J Korean Assoc Oral Maxillofac Surg.
2022 Feb;48(1):21-32. 10.5125/jkaoms.2022.48.1.21.
Effectiveness of dexamethasone or adrenaline with lignocaine 2% for prolonging inferior alveolar nerve block: a randomized controlled trial
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, MB Kedia Dental College, Birgunj, Nepal
- 2Department of Dentistry, National Medical College, MB Kedia Dental College, Birgunj, Nepal
- 3Department of Community Dentistry, MB Kedia Dental College, Birgunj, Nepal
- KMID: 2526807
- DOI: http://doi.org/10.5125/jkaoms.2022.48.1.21
Abstract
Objectives
Inferior alveolar nerve block (IANB) is commonly used for mandibular dentoalveolar surgery. The objective of this study was to evaluate and compare the effectiveness of coadministration of dexamethasone (4 mg/mL) or adrenaline (0.01 mg/mL) as an adjuvant with lignocaine 2% in IANB during third molar surgery (TMS).
Patients and Methods
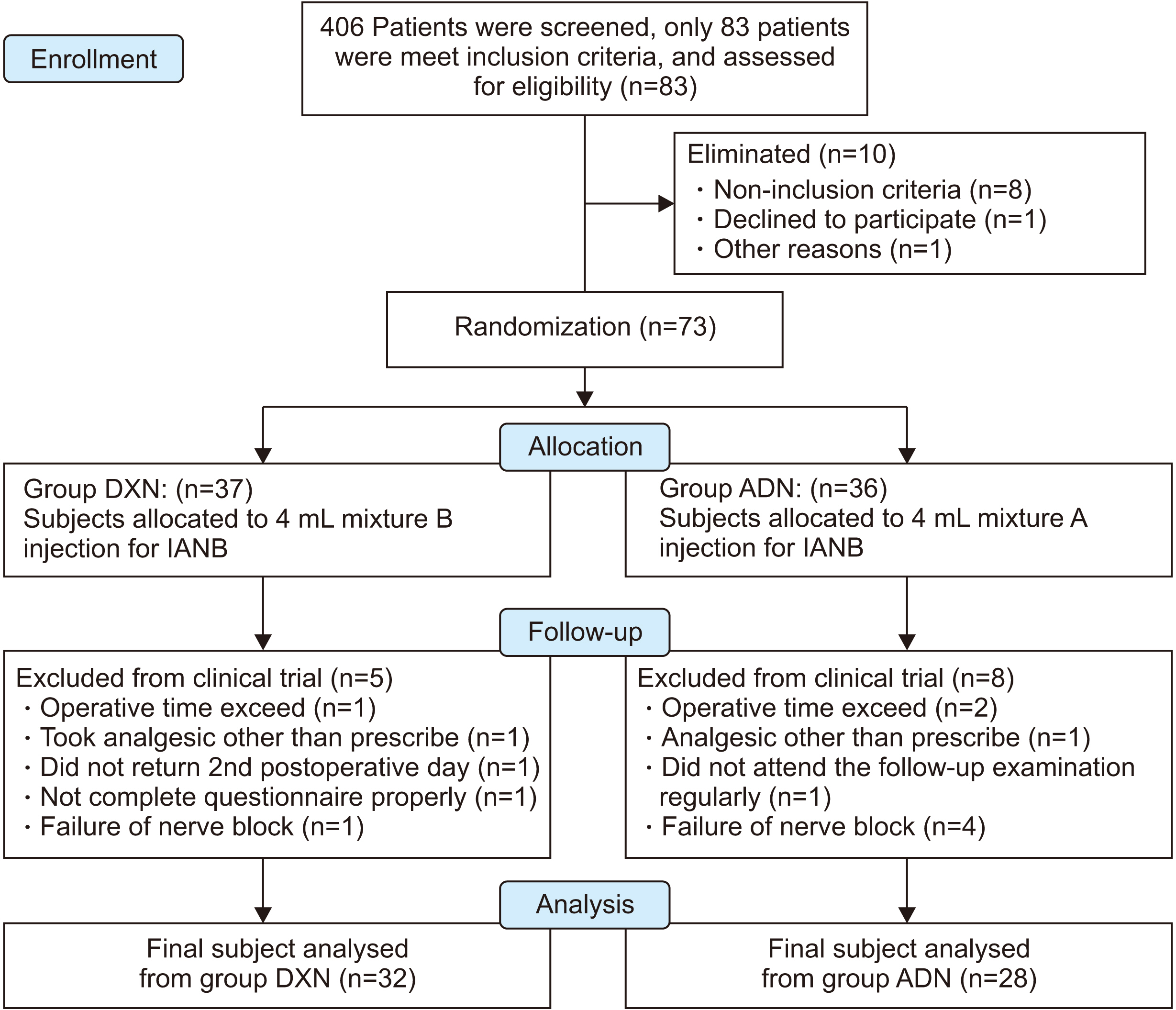
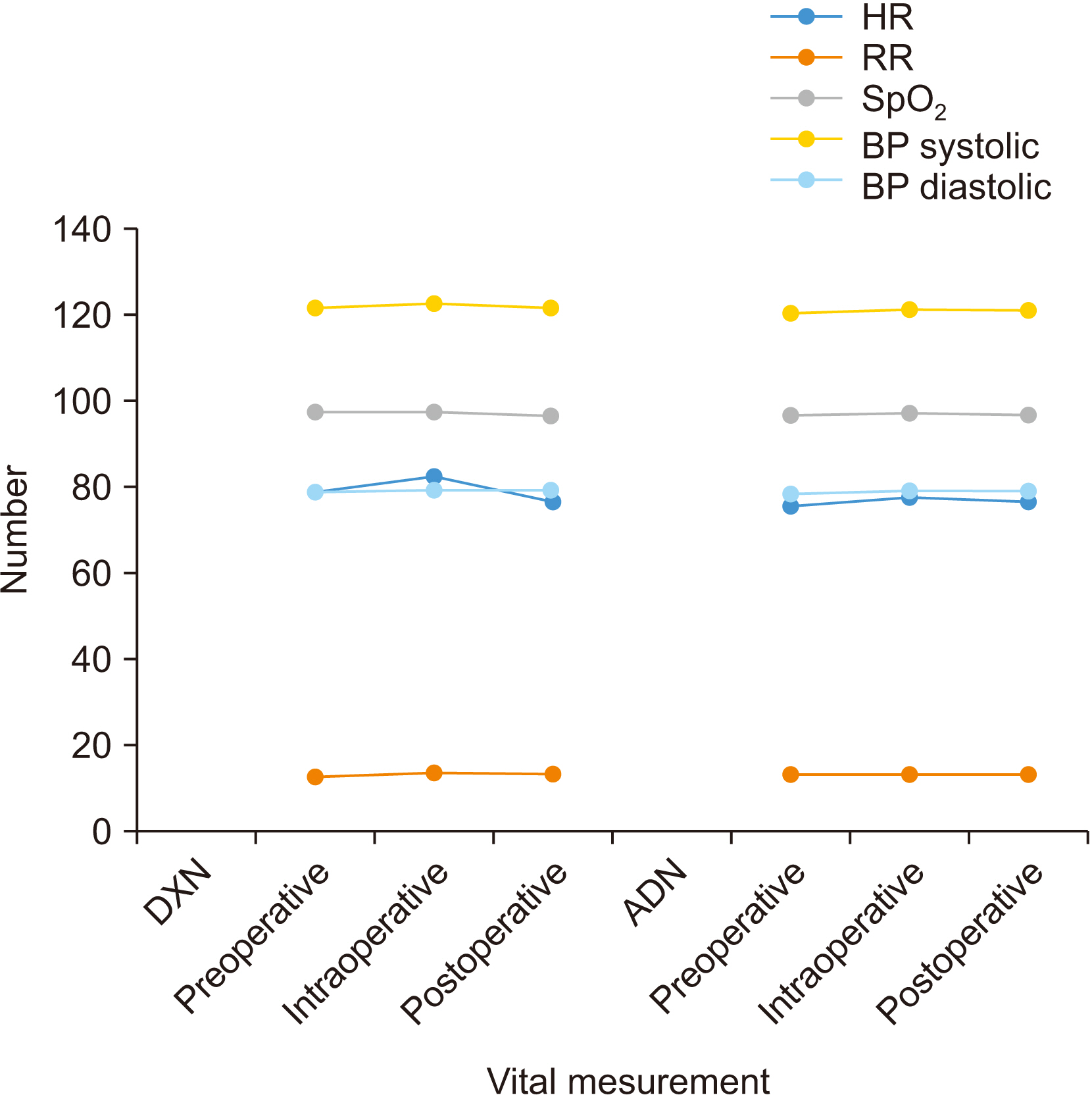
This double-blind, randomized controlled trial was conducted between March and August 2020. The investigators screened patients needing elective TMS under local anesthesia. Based on strict inclusion and exclusion criteria, patients were enrolled in this study. These patients were assigned randomly into two study groups: dexamethasone group (DXN) or adrenaline group (ADN). Outcome variables were postoperative edema, trismus, visual analogue scale (VAS), perioperative analgesia, onset time, and duration of IANB.
