J Korean Assoc Oral Maxillofac Surg.
2022 Feb;48(1):59-62. 10.5125/jkaoms.2022.48.1.59.
Intraductal papilloma of the sublingual gland imitating a ranula
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, General Hospital of Thessaloniki "G. Papanikolaou", Pylaia.
- 2Department of Oral and Maxillofacial Surgery, St. Lukes Hospital, Pylaia.
- 3Pathologist, Private Practice, Greece.
- 4Department of Oral and Maxillofacial Surgery, Aristotle University of Thessaloniki, Thessaloniki, Greece.
- KMID: 2526811
- DOI: http://doi.org/10.5125/jkaoms.2022.48.1.59
Abstract
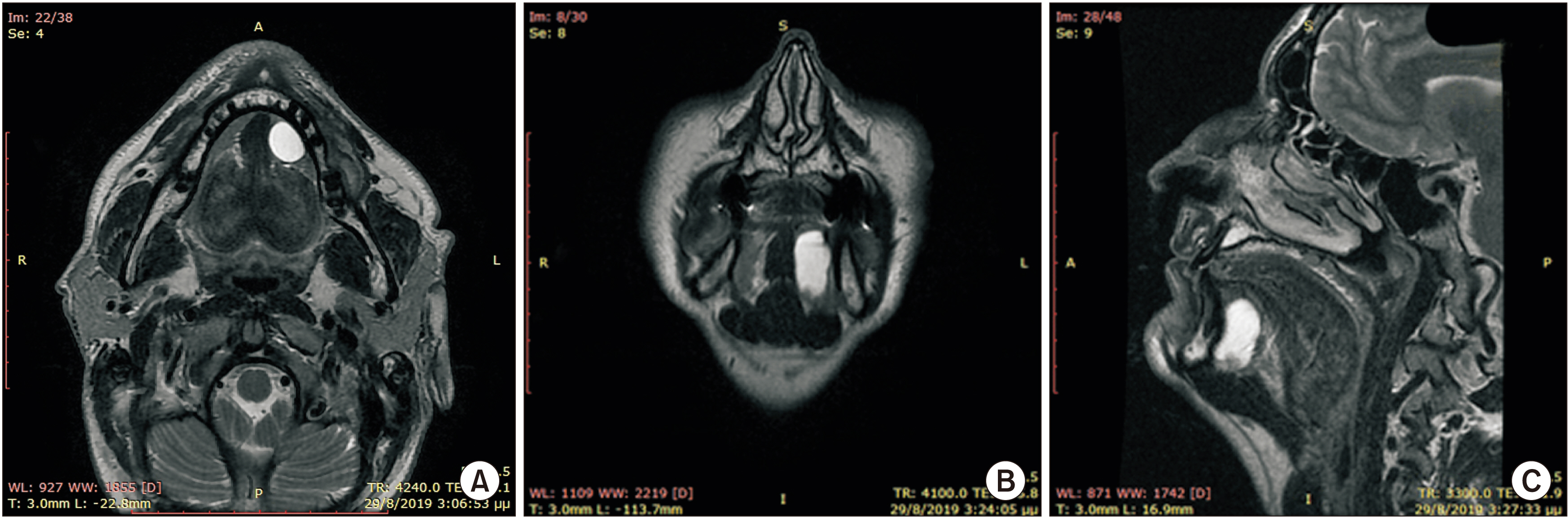
- Ductal papillomas are rare benign lesions of the salivary glands with two distinctive types, intraductal and inverted. The rarest anatomical location where intraductal papillomas occur is the major salivary glands. In the present study, we report an intraductal papilloma of the left sublingual gland with the relevant clinical, imaging, and histopathological findings and postoperative follow-up. To our knowledge, this is the fourth case of an intraductal papilloma of a sublingual gland to be reported in the international literature. We present this rare case because of its clinical and radiological imitation of a ranula.
Keyword
Figure
Reference
-
References
1. El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ, editors. 2017. WHO classification of head and neck tumours. 4th ed. IARC (International Agency for Research on Cancer);Lyon:2. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. 2008. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. IARC;Lyon: p. 202–8.3. Choi G, Choi CS, Choi JS, Choi JO. 2001; Intraductal papilloma of the parotid gland in a child. Otolaryngol Head Neck Surg. 125:280. https://doi.org/10.1067/mhn.2001.115666. DOI: 10.1067/mhn.2001.115666. PMID: 11555769.
Article4. Brannon RB, Sciubba JJ, Giulani M. 2001; Ductal papillomas of salivary gland origin: a report of 19 cases and a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 92:68–77. https://doi.org/10.1067/moe.2001.115978. DOI: 10.1067/moe.2001.115978. PMID: 11458248.
Article5. Aikawa T, Kishino M, Masuda T, Isomura ET, Tanaka S, Namikawa M, et al. 2009; Intraductal papilloma arising from sublingual minor salivary gland: case report and immunohistochemical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 107:e34–7. Erratum in: Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:475. https://doi.org/10.1016/j.tripleo.2009.01.019. DOI: 10.1016/j.tripleo.2009.01.019. PMID: 19426904.
Article6. Nagao T, Sugano I, Matsuzaki O, Hara H, Kondo Y, Nagao K. 2000; Intraductal papillary tumors of the major salivary glands: case reports of benign and malignant variants. Arch Pathol Lab Med. 124:291–5. https://doi.org/10.5858/2000-124-0291-IPTOTM. DOI: 10.5858/2000-124-0291-IPTOTM. PMID: 10656742.
Article7. Hara H, Oyama T, Omori K, Misawa T, Kasai H, Kimura M, et al. 1999; Fine needle aspiration cytology of an intraductal papilloma originating in a sublingual gland. A case report. Acta Cytol. 43:457–63. https://doi.org/10.1159/000331100. DOI: 10.1159/000331100. PMID: 10349381.
Article8. Wenig BM. 2015. Atlas of head and neck pathology. 3rd ed. Elsevier;Philadelphia (PA): p. 908–14. p. 490–3.9. Infante-Cossio P, Gonzalo DH, Hernandez-Gutierrez J, Borrero-Martin JJ. 2008; Oral inverted ductal papilloma associated with condyloma acuminata and HPV in an HIV+ patient. Int J Oral Maxillofac Surg. 37:1159–61. https://doi.org/10.1016/j.ijom.2008.07.016. DOI: 10.1016/j.ijom.2008.07.016. PMID: 18774261.
Article10. Hellquist H, Paiva-Correia A, Vander Poorten V, Quer M, Hernandez-Prera JC, Andreasen S, et al. 2019; Analysis of the clinical relevance of histological classification of benign epithelial salivary gland tumours. Adv Ther. 36:1950–74. https://doi.org/10.1007/s12325-019-01007-3. DOI: 10.1007/s12325-019-01007-3. PMID: 31209701. PMCID: PMC6822986.
Article11. Ramaswamy P, Khaitan T, Anuradha A, Kumar BP, Sudhakar S. 2013; Intraductal papilloma: atypical presentation. Case Rep Dent. 2013:652728. https://doi.org/10.1155/2013/652728. DOI: 10.1155/2013/652728. PMID: 23762648. PMCID: PMC3677017.
Article12. Agaimy A, Mueller SK, Bumm K, Iro H, Moskalev EA, Hartmann A, et al. 2018; Intraductal papillary mucinous neoplasms of minor salivary glands with AKT1 p.Glu17Lys mutation. Am J Surg Pathol. 42:1076–82. https://doi.org/10.1097/PAS.0000000000001080. DOI: 10.1097/PAS.0000000000001080. PMID: 29738361.
Article13. Nakaguro M, Urano M, Ogawa I, Hirai H, Yamamoto Y, Yamaguchi H, et al. 2020; Histopathological evaluation of minor salivary gland papillary-cystic tumours: focus on genetic alterations in sialadenoma papilliferum and intraductal papillary mucinous neoplasm. Histopathology. 76:411–22. https://doi.org/10.1111/his.13990. DOI: 10.1111/his.13990. PMID: 31505033.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Case report of the management of the ranula
- Analysis of Treatment Result According to Operative Methods for Ranula
- Intraductal Papilloma Arising in the Sublingual Salivary Gland
- Transoral Drainage of Plunging Ranula using Intraoperative Ultrasonography after Sublingual Gland Resection: A Case Report
- A Case of Bilateral Plunging Ranula