Zheng H, Li Z, Zhou S, Cuan Y, Wen W. Update: laryngeal reinnervation for unilateral vocal cord paralysis with the ansa cervicalis. Laryngoscope. 1996; Dec. 106(12 Pt 1):1522–7.
Article124. Lee SW, Park KN, Oh SK, Jung CH, Mok JO, Kim CH. Long-term efficacy of primary intraoperative recurrent laryngeal nerve reinnervation in the management of thyroidectomy-related unilateral vocal fold paralysis. Acta Otolaryngol. 2014; Nov. 134(11):1179–84.
Article125. Paniello RC, Edgar JD, Kallogjeri D, Piccirillo JF. Medialization versus reinnervation for unilateral vocal fold paralysis: a multicenter randomized clinical trial. Laryngoscope. 2011; Oct. 121(10):2172–9.
Article126. Iwaki S, Maeda T, Saito M, Otsuki N, Takahashi M, Wakui E, et al. Role of immediate recurrent laryngeal nerve reconstruction in surgery for thyroid cancers with fixed vocal cords. Head Neck. 2017; Mar. 39(3):427–31.
Article127. Lee SW, Park KN. A long-term comparative prospective study between reinnervation and injection laryngoplasty. Laryngoscope. 2018; Aug. 128(8):1893–7.
Article128. Isseroff TF, Pitman MJ. Optimal management of acute recurrent laryngeal nerve injury during thyroidectomy. Curr Otorhinolaryngol Rep. 2013; Sep. 1:163–70.
Article129. Crumley RL. Laryngeal synkinesis revisited. Ann Otol Rhinol Laryngol. 2000; Apr. 109(4):365–71.
Article130. Lee SW. Management of post-throidectomy voice problems: surgeon’s perspectives. Korean J Otorhinolaryngol-Head Neck Surg. 2016; Jan. 59(1):1–8.
Article131. Isshiki N, Okamura H, Ishikawa T. Thyroplasty type I (lateral compression) for dysphonia due to vocal cord paralysis or atrophy. Acta Otolaryngol. 1975; Nov-Dec. 80(5-6):465–73.
Article132. McCulloch TM, Hoffman HT, Andrews BT, Karnell MP. Arytenoid adduction combined with Gore-Tex medialization thyroplasty. Laryngoscope. 2000; Aug. 110(8):1306–11.
Article133. Aynehchi BB, McCoul ED, Sundaram K. Systematic review of laryngeal reinnervation techniques. Otolaryngol Head Neck Surg. 2010; Dec. 143(6):749–59.
Article134. Paniello RC. Laryngeal reinnervation. Otolaryngol Clin North Am. 2004; Feb. 37(1):161–81.
Article135. Hong JW, Roh TS, Yoo HS, Hong HJ, Choi HS, Chang HS, et al. Outcome with immediate direct anastomosis of recurrent laryngeal nerves injured during thyroidectomy. Laryngoscope. 2014; Jun. 124(6):1402–8.
Article136. Sanuki T, Yumoto E, Minoda R, Kodama N. The role of immediate recurrent laryngeal nerve reconstruction for thyroid cancer surgery. J Oncol. 2010; 2010:846235.
Article137. Wang W, Chen D, Chen S, Li D, Li M, Xia S, et al. Laryngeal reinnervation using ansa cervicalis for thyroid surgery-related unilateral vocal fold paralysis: a long-term outcome analysis of 237 cases. PLoS One. 2011; Apr. 6(4):e19128.
Article138. Eadie TL, Kapsner M, Rosenzweig J, Waugh P, Hillel A, Merati A. The role of experience on judgments of dysphonia. J Voice. 2010; Sep. 24(5):564–73.
Article139. Lacoste L, Karayan J, Lehuede MS, Thomas D, Goudou-Sinha M, Ingrand P, et al. A comparison of direct, indirect, and fiberoptic laryngoscopy to evaluate vocal cord paralysis after thyroid surgery. Thyroid. 1996; Feb. 6(1):17–21.
Article140. Dionigi G, Boni L, Rovera F, Rausei S, Castelnuovo P, Dionigi R. Postoperative laryngoscopy in thyroid surgery: proper timing to detect recurrent laryngeal nerve injury. Langenbecks Arch Surg. 2010; Apr. 395(4):327–31.
Article141. Bures C, Bobak-Wieser R, Koppitsch C, Klatte T, Zielinski V, Freissmuth M, et al. Late-onset palsy of the recurrent laryngeal nerve after thyroid surgery. Br J Surg. 2014; Nov. 101(12):1556–9.
Article142. Friedman AD, Burns JA, Heaton JT, Zeitels SM. Early versus late injection medialization for unilateral vocal cord paralysis. Laryngoscope. 2010; Oct. 120(10):2042–6.
Article143. Yung KC, Likhterov I, Courey MS. Effect of temporary vocal fold injection medialization on the rate of permanent medialization laryngoplasty in unilateral vocal fold paralysis patients. Laryngoscope. 2011; Oct. 121(10):2191–4.
Article144. Stojadinovic A, Shaha AR, Orlikoff RF, Nissan A, Kornak MF, Singh B, et al. Prospective functional voice assessment in patients undergoing thyroid surgery. Ann Surg. 2002; Dec. 236(6):823–32.
Article145. Page C, Zaatar R, Biet A, Strunski V. Subjective voice assessment after thyroid surgery: a prospective study of 395 patients. Indian J Med Sci. 2007; Aug. 61(8):448–54.
Article146. Boone DR, McFarlane SC, Von Berg SL, Zraick RI. The voice and voice therapy. 10th ed. Hoboken: Pearson Education;2019.147. Tedla M, Chakrabarti S, Suchankova M, Weickert MO. Voice outcomes after thyroidectomy without superior and recurrent laryngeal nerve injury: VoiSS questionnaire and GRBAS tool assessment. Eur Arch Otorhinolaryngol. 2016; Dec. 273(12):4543–7.
Article148. Sung E, Lee JC, Song CM, Ji Y, Tae K. Long-term serial follow-up of voice outcome after thyroidectomy. Otolaryngol Head Neck Surg. 2016; Sep. 155(S1):P171.149. Debruyne F, Ostyn F, Delaere P, Wellens W, Decoster W. Temporary voice changes after uncomplicated thyroidectomy. Acta Otorhinolaryngol Belg. 1997; 51(3):137–40.150. Shonka DC Jr, Terris DJ. The American Thyroid Association guidelines on voice assessment: have we done enough. JAMA Otolaryngol Head Neck Surg. 2016; Feb. 142(2):115–6.
Article151. Sorensen JR, Dossing H, Bonnema SJ, Hegedus L, Printz T, Godballe C. Voice changes after thyroidectomy impacts quality of life. Otolaryngol Head Neck Surg. 2017; Sep. 157(S1):P171.152. Lee SJ, Lim SE, Choi HS. Responsiveness of the Korean version of the Voice Activity and Participation Profile (K-VAPP) after surgical intervention. Commun Sci Disord. 2017; 22(2):379–90.
Article153. Lee SJ, Choi HS, Kim H, Byeon HK, Lim SE, Yang MK, et al. Korean version of the Voice Activity and Participation Profile (K-VAPP): a validation study. Commun Sci Disord. 2016; Dec. 21(4):695–708.
Article154. Lang BH, Wong CK, Ma EP. A systematic review and meta-analysis on acoustic voice parameters after uncomplicated thyroidectomy. Laryngoscope. 2016; Feb. 126(2):528–37.
Article155. Minni A, Ruoppolo G, Barbaro M, Di Lorenzo E, Sementilli G, Bononi M. Long-term (12 to 18 months) functional voice assessment to detect voice alterations after thyroidectomy. Eur Rev Med Pharmacol Sci. 2014; 18(12):1704–8.156. Ortega J, Cassinello N, Dorcaratto D, Leopaldi E. Computerized acoustic voice analysis and subjective scaled evaluation of the voice can avoid the need for laryngoscopy after thyroid surgery. Surgery. 2009; Mar. 145(3):265–71.
Article157. Solomon NP, Awan SN, Helou LB, Stojadinovic A. Acoustic analyses of thyroidectomy-related changes in vowel phonation. J Voice. 2012; Nov. 26(6):711–20.
Article158. Iyomasa RM, Tavares EL, Castilho EC, Veloso IL, Tagliarini JV, Martins RH. Videolaryngoscopy, vocal symptoms assessment, and voice acoustic features in patients undergoing thyroid surgery. Int Arch Otorhinolaryngol. 2014; 18:a2450.
Article159. Dixon H, Amin N, Roplekar R, Lindisfarne E, Gibbins N, Harries M. Assessment of voice in thyroidectomy patients: an audit cycle. Otorhinolaryngologist. 2013; 6(2):122–4.160. Kletzien H, Macdonald CL, Orne J, Francis DO, Leverson G, Wendt E, et al. Comparison between patient-perceived voice changes and quantitative voice measures in the first postoperative year after thyroidectomy: a secondary analysis of a randomized clinical trial. JAMA Otolaryngol Head Neck Surg. 2018; Nov. 144(11):995–1003.
Article161. Lee SJ, Lim SE, Choi HS. A comparison of cepstral and spectral measures according to measurement position in a reading passage. Commun Sci Disord. 2017; Dec. 22(4):818–26.
Article162. Lee SJ, Pyo HY, Choi HS. Normative data of cepstral and spectral measures in Korean adults using vowel phonation and passage reading tasks. Commun Sci Disord. 2018; Mar. 23(1):208–17.
Article163. Yu M, Choi SH, Choi CH, Choi B. Predicting normal and pathological voice using a cepstral based acoustic index in sustained vowels versus connected speech. Commun Sci Disord. 2018; Dec. 23(4):1055–64.
Article164. Desuter G, Dedry M, Schaar B, van Lith-Bijl J, van Benthem PP, Sjogren EV. Voice outcome indicators for unilateral vocal fold paralysis surgery: a review of the literature. Eur Arch Otorhinolaryngol. 2018; Feb. 275(2):459–68.
Article165. Lo CY, Kwok KF, Yuen PW. A prospective evaluation of recurrent laryngeal nerve paralysis during thyroidectomy. Arch Surg. 2000; Feb. 135(2):204–7.
Article166. Affleck BD, Swartz K, Brennan J. Surgical considerations and controversies in thyroid and parathyroid surgery. Otolaryngol Clin North Am. 2003; Feb. 36(1):159–87.
Article167. Lee DH, Lee SY, Lee M, Seok J, Park SJ, Jin YJ, et al. Natural course of unilateral vocal fold paralysis and optimal timing of permanent treatment. JAMA Otolaryngol Head Neck Surg. 2020; Jan. 146(1):30–5.
Article168. Husain S, Sadoughi B, Mor N, Levin AM, Sulica L. Time course of recovery of idiopathic vocal fold paralysis. Laryngoscope. 2018; Jan. 128(1):148–52.
Article169. Mau T, Pan HM, Childs LF. The natural history of recoverable vocal fold paralysis: implications for kinetics of reinnervation. Laryngoscope. 2017; Nov. 127(11):2585–90.
Article170. Sulica L. The natural history of idiopathic unilateral vocal fold paralysis: evidence and problems. Laryngoscope. 2008; Jul. 118(7):1303–7.
Article171. Vila PM, Bhatt NK, Paniello RC. Early-injection laryngoplasty may lower risk of thyroplasty: a systematic review and meta-analysis. Laryngoscope. 2018; Apr. 128(4):935–40.
Article172. Lee SW, Kim JW, Chung CH, Mok JO, Shim SS, Koh YW, et al. Utility of injection laryngoplasty in the management of post-thyroidectomy vocal cord paralysis. Thyroid. 2010; May. 20(5):513–7.
Article173. Halderman AA, Bryson PC, Benninger MS, Chota R. Safety and length of benefit of restylane for office-based injection medialization-a retrospective review of one institution’s experience. J Voice. 2014; Sep. 28(5):631–5.
Article174. Silva Merea V, Husain S, Sulica L. Medialization laryngoplasty after injection augmentation. J Voice. 2018; Mar. 32(2):249–55.
Article175. Vinson KN, Zraick RI, Ragland FJ. Injection versus medialization laryngoplasty for the treatment of unilateral vocal fold paralysis: follow-up at six months. Laryngoscope. 2010; Sep. 120(9):1802–7.
Article176. Morgan JE, Zraick RI, Griffin AW, Bowen TL, Johnson FL. Injection versus medialization laryngoplasty for the treatment of unilateral vocal fold paralysis. Laryngoscope. 2007; Nov. 117(11):2068–74.
Article177. Shen T, Damrose EJ, Morzaria S. A meta-analysis of voice outcome comparing calcium hydroxylapatite injection laryngoplasty to silicone thyroplasty. Otolaryngol Head Neck Surg. 2013; Feb. 148(2):197–208.
Article178. Fang TJ, Pei YC, Li HY, Wong AM, Chiang HC. Glottal gap as an early predictor for permanent laryngoplasty in unilateral vocal fold paralysis. Laryngoscope. 2014; Sep. 124(9):2125–30.
Article179. Nouwen J, Hans S, De Mones E, Brasnu D, Crevier-Buchman L, Laccourreye O. Thyroplasty type I without arytenoid adduction in patients with unilateral laryngeal nerve paralysis: the montgomery implant versus the Gore-Tex implant. Acta Otolaryngol. 2004; Aug. 124(6):732–8.
Article180. Elnashar I, El-Anwar M, Amer H, Quriba A. Voice outcome after Gore-Tex medialization thyroplasty. Int Arch Otorhinolaryngol. 2015; Jul. 19(3):248–54.
Article181. Storck C, Brockmann M, Schnellmann E, Stoeckli SJ, Schmid S. Functional outcome of vocal fold medialization thyroplasty with a hydroxyapatite implant. Laryngoscope. 2007; Jun. 117(6):1118–22.
Article182. Young VN, Zullo TG, Rosen CA. Analysis of laryngeal framework surgery: 10-year follow-up to a national survey. Laryngoscope. 2010; Aug. 120(8):1602–8.
Article183. Hess M, Schroeder D, Puschel K. Sling arytenoid adduction. Eur Arch Otorhinolaryngol. 2011; Jul. 268(7):1023–8.
Article184. Chester MW, Stewart MG. Arytenoid adduction combined with medialization thyroplasty: an evidence-based review. Otolaryngol Head Neck Surg. 2003; Oct. 129(4):305–10.
Article185. Mortensen M, Carroll L, Woo P. Arytenoid adduction with medialization laryngoplasty versus injection or medialization laryngoplasty: the role of the arytenoidopexy. Laryngoscope. 2009; Apr. 119(4):827–31.
Article186. Chang J, Schneider SL, Curtis J, Langenstein J, Courey MS, Yung KC. Outcomes of medialization laryngoplasty with and without arytenoid adduction. Laryngoscope. 2017; Nov. 127(11):2591–5.
Article187. Li AJ, Johns MM, Jackson-Menaldi C, Dailey S, Heman-Ackah Y, Merati A, et al. Glottic closure patterns: type I thyroplasty versus type I thyroplasty with arytenoid adduction. J Voice. 2011; May. 25(3):259–64.
Article188. Feehery JM, Pribitkin EA, Heffelfinger RN, Lacombe VG, Lee D, Lowry LD, et al. The evolving etiology of bilateral vocal fold immobility. J Voice. 2003; Mar. 17(1):76–81.
Article189. Rosenthal LH, Benninger MS, Deeb RH. Vocal fold immobility: a longitudinal analysis of etiology over 20 years. Laryngoscope. 2007; Oct. 117(10):1864–70.
Article190. Pinto JA, Godoy LB, Marquis VW, Sonego TB, Leal Cde F. Bilateral vocal fold immobility: diagnosis and treatment. Braz J Otorhinolaryngol. 2011; Sep-Oct. 77(5):594–9.
Article191. Bogdasarian RS, Olson NR. Posterior glottic laryngeal stenosis. Otolaryngol Head Neck Surg (1979). 1980; Nov-Dec. 88(6):765–72.
