J Korean Assoc Oral Maxillofac Surg.
2022 Feb;48(1):63-67. 10.5125/jkaoms.2022.48.1.63.
A new rationale for preservation of the mandibular third molar in orthognathic patients with missing molars
- Affiliations
-
- 1Private Practice, Seoul, Korea
- 2Department of Orthodontics, Korea University Anam Hospital, Seoul, Korea
- 3Department of Orthodontics, Institute of Oral Health Science, Ajou University School of Medicine, Suwon, Korea
- 4Department of Oral and Maxillofacial Surgery, Seoul St. Mary’s Hospital, Catholic University of Korea, Seoul, Korea
- 5Orthodontics and Maxillary Orthopedics, University of Salvador, Buenos Aires, Argentina
- 6SAS Orthodontic Centre, Ichiban-Cho Dental Clinic, Sendai, Japan
- 7Department of Oral and Maxillofacial Surgery, Dental Center, Chung-Ang University Hospital, Seoul, Korea
- KMID: 2526812
- DOI: http://doi.org/10.5125/jkaoms.2022.48.1.63
Abstract
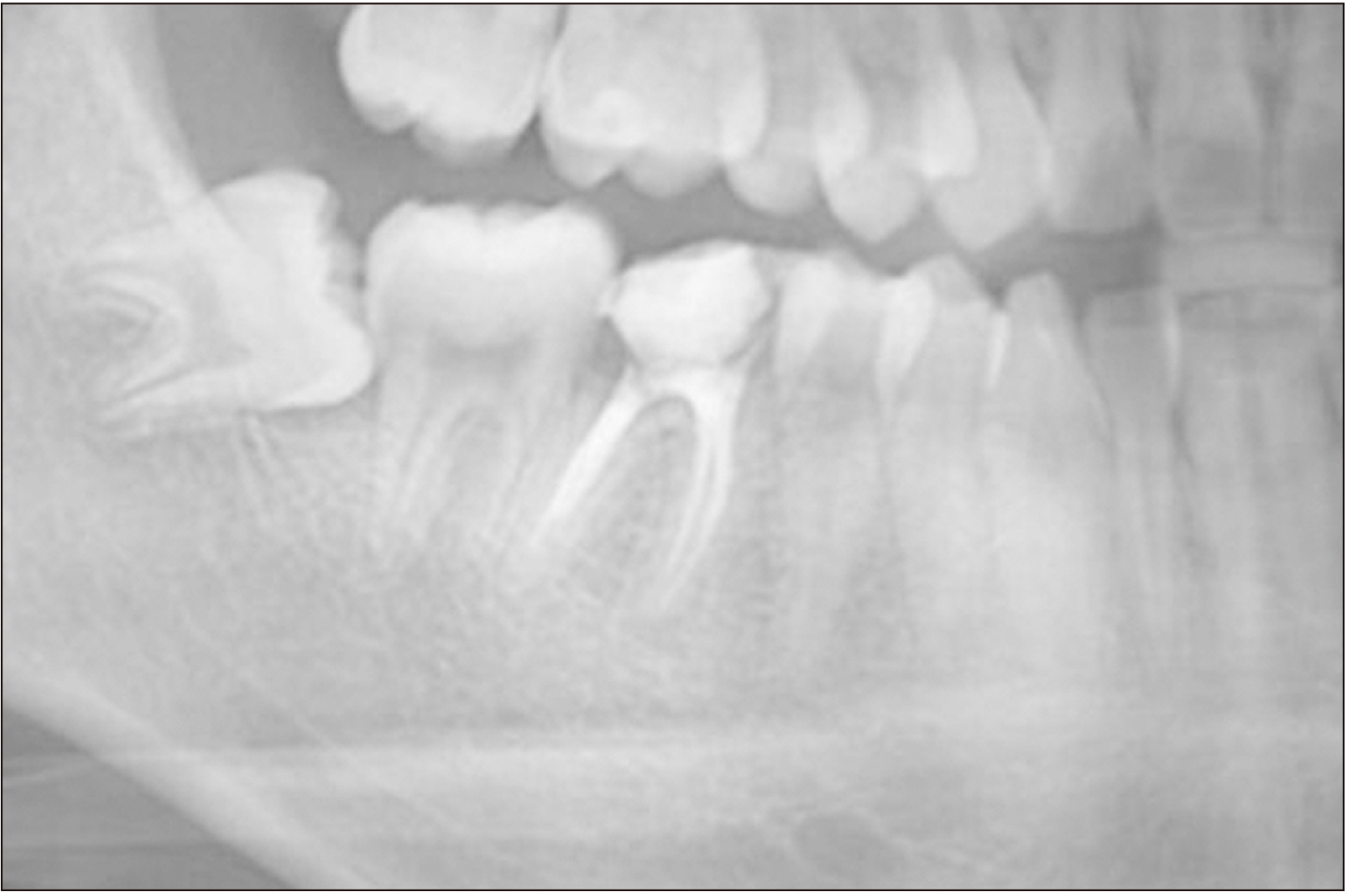
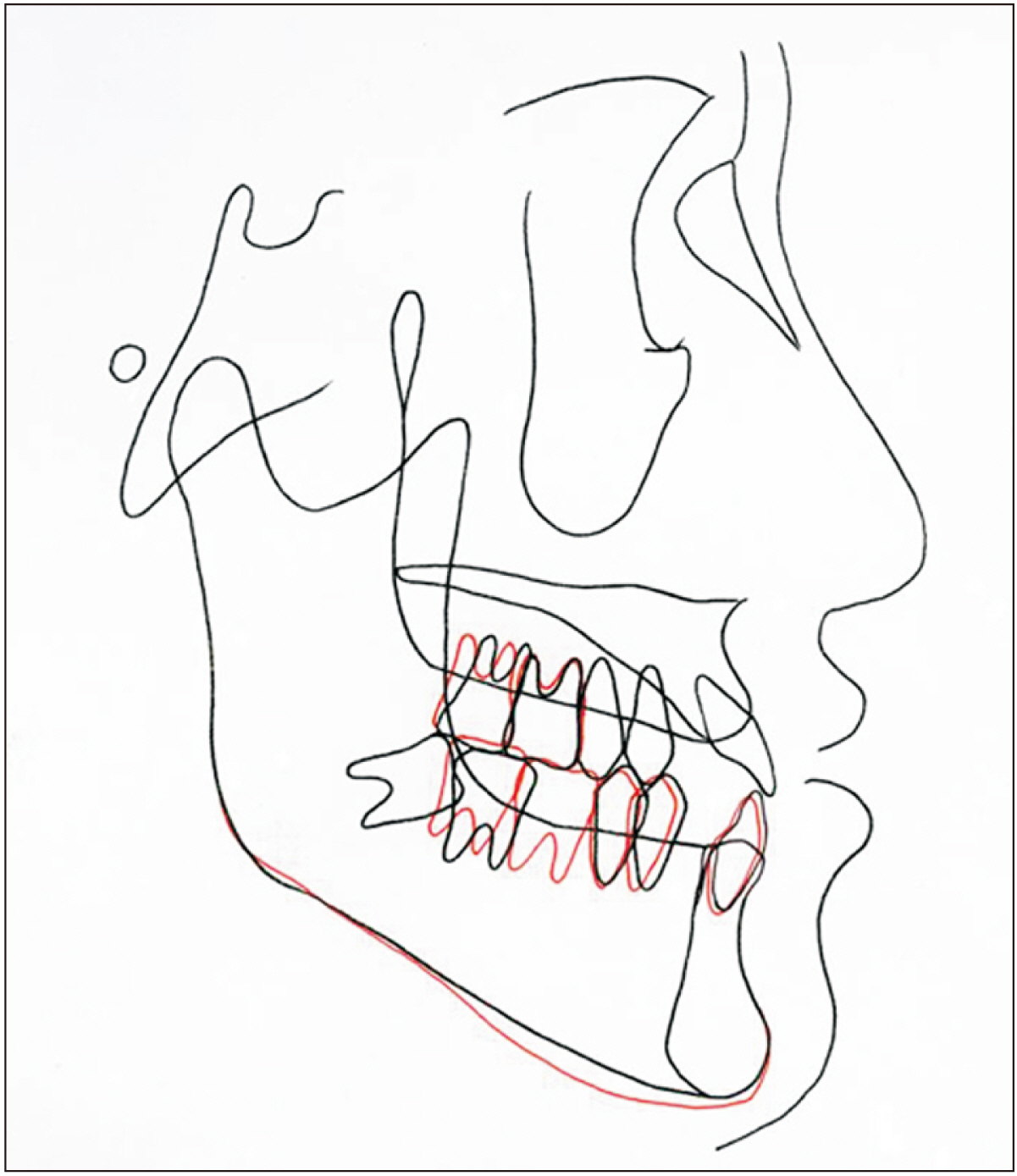
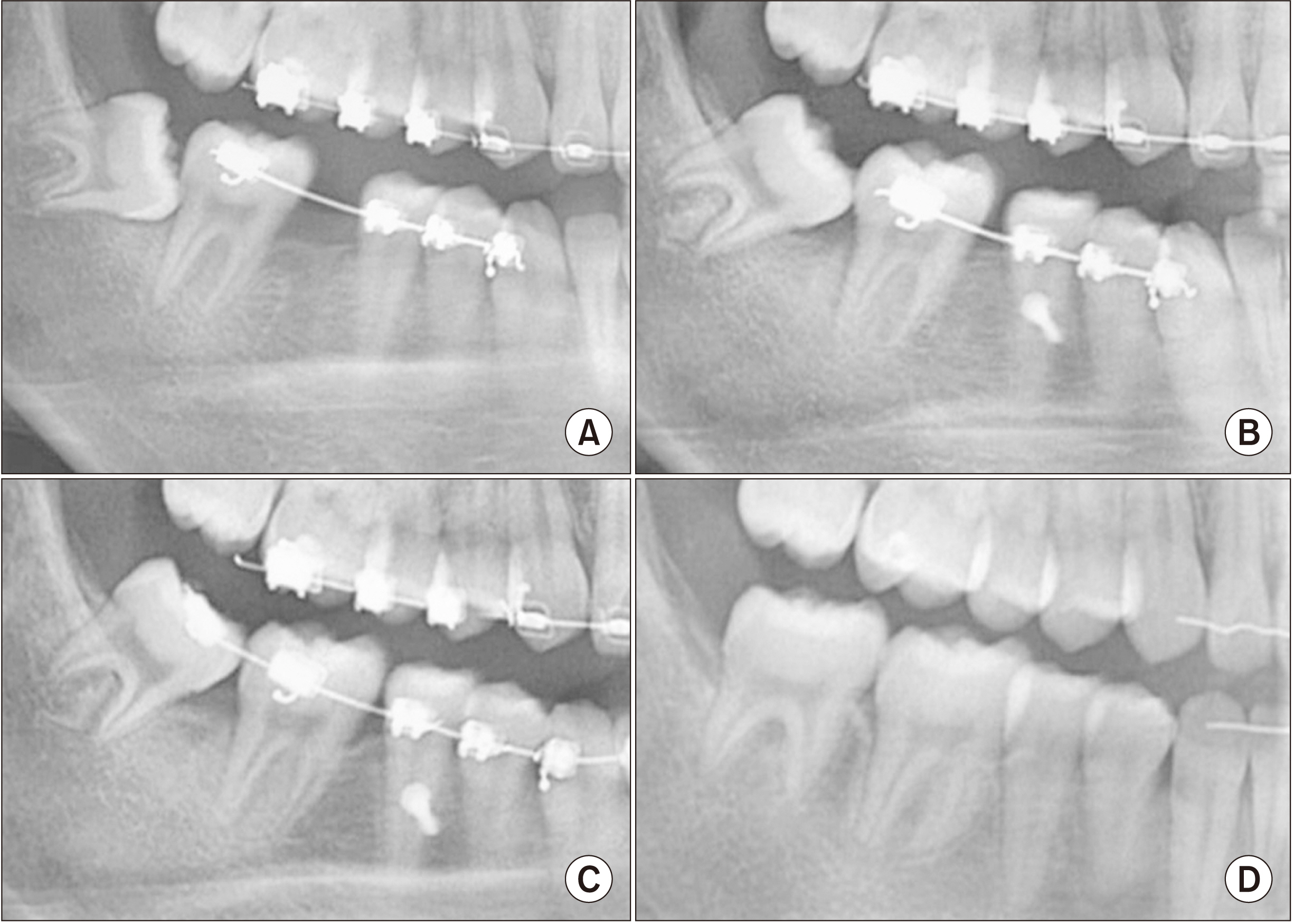
- Controversies exist regarding the need for prophylactic extraction of mandibular third molars in patients who plan to undergo orthognathic surgery. An 18-year-old male patient was diagnosed with mandibular prognathism and maxillary retrognathism with mild facial asymmetry. He had a severely damaged mandibular first molar and a horizontally impacted third molar. After extraction of the first molar, the second molar was protracted into the first molar space, and the third molar erupted into the posterior line of occlusion. The orthognathic surgery involved clockwise rotation of the maxillomandibular complex as well as angle shaving and chin border trimming. Patients who are missing or have damaged mandibular molars should be monitored for eruption of third molars to replace the missing posterior tooth regardless of the timing of orthognathic surgery.
