Ann Surg Treat Res.
2022 Mar;102(3):159-166. 10.4174/astr.2022.102.3.159.
Learning curve for single-port robot-assisted rectal cancer surgery
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2526937
- DOI: http://doi.org/10.4174/astr.2022.102.3.159
Abstract
- Purpose
We analyzed the learning curve of single-port robotic (SPR)-assisted rectal cancer surgery.
Methods
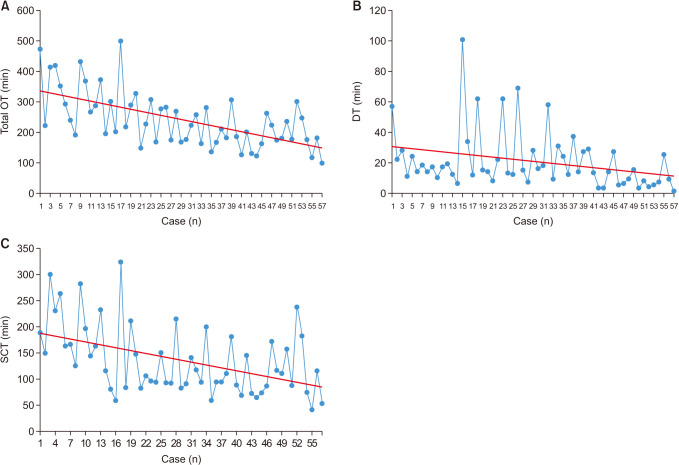
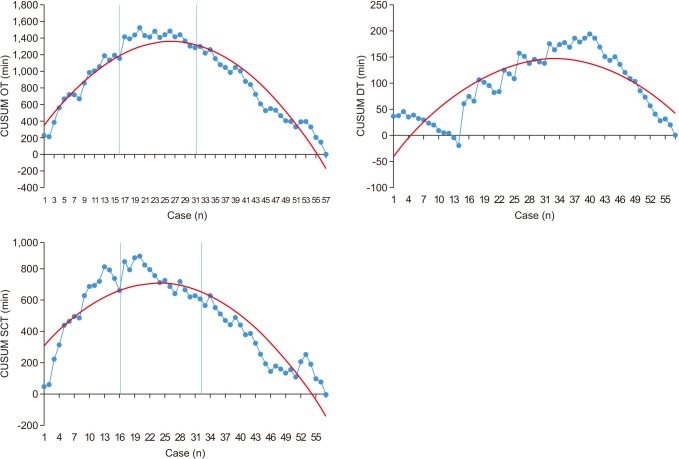
Fifty-seven consecutive SPR-assisted rectal cancer surgery cases performed by the same surgeon were considered in surgical interventions for rectal cancer. Total operation time (OT), docking time (DT), and surgeon console time (SCT) measured during surgery were used to parametrize the learning curve. The parameters representing the learning curve were evaluated using the cumulative sum (CUSUM).
Results
The mean value of total OT was 241.8 ± 91.7 minutes, the mean value of DT was 20.6 ± 19.1 minutes, and the mean value of SCT was 135.9 ± 66.7 minutes. The learning curve was divided into phase 1 (initial 16 cases), phase 2 (second 16 cases), and phase 3 (subsequent 25 cases). The peak on the CUSUM graph occurred in the 21st case. The longest OT among phases was in phase 2. Complications were most frequent in phase 2. However, complications of Clavien-Dindo (CD) grade IIIb were most frequent in phase 3 with 2 patients. The most common complications were fluid collection and urinary retention (7 patients each). Complications of CD grade IIIb required one stomal revision due to stoma obstruction and one irrigation and loop ileostomy due to anastomosis leakage.
Conclusion
Improvement in surgical performance of SPR assisted rectal cancer operation was achieved after 21 cases. The three phases identified in the cumulative sum analysis showed a significant decrease in operative time after the middle stage of the learning curve without an increase in the complication rate.
Figure
Cited by 1 articles
-
Single-port
versus multiport robotic total mesorectal excision for rectal cancer: initial experiences by case-matched analysis of short-term outcomes
Min Hye Jeong, Hye Jin Kim, Gyu-Seog Choi, Seung Ho Song, Jun Seok Park, Soo Yeun Park, Sung Min Lee, Dong Hee Na
Ann Surg Treat Res. 2023;105(2):99-106. doi: 10.4174/astr.2023.105.2.99.
Reference
-
1. Buess G, Manncke K, Merhan J, Lirici M. State of the art of laparoscopic colorectal surgery. Endosc Surg Allied Technol. 1993; 1:3–12. PMID: 8050007.2. Remzi FH, Kirat HT, Kaouk JH, Geisler DP. Single-port laparoscopy in colorectal surgery. Colorectal Dis. 2008; 10:823–826. PMID: 18684153.
Article3. Pigazzi A, Ellenhorn JD, Ballantyne GH, Paz IB. Robotic-assisted laparoscopic low anterior resection with total mesorectal excision for rectal cancer. Surg Endosc. 2006; 20:1521–1525. PMID: 16897284.
Article4. Park SJ, Lee KY, Lee SH. Laparoscopic surgery for colorectal cancer in Korea: nationwide data from 2013 to 2018. Cancer Res Treat. 2020; 52:938–944. PMID: 32252138.