Article192. Andrade Filho PA, Rosen CA. Bilateral vocal fold paralysis: an unusual treatment with botulinum toxin. J Voice. 2004; Jun. 18(2):254–5.193. Nawka T, Sittel C, Arens C, Lang-Roth R, Wittekindt C, Hagen R, et al. Voice and respiratory outcomes after permanent transoral surgery of bilateral vocal fold paralysis. Laryngoscope. 2015; Dec. 125(12):2749–55.
Article194. Li Y, Garrett G, Zealear D. Current treatment options for bilateral vocal fold paralysis: a state-of-the-art review. Clin Exp Otorhinolaryngol. 2017; Sep. 10(3):203–12.
Article195. Su WF, Liu SC, Tang WS, Yang MC, Lin YY, Huang TT. Suture lateralization in patients with bilateral vocal fold paralysis. J Voice. 2014; Sep. 28(5):644–51.
Article196. Ozdemir S, Tuncer U, Tarkan O, Kara K, Surmelioglu O. Carbon dioxide laser endoscopic posterior cordotomy technique for bilateral abductor vocal cord paralysis: a 15-year experience. JAMA Otolaryngol Head Neck Surg. 2013; Apr. 139(4):401–4.
Article197. Szakacs L, Sztano B, Matievics V, Bere Z, Bach A, Castellanos PF, et al. A comparison between transoral glottis-widening techniques for bilateral vocal fold immobility. Laryngoscope. 2015; Nov. 125(11):2522–9.
Article198. Yilmaz T. Endoscopic partial arytenoidectomy for bilateral vocal fold paralysis: medially based mucosal flap technique. J Voice. 2019; Sep. 33(5):751–8.
Article199. Rodriguez-Torres J, Lopez-Lopez L, Cabrera-Martos I, Torres-Sanchez I, Ortiz-Rubio A, Valenza MC. Musculoskeletal neck disorders in thyroid cancer patients after thyroidectomy. Eur J Cancer Care (Engl). 2019; Jul. 28(4):e13053.200. Lang BH, Ng SH, Wong KP. Pain and surgical outcomes with and without neck extension in standard open thyroidectomy: a prospective randomized trial. Head Neck. 2015; Mar. 37(3):407–12.
Article201. Takamura Y, Miyauchi A, Tomoda C, Uruno T, Ito Y, Miya A, et al. Stretching exercises to reduce symptoms of postoperative neck discomfort after thyroid surgery: prospective randomized study. World J Surg. 2005; Jun. 29(6):775–9.
Article202. Lombardi CP, Raffaelli M, D’Alatri L, Marchese MR, Rigante M, Paludetti G, et al. Voice and swallowing changes after thyroidectomy in patients without inferior laryngeal nerve injuries. Surgery. 2006; Dec. 140(6):1026–32.
Article203. Lombardi CP, Raffaelli M, De Crea C, D’Alatri L, Maccora D, Marchese MR, et al. Long-term outcome of functional post-thyroidectomy voice and swallowing symptoms. Surgery. 2009; Dec. 146(6):1174–81.
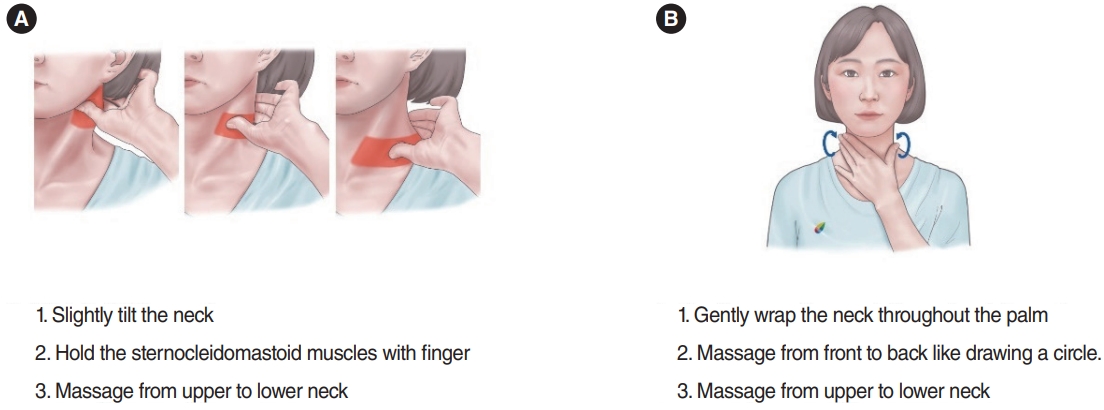
Article204. Lee JS, Kim JP, Ryu JS, Woo SH. Effect of wound massage on neck discomfort and voice changes after thyroidectomy. Surgery. 2018; Nov. 164(5):965–71.