Results
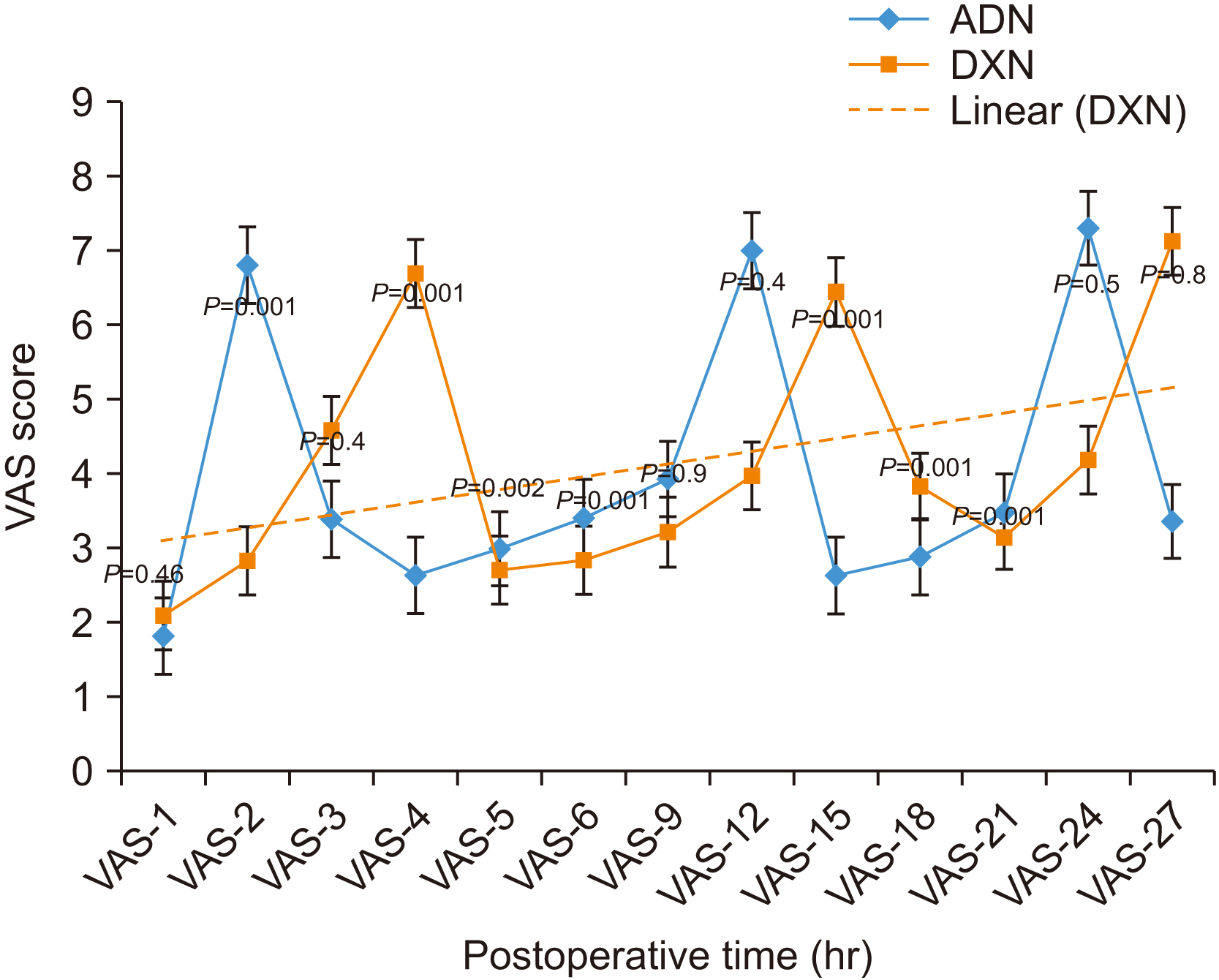
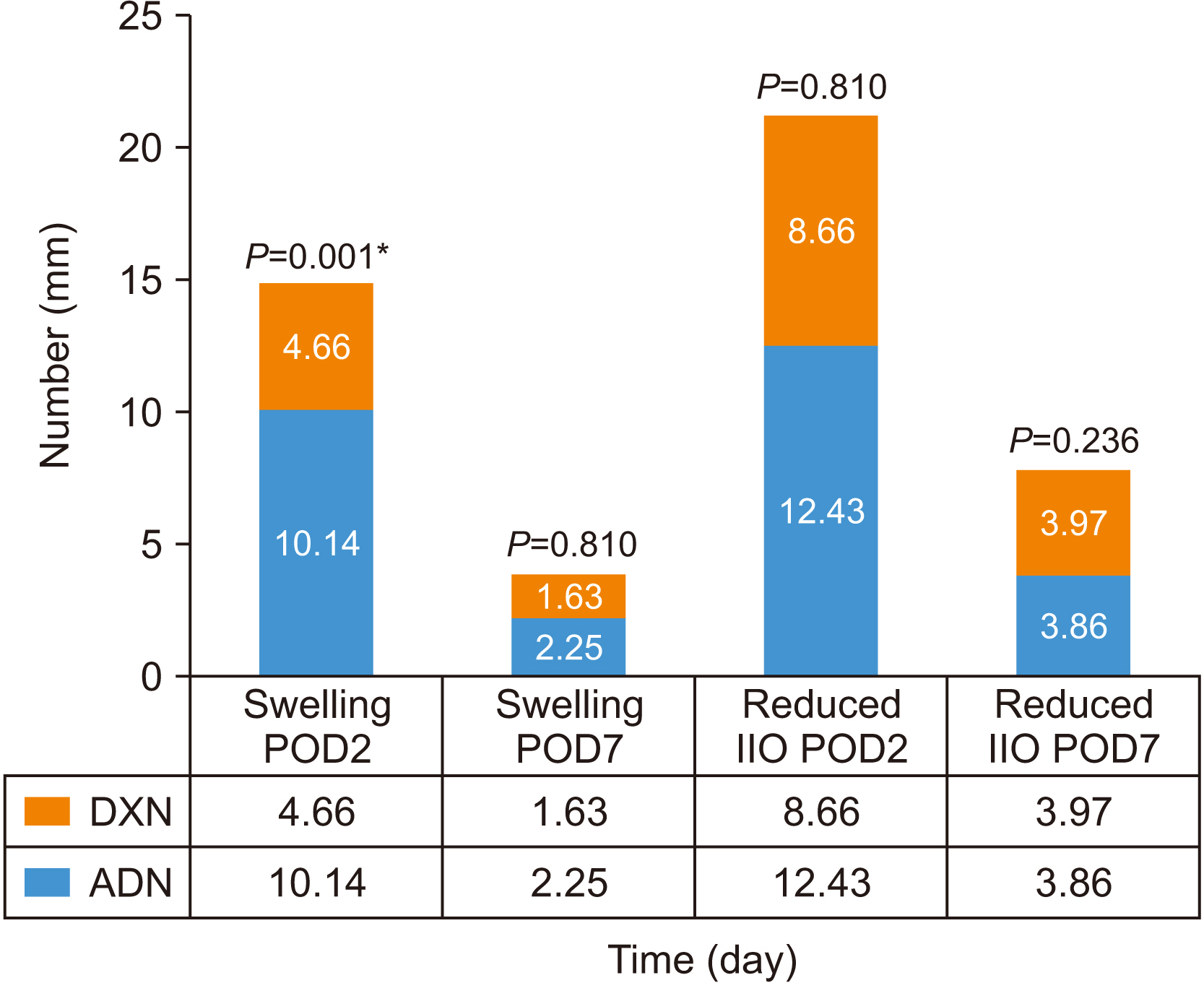
Eighty-three patients were enrolled in this study, of whom 23 (27.7%) were eliminated or excluded during follow-up. This study thus included data from 60 samples. Mean age was 32.28±11.74 years, including 28 females (46.7%) in the ADN (16 patients, 57.1%) and DXN (12 patients, 42.9%) groups. The duration of action for DXN (mean±standard deviation [SD], 4:02:07±0:34:01 hours; standard error [SE], 0:06:00 hours; log-rank P=0.001) and for ADN (mean±SD, 1:58:34±0:24:52 hours; SE, 0:04:42 hours; log-rank P=0.001) were found. Similarly, time at which 1st analgesic consume and total number of nonsteroidal antiinflammatory drugs need to rescue postoperative analgesia was found statistically significant between study groups (t (58)=–11.95; confidence interval, –2:25:41 to –1:43:53; P=0.001). Early-hours VAS was also significantly different between the study groups.
Conclusion
A single injection of dexamethasone prolongs the duration of action of lignocaine 2% IANB. Additionally, it can be used in cases where adrenaline is contraindicated.
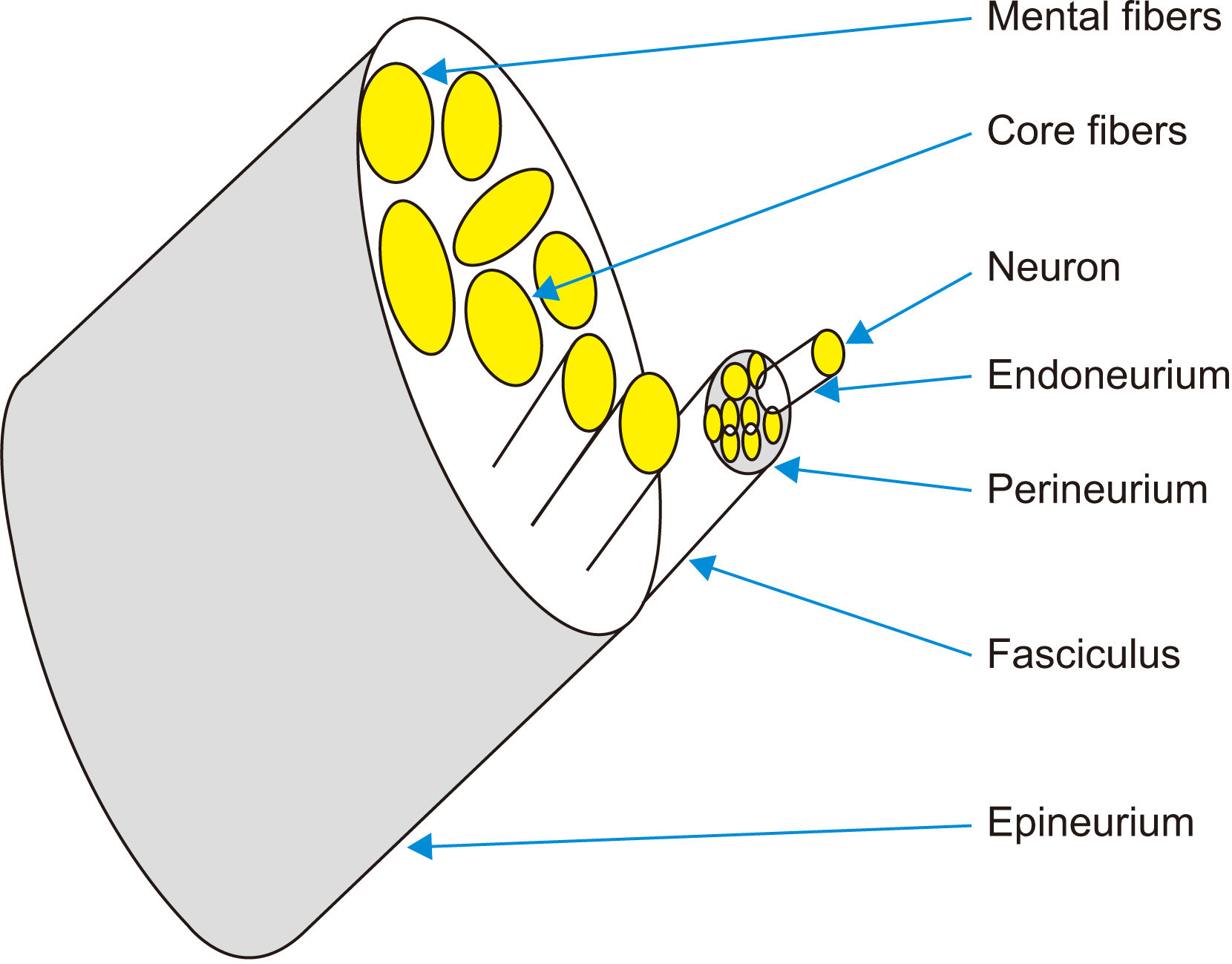
Figure
Reference
-
References
1. Calatayud J, González A. 2003; History of the development and evolution of local anesthesia since the coca leaf. Anesthesiology. 98:1503–8. https://doi.org/10.1097/00000542-200306000-00031. DOI: 10.1097/00000542-200306000-00031. PMID: 12766665.
Article2. Ogle OE, Mahjoubi G. 2011; Advances in local anesthesia in dentistry. Dent Clin North Am. 55:481–99. viii. https://doi.org/10.1016/j.cden.2011.02.007. DOI: 10.1016/j.cden.2011.02.007. PMID: 21726685.
Article3. Albaladejo P, Aubrun F, Samama CM, Jouffroy L, Beaussier M, Benhamou D, et al. 2017; The structure, organisation and perioperative management of ambulatory surgery and anaesthesia in France: methodology of the SFAR-OPERA study. Anaesth Crit Care Pain Med. 36:307–12. https://doi.org/10.1016/j.accpm.2016.10.002. DOI: 10.1016/j.accpm.2016.10.002. PMID: 27913269.
Article4. Yagiela JA. 2004; Recent developments in local anesthesia and oral sedation. Compend Contin Educ Dent. 25:697–706. quiz 708. PMID: 15645899.5. Chew ST, Tan T, Tan SS, Ip-Yam PC. 1998; A survey of patients' knowledge of anaesthesia and perioperative care. Singapore Med J. 39:399–402. PMID: 9885718.6. Buvanendran A, Fiala J, Patel KA, Golden AD, Moric M, Kroin JS. 2015; The incidence and severity of postoperative pain following inpatient surgery. Pain Med. 16:2277–83. https://doi.org/10.1111/pme.12751. DOI: 10.1111/pme.12751. PMID: 25917518.
Article7. Gan TJ, Habib AS, Miller TE, White W, Apfelbaum JL. 2014; Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Curr Med Res Opin. 30:149–60. https://doi.org/10.1185/03007995.2013.860019. DOI: 10.1185/03007995.2013.860019. PMID: 24237004.
Article8. Meissner W, Coluzzi F, Fletcher D, Huygen F, Morlion B, Neugebauer E, et al. 2015; Improving the management of post-operative acute pain: priorities for change. Curr Med Res Opin. 31:2131–43. https://doi.org/10.1185/03007995.2015.1092122. DOI: 10.1185/03007995.2015.1092122. PMID: 26359332.
Article9. Deo SP. 2011; Effect of submucosal injection of dexamethasone on post-operative sequelae of third molar surgery. JNMA J Nepal Med Assoc. 51:72–8. DOI: 10.31729/jnma.247. PMID: 22916516.10. Deo SP. 2016; Role of addition of dexamethasone to lignocaine 2% with adrenaline in dental nerve blocks for third molar surgery: a prospective randomized control trial. Ann Maxillofac Surg. 6:260–6. https://doi.org/10.4103/2231-0746.200341. DOI: 10.4103/2231-0746.200341. PMID: 28299268. PMCID: PMC5343638.
Article11. Latt MM, Kiattavorncharoen S, Boonsiriseth K, Pairuchvej V, Wongsirichat N. 2016; The efficacy of dexamethasone injection on postoperative pain in lower third molar surgery. J Dent Anesth Pain Med. 16:95–102. https://doi.org/10.17245/jdapm.2016.16.2.95. DOI: 10.17245/jdapm.2016.16.2.95. PMID: 28879301. PMCID: PMC5564088.
Article12. Barden J, Edwards JE, McQuay HJ, Andrew Moore R. 2004; Pain and analgesic response after third molar extraction and other postsurgical pain. Pain. 107:86–90. https://doi.org/10.1016/j.pain.2003.09.021. DOI: 10.1016/j.pain.2003.09.021. PMID: 14715393.
Article13. Marković AB, Todorović L. 2006; Postoperative analgesia after lower third molar surgery: contribution of the use of long-acting local anesthetics, low-power laser, and diclofenac. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 102:e4–8. https://doi.org/10.1016/j.tripleo.2006.02.024. DOI: 10.1016/j.tripleo.2006.02.024. PMID: 17052624.
Article14. Danielsson K, Evers H, Holmlund A, Kjellman O, Nordenram A, Persson NE. 1986; Long-acting local anaesthetics in oral surgery. Clinical evaluation of bupivacaine and etidocaine for mandibular nerve block. Int J Oral Maxillofac Surg. 15:119–26. https://doi.org/10.1016/s0300-9785(86)80131-4. DOI: 10.1016/S0300-9785(86)80131-4. PMID: 3083015.
Article15. Crincoli V, Favia G, LImongelli L, Tempesta A, Brienza N. 2015; The effectiveness of ropivacaine and mepivacaine in the postoperative pain after third lower molar surgery. Int J Med Sci. 12:862–6. https://doi.org/10.7150/ijms.13072. DOI: 10.7150/ijms.13072. PMID: 26640405. PMCID: PMC4643076.
Article16. Prabhakar A, Lambert T, Kaye RJ, Gaignard SM, Ragusa J, Wheat S, et al. 2019; Adjuvants in clinical regional anesthesia practice: a comprehensive review. Best Pract Res Clin Anaesthesiol. 33:415–23. https://doi.org/10.1016/j.bpa.2019.06.001. DOI: 10.1016/j.bpa.2019.06.001. PMID: 31791560.
Article17. Renck H, Hassan HG. 1992; Epinephrine as an adjuvant to amino-amide local anesthetics does not prolong their duration of action in infraorbital nerve block in the rat. Acta Anaesthesiol Scand. 36:387–92. https://doi.org/10.1111/j.1399-6576.1992.tb03486.x. DOI: 10.1111/j.1399-6576.1992.tb03486.x. PMID: 1632160.
Article18. Marhofer P, Columb M, Hopkins PM, Greher M, Marhofer D, Bienzle M, et al. 2019; Dexamethasone as an adjuvant for peripheral nerve blockade: a randomised, triple-blinded crossover study in volunteers. Br J Anaesth. 122:525–31. https://doi.org/10.1016/j.bja.2019.01.004. DOI: 10.1016/j.bja.2019.01.004. PMID: 30857609. PMCID: PMC6435911.
Article19. Swami SS, Keniya VM, Ladi SD, Rao R. 2012; Comparison of dexmedetomidine and clonidine (α2 agonist drugs) as an adjuvant to local anaesthesia in supraclavicular brachial plexus block: a randomised double-blind prospective study. Indian J Anaesth. 56:243–9. https://doi.org/10.4103/0019-5049.98767. DOI: 10.4103/0019-5049.98767. PMID: 22923822. PMCID: PMC3425283.
Article20. Zhang C, Li C, Pirrone M, Sun L, Mi W. 2016; Comparison of dexmedetomidine and clonidine as adjuvants to local anesthetics for intrathecal anesthesia: a meta-analysis of randomized controlled trials. J Clin Pharmacol. 56:827–34. https://doi.org/10.1002/jcph.666. DOI: 10.1002/jcph.666. PMID: 26510095.
Article21. McCartney CJ, Duggan E, Apatu E. 2007; Should we add clonidine to local anesthetic for peripheral nerve blockade? A qualitative systematic review of the literature. Reg Anesth Pain Med. 32:330–8. https://doi.org/10.1016/j.rapm.2007.02.010. DOI: 10.1016/j.rapm.2007.02.010. PMID: 17720118.
Article22. Bharti N, Sardana DK, Bala I. 2015; The analgesic efficacy of dexmedetomidine as an adjunct to local anesthetics in supraclavicular brachial plexus block: a randomized controlled trial. Anesth Analg. 121:1655–60. https://doi.org/10.1213/ANE.0000000000001006. DOI: 10.1213/ANE.0000000000001006. PMID: 26496366.
Article23. Candido KD, Winnie AP, Ghaleb AH, Fattouh MW, Franco CD. 2002; Buprenorphine added to the local anesthetic for axillary brachial plexus block prolongs postoperative analgesia. Reg Anesth Pain Med. 27:162–7. https://doi.org/10.1053/rapm.2002.30671. DOI: 10.1053/rapm.2002.30671. PMID: 11915063.
Article24. Shah A, Halli R, Merchant Y, Kshirsagar R, Khurana J. 2016; Efficacy of ketamine as an adjunct to local anesthesia in the surgical removal of impacted mandibular third molars - a split mouth prospective controlled clinical study. J Clin Diagn Res. 10:ZC29–33. https://doi.org/10.7860/JCDR/2016/19677.8638. DOI: 10.7860/JCDR/2016/19677.8638. PMID: 27891453. PMCID: PMC5121799.
Article25. Ettinger KS, Jacob AK, Viozzi CF, Van Ess JM, Fillmore WJ, Arce K. 2015; Does intravenous midazolam dose influence the duration of recovery room stay following outpatient third molar surgery? J Oral Maxillofac Surg. 73:2287–93. https://doi.org/10.1016/j.joms.2015.06.164. DOI: 10.1016/j.joms.2015.06.164. PMID: 26183011.
Article26. Tempestini Horliana AC, de Brito MA, Perez FE, Simonetti MP, Rocha RG, Borsatti MA. 2008; Hyaluronidase increases the duration of mepivacaine in inferior alveolar nerve blocks. J Oral Maxillofac Surg. 66:286–90. https://doi.org/10.1016/j.joms.2007.06.628. DOI: 10.1016/j.joms.2007.06.628. PMID: 18201610.
Article27. Yadav RK, Sah BP, Kumar P, Singh SN. 2008; Effectiveness of addition of neostigmine or dexamethasone to local anaesthetic in providing perioperative analgesia for brachial plexus block: a prospective, randomized, double blinded, controlled study. Kathmandu Univ Med J (KUMJ). 6:302–9. https://doi.org/10.3126/kumj.v6i3.1704. DOI: 10.3126/kumj.v6i3.1704. PMID: 20071811.
Article28. Shah DM, Arora M, Trikha A, Prasad G, Sunder R, Kotwal P, et al. 2015; Comparison of dexamethasone and clonidine as an adjuvant to 1.5% lignocaine with adrenaline in infraclavicular brachial plexus block for upper limb surgeries. J Anaesthesiol Clin Pharmacol. 31:354–9. https://doi.org/10.4103/0970-9185.161672. DOI: 10.4103/0970-9185.161672. PMID: 26330715. PMCID: PMC4541183.
Article29. Biradar PA, Kaimar P, Gopalakrishna K. 2013; Effect of dexamethasone added to lidocaine in supraclavicular brachial plexus block: a prospective, randomised, double-blind study. Indian J Anaesth. 57:180–4. https://doi.org/10.4103/0019-5049.111850. DOI: 10.4103/0019-5049.111850. PMID: 23825819. PMCID: PMC3696267.
Article30. Alzeftawy AE, El Morad MB. 2018; Dexamethasone compared to dexmedetomidine as an adjuvant to local anesthetic mixture in peribulbar block for vitreoretinal surgery. A prospective randomized study. Anesth Essays Res. 12:359–65. https://doi.org/10.4103/aer.AER_224_17. DOI: 10.4103/aer.AER_224_17. PMID: 29962598. PMCID: PMC6020602.
Article31. Vadhanan P, Ganesh N, Ahmed MIH. 2018; Comparison of dexamethasone and buprenorphine as adjuvant in ultrasound-guided brachial plexus blocks: a randomized controlled trial. Anesth Essays Res. 12:176–9. https://doi.org/10.4103/aer.AER_129_17. DOI: 10.4103/aer.AER_129_17. PMID: 29628577. PMCID: PMC5872859.
Article32. Kheirabadi D, Shafa A, Hirmanpour A, Zareh F. 2020; Prophylactic effects of intravenous dexamethasone and lidocaine on attenuating hemodynamic-respiratory and pain complications in children undergoing cleft palate repair surgery with general anesthesia. J Pain Palliat Care Pharmacother. 34:63–8. https://doi.org/10.1080/15360288.2019.1706691. DOI: 10.1080/15360288.2019.1706691. PMID: 31922432.
Article33. McHardy PG, Singer O, Awad IT, Safa B, Henry PDG, Kiss A, et al. 2020; Comparison of the effects of perineural or intravenous dexamethasone on low volume interscalene brachial plexus block: a randomised equivalence trial. Br J Anaesth. 124:84–91. https://doi.org/10.1016/j.bja.2019.08.025. DOI: 10.1016/j.bja.2019.08.025. PMID: 31591018.
Article34. Choi S, Rodseth R, McCartney CJ. 2014; Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: a systematic review and meta-analysis of randomized trials. Br J Anaesth. 112:427–39. https://doi.org/10.1093/bja/aet417. DOI: 10.1093/bja/aet417. PMID: 24413428.
Article35. Bhargava D, Sreekumar K, Rastogi S, Deshpande A, Chakravorty N. 2013; A prospective randomized double-blind study to assess the latency and efficacy of twin-mix and 2% lignocaine with 1:200,000 epinephrine in surgical removal of impacted mandibular third molars: a pilot study. Oral Maxillofac Surg. 17:275–80. https://doi.org/10.1007/s10006-012-0372-3. DOI: 10.1007/s10006-012-0372-3. PMID: 23143710.
Article36. Calvo AM, Santos GM, Dionísio TJ, Marques MP, Brozoski DT, Lanchote VL, et al. 2016; Quantification of piroxicam and 5'-hydroxypiroxicam in human plasma and saliva using liquid chromatography-tandem mass spectrometry following oral administration. J Pharm Biomed Anal. 120:212–20. https://doi.org/10.1016/j.jpba.2015.12.042. DOI: 10.1016/j.jpba.2015.12.042. PMID: 26760238.
Article37. Hargreaves KM, Schmidt EA, Mueller GP, Dionne RA. 1987; Dexamethasone alters plasma levels of beta-endorphin and postoperative pain. Clin Pharmacol Ther. 42:601–7. https://doi.org/10.1038/clpt.1987.206. DOI: 10.1038/clpt.1987.206. PMID: 2961501.
Article38. Hosgor H, Coskunses FM, Tokuc B. 2021; Correlation between preoperative pressure pain assessments and anxiety and postoperative pain in impacted lower third molar surgery. J Korean Assoc Oral Maxillofac Surg. 47:15–9. https://doi.org/10.5125/jkaoms.2021.47.1.15. DOI: 10.5125/jkaoms.2021.47.1.15. PMID: 33632972. PMCID: PMC7925165.
Article39. Benzon HT, Chew TL, McCarthy RJ, Benzon HA, Walega DR. 2007; Comparison of the particle sizes of different steroids and the effect of dilution: a review of the relative neurotoxicities of the steroids. Anesthesiology. 106:331–8. https://doi.org/10.1097/00000542-200702000-00022. DOI: 10.1097/00000542-200702000-00022. PMID: 17264728.
Article40. Alexander RE, Throndson RR. 2000; A review of perioperative corticosteroid use in dentoalveolar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 90:406–15. https://doi.org/10.1067/moe.2000.109778. DOI: 10.1067/moe.2000.109778. PMID: 11027375.
Article41. Markiewicz MR, Brady MF, Ding EL, Dodson TB. 2008; Corticosteroids reduce postoperative morbidity after third molar surgery: a systematic review and meta-analysis. J Oral Maxillofac Surg. 66:1881–94. https://doi.org/10.1016/j.joms.2008.04.022. DOI: 10.1016/j.joms.2008.04.022. PMID: 18718396.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical efficacy of 0.75% ropivacaine vs. 2% lignocaine hydrochloride with adrenaline (1:80,000) in patients undergoing removal of bilateral maxillary third molars: a randomized controlled trial
- Efficacy of buccal piroxicam infiltration and inferior alveolar nerve block in patients with irreversible pulpitis: a prospective, double-blind, randomized clinical trial
- Post-operative analgesia of 2% lignocaine with or without magnesium sulfate for inferior alveolar nerve block in symptomatic mandibular molars - a randomized double blind controlled clinical trial
- Pain perception and efficacy of local analgesia using 2% lignocaine, buffered lignocaine, and 4% articaine in pediatric dental procedures
- Photobiomodulation by soft laser irradiation with and without ibuprofen improves success rate of inferior alveolar nerve block using 2% lignocaine with adrenaline in symptomatic irreversible pulpitis of mandibular molar teeth: a double-blind, randomized placebo-controlled trial