Keyword
Figure
Reference
-
References
1. Colelia G, Giudice A. 2003; The timing of third molar removal in patients undergoing a bilateral sagittal split osteotomy. J Oral Maxillofac Surg. 61:975. https://doi.org/10.1016/s0278-2391(03)00505-6. DOI: 10.1016/S0278-2391(03)00505-6. PMID: 12908480.
Article2. Mehra P, Castro V, Freitas RZ, Wolford LM. 2001; Complications of the mandibular sagittal split ramus osteotomy associated with the presence or absence of third molars. J Oral Maxillofac Surg. 59:854–8. discussion 859. https://doi.org/10.1053/joms.2001.25013. DOI: 10.1053/joms.2001.25013. PMID: 11474434.
Article3. Reyneke JP, Tsakiris P, Becker P. 2002; Age as a factor in the complication rate after removal of unerupted/impacted third molars at the time of mandibular sagittal split osteotomy. J Oral Maxillofac Surg. 60:654–9. https://doi.org/10.1053/joms.2002.33114. DOI: 10.1053/joms.2002.33114. PMID: 12022103.
Article4. Van Sickels JE, Jeter TS, Theriot BA. 1985; Management of an unfavorable lingual fracture during a sagittal split osteotomy. J Oral Maxillofac Surg. 43:808–9. https://doi.org/10.1016/0278-2391(85)90341-6. DOI: 10.1016/0278-2391(85)90341-6. PMID: 3862783.
Article5. Camargo IB, Van Sickels JE, Curtis WJ. 2015; Simultaneous removal of third molars during a sagittal split does not increase the incidence of bad splits in patients aged 30 years or older. J Oral Maxillofac Surg. 73:1350–9. https://doi.org/10.1016/j.joms.2015.01.023. DOI: 10.1016/j.joms.2015.01.023. PMID: 25913510.
Article6. Doucet JC, Morrison AD, Davis BR, Robertson CG, Goodday R, Precious DS. 2012; Concomitant removal of mandibular third molars during sagittal split osteotomy minimizes neurosensory dysfunction. J Oral Maxillofac Surg. 70:2153–63. https://doi.org/10.1016/j.joms.2011.08.029. DOI: 10.1016/j.joms.2011.08.029. PMID: 22079060.
Article7. Schwartz HC. 2004; Simultaneous removal of third molars during sagittal split osteotomies: the case against. J Oral Maxillofac Surg. 62:1147–9. https://doi.org/10.1016/j.joms.2004.04.015. DOI: 10.1016/j.joms.2004.04.015. PMID: 15346369.
Article8. Steinbacher DM, Kontaxis KL. 2016; Does simultaneous third molar extraction increase intraoperative and perioperative complications in orthognathic surgery? J Craniofac Surg. 27:923–6. https://doi.org/10.1097/SCS.0000000000002648. DOI: 10.1097/SCS.0000000000002648. PMID: 27192639.
Article9. McCaul LK, Jenkins WM, Kay EJ. 2001; The reasons for the extraction of various tooth types in Scotland: a 15-year follow up. J Dent. 29:401–7. https://doi.org/10.1016/s0300-5712(01)00036-7. DOI: 10.1016/S0300-5712(01)00036-7. PMID: 11520588.
Article10. Sayegh A, Hilow H, Bedi R. 2004; Pattern of tooth loss in recipients of free dental treatment at the University Hospital of Amman, Jordan. J Oral Rehabil. 31:124–30. https://doi.org/10.1046/j.0305-182x.2003.01229.x. DOI: 10.1046/j.0305-182X.2003.01229.x. PMID: 15009595.
Article11. Baik UB, Kook YA, Bayome M, Park JU, Park JH. 2016; Vertical eruption patterns of impacted mandibular third molars after the mesialization of second molars using miniscrews. Angle Orthod. 86:565–70. https://doi.org/10.2319/061415-399.1. DOI: 10.2319/061415-399.1. PMID: 26438976. PMCID: PMC8601483.
Article12. Kyung SH, Choi JH, Park YC. 2003; Miniscrew anchorage used to protract lower second molars into first molar extraction sites. J Clin Orthod. 37:575–9. PMID: 14617846.13. Baik UB, Chun YS, Jung MH, Sugawara J. 2012; Protraction of mandibular second and third molars into missing first molar spaces for a patient with an anterior open bite and anterior spacing. Am J Orthod Dentofacial Orthop. 141:783–95. https://doi.org/10.1016/j.ajodo.2010.07.031. DOI: 10.1016/j.ajodo.2010.07.031. PMID: 22640680.
Article14. Nagaraj K, Upadhyay M, Yadav S. 2008; Titanium screw anchorage for protraction of mandibular second molars into first molar extraction sites. Am J Orthod Dentofacial Orthop. 134:583–91. https://doi.org/10.1016/j.ajodo.2006.09.055. DOI: 10.1016/j.ajodo.2006.09.055. PMID: 18929277.
Article15. Baik UB. Kim KB, editor. 2014. Molar protraction: orthodontic substitution of missing posterior teeth. Temporary skeletal anchorage devices: a guide to design and evidence-based solution. Springer;Berlin-Heidelberg: p. 119–60. DOI: 10.1007/978-3-642-55052-2_8.
Article16. Jee JH, Ahn HW, Seo KW, Kim SH, Kook YA, Chung KR, et al. 2014; En-masse retraction with a preformed nickel-titanium and stainless steel archwire assembly and temporary skeletal anchorage devices without posterior bonding. Korean J Orthod. 44:236–45. https://doi.org/10.4041/kjod.2014.44.5.236. DOI: 10.4041/kjod.2014.44.5.236. PMID: 25309863. PMCID: PMC4192525.
Article17. Nagasaka H, Sugawara J, Kawamura H, Nanda R. 2009; "Surgery first" skeletal class III correction using the skeletal anchorage system. J Clin Orthod. 43:97–105.18. Baek SH, Ahn HW, Kwon YH, Choi JY. 2010; Surgery-first approach in skeletal class III malocclusion treated with 2-jaw surgery: evaluation of surgical movement and postoperative orthodontic treatment. J Craniofac Surg. 21:332–8. https://doi.org/10.1097/SCS.0b013e3181cf5fd4. DOI: 10.1097/SCS.0b013e3181cf5fd4. PMID: 20186090.
Article19. Liou EJ, Chen PH, Wang YC, Yu CC, Huang CS, Chen YR. 2011; Surgery-first accelerated orthognathic surgery: orthodontic guidelines and setup for model surgery. J Oral Maxillofac Surg. 69:771–80. https://doi.org/10.1016/j.joms.2010.11.011. DOI: 10.1016/j.joms.2010.11.011. PMID: 21257249.
Article20. Yu CC, Chen PH, Liou EJ, Huang CS, Chen YR. 2010; A surgery-first approach in surgical-orthodontic treatment of mandibular prognathism--a case report. Chang Gung Med J. 33:699–705. PMID: 21199616.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of missing and impacted third molars in adults aged 25 years and above
- Proximity of the mandibular molar root apex from the buccal bone surface: a cone-beam computed tomographic study
- A comparative study on crowding according to the status of the third molars in mandibular arch
- The Location of Molar Furcation in Korean
- The role of mandibular third molar in the mandibular angle fractures