Article205. Ayhan H, Tastan S, Iyigun E, Ozturk E, Yildiz R, Gorgulu S. The effectiveness of neck stretching exercises following total thyroidectomy on reducing neck pain and disability: a randomized controlled trial. Worldviews Evid Based Nurs. 2016; Jun. 13(3):224–31.
Article206. Kim K, Gu MO, Jung JH, Hahm JR, Kim SK, Kim JH, et al. Efficacy of a home-based exercise program after thyroidectomy for thyroid cancer patients. Thyroid. 2018; Feb. 28(2):236–45.
Article207. Genc A, Celik SU, Genc V, Gokmen D, Tur BS. The effects of cervical kinesiotaping on neck pain, range of motion, and disability in patients following thyroidectomy: a randomized, double-blind, sham-controlled clinical trial. Turk J Med Sci. 2019; Aug. 49(4):1185–91.
Article208. Stachler RJ, Francis DO, Schwartz SR, Damask CC, Digoy GP, Krouse HJ, et al. Clinical practice guideline: hoarseness (dysphonia) (update). Otolaryngol Head Neck Surg. 2018; Mar. 158(1_ suppl):S1–42.
Article209. Yu WV, Wu CW. Speech therapy after thyroidectomy. Gland Surg. 2017; Oct. 6(5):501–9.
Article210. Guzman M, Castro C, Madrid S, Olavarria C, Leiva M, Munoz D, et al. Air pressure and contact quotient measures during different semioccluded postures in subjects with different voice conditions. J Voice. 2016; Nov. 30(6):759.e1–759.e10.211. Heuer RJ, Sataloff RT, Emerich K, Rulnick R, Baroody M, Spiegel JR, et al. Unilateral recurrent laryngeal nerve paralysis: the importance of “preoperative” voice therapy. J Voice. 1997; Mar. 11(1):88–94.
Article212. Isshiki N. Mechanical and dynamic aspects of voice production as related to voice therapy and phonosurgery. Otolaryngol Head Neck Surg. 2000; Jun. 122(6):782–93.
Article213. Schindler A, Bottero A, Capaccio P, Ginocchio D, Adorni F, Ottaviani F. Vocal improvement after voice therapy in unilateral vocal fold paralysis. J Voice. 2008; Jan. 22(1):113–8.
Article214. Mattioli F, Menichetti M, Bergamini G, Molteni G, Alberici MP, Luppi MP, et al. Results of early versus intermediate or delayed voice therapy in patients with unilateral vocal fold paralysis: our experience in 171 patients. J Voice. 2015; Jul. 29(4):455–8.
Article215. Ptok M, Strack D. Electrical stimulation-supported voice exercises are superior to voice exercise therapy alone in patients with unilateral recurrent laryngeal nerve paresis: results from a prospective, randomized clinical trial. Muscle Nerve. 2008; Aug. 38(2):1005–11.
Article216. Anderson SK, Terris DJ. Complications of endoscopic neck surgery. In : Eisele DW, Smith RV, editors. Complications in head and neck surgery. 2nd ed. Philadelphia (PA): Mosby;2009. p. 467–75.217. Nam IC, Bae JS, Chae BJ, Shim MR, Hwang YS, Sun DI. Therapeutic approach to patients with a lower-pitched voice after thyroidectomy. World J Surg. 2013; Aug. 37(8):1940–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Voice Care for the Post-Thyroidectomy Dysphonia
- Perioperative Management of the Voice in Thyroid Cancer
- The SLP's Perspectives for the Vocal Elites and Singing Voice
- A Case of Voice Therapy for Patient Who Voice Changed after Total Thyroidectomy Using Contactless Voice and Speech Therapy Service Platform
- A Case of Voice Therapy for Post-Thyroidectomy Syndrome