Article5. Hazebroek EJ. Color Study Group. COLOR: a randomized clinical trial comparing laparoscopic and open resection for colon cancer. Surg Endosc. 2002; 16:949–953. PMID: 12163961.6. Dobbs RW, Halgrimson WR, Madueke I, Vigneswaran HT, Wilson JO, Crivellaro S. Single-port robot-assisted laparoscopic radical prostatectomy: initial experience and technique with the da Vinci® SP platform. BJU Int. 2019; 124:1022–1027. PMID: 31301693.
Article7. Marks JH, Salem JF, Anderson BK, Josse JM, Schoonyoung HP. Single-port robotic left colectomy: first clinical experience using the SP robot (rSILS). Tech Coloproctol. 2020; 24:57–63. PMID: 31832798.
Article8. Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM. Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc. 2011; 25:855–860. PMID: 20734081.
Article9. Jiménez-Rodríguez RM, Díaz-Pavón JM, de la Portilla de Juan F, Prendes-Sillero E, Dussort HC, Padillo J. Learning curve for robotic-assisted laparoscopic rectal cancer surgery. Int J Colorectal Dis. 2013; 28:815–821. PMID: 23242270.
Article10. Park EJ, Kim CW, Cho MS, Kim DW, Min BS, Baik SH, et al. Is the learning curve of robotic low anterior resection shorter than laparoscopic low anterior resection for rectal cancer?: a comparative analysis of clinicopathologic outcomes between robotic and laparoscopic surgeries. Medicine (Baltimore). 2014; 93:e109. PMID: 25437022.11. Jiménez-Rodríguez RM, Rubio-Dorado-Manzanares M, Díaz-Pavón JM, Reyes-Díaz ML, Vazquez-Monchul JM, Garcia-Cabrera AM, et al. Learning curve in robotic rectal cancer surgery: current state of affairs. Int J Colorectal Dis. 2016; 31:1807–1815. PMID: 27714517.
Article12. Nasir M, Panteleimonitis S, Ahmed J, Abbas HM, Parvaiz A. Learning curves in robotic rectal cancer surgery: a literature review. J Minim Invasive Surg Sci. 2016; 5:e41196.
Article13. Steiner SH, Cook RJ, Farewell VT, Treasure T. Monitoring surgical performance using risk-adjusted cumulative sum charts. Biostatistics. 2000; 1:441–452. PMID: 12933566.
Article14. Park Y, Yong YG, Yun SH, Jung KU, Huh JW, Cho YB, et al. Learning curves for single incision and conventional laparoscopic right hemicolectomy: a multidimensional analysis. Ann Surg Treat Res. 2015; 88:269–275. PMID: 25960990.
Article15. Rosman AS, Melis M, Fichera A. Metaanalysis of trials comparing laparoscopic and open surgery for Crohn’s disease. Surg Endosc. 2005; 19:1549–1555. PMID: 16235128.
Article16. Studniarek A, Pan J, Gantt G Jr, Mellgren A, Giulianotti PC, Nordenstam JF. Single-port, robot-assisted transanal excision of rectal lesion. Dis Colon Rectum. 2021; 64:e25. PMID: 33417348.
Article17. Park JW, Sohn DK, Park S, Park SC, Chang HJ, Son HJ, et al. Safety and efficacy of single-port colectomy for sigmoid colon cancer: a phase II clinical trial. J Laparoendosc Adv Surg Tech A. 2013; 23:745–750. PMID: 23937142.
Article18. Park SJ, Lee KY, Kang BM, Choi SI, Lee SH. Initial experience of single-port laparoscopic surgery for sigmoid colon cancer. World J Surg. 2013; 37:652–656. PMID: 23232821.
Article19. Arteaga González I, Martín Malagón A, Garcia SG, Fernández EM, Pallares AC. Single-incision laparoscopic surgery for colon and rectal cancer: an initial experience with the technique. Surg Laparosc Endosc Percutan Tech. 2013; 23:494–497. PMID: 24300924.20. Hamabe A, Takemasa I, Uemura M, Nishimura J, Mizushima T, Ikeda M, et al. Feasibility of single-port laparoscopic surgery for sigmoid colon and rectal cancers and preoperative assessment of operative difficulty. J Gastrointest Surg. 2014; 18:977–985. PMID: 24470062.
Article21. Bae SU, Jeong WK, Baek SK. Single-port plus an additional port robotic complete mesocolic excision and intracorporeal anastomosis using a robotic stapler for right-sided colon cancer. Ann Surg Treat Res. 2016; 91:212–217. PMID: 27757400.
Article22. Bae SU, Jeong WK, Bae OS, Baek SK. Reduced-port robotic anterior resection for left-sided colon cancer using the Da Vinci single-site(®) platform. Int J Med Robot. 2016; 12:517–523. PMID: 26099476.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of intraoperative and short-term postoperative outcomes between robot-assisted laparoscopic multi-port pyeloplasty using the da Vinci Si system and single-port pyeloplasty using the da Vinci SP system in children
- Learning curve for single-port robot-assisted colectomy
- Robot-Assisted Thoracic Surgery in Non-small Cell Lung Cancer
- Learning curve analysis of robot-assisted radical hysterectomy for cervical cancer: initial experience at a single institution
- Robotic harvest of a latissimus dorsi flap using a single-port surgical robotic system in breast reconstruction