Neurointervention.
2022 Mar;17(1):58-64. 10.5469/neuroint.2021.00444.
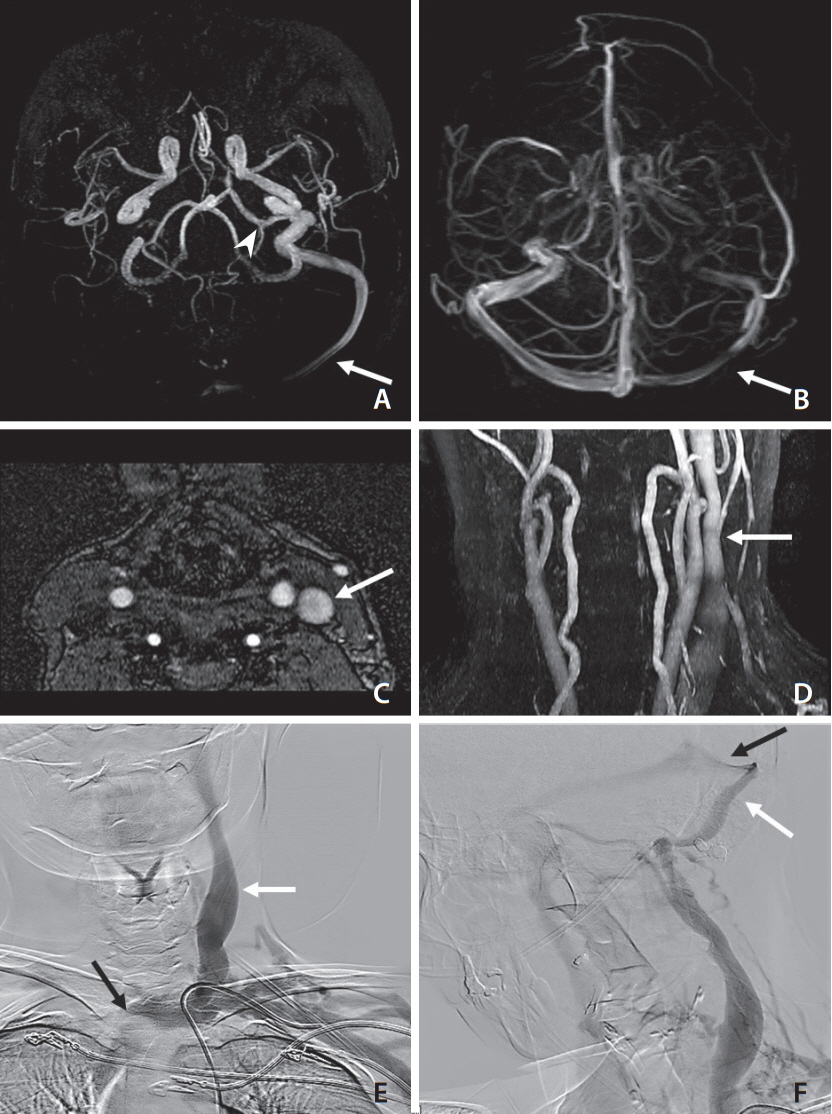
Central Venous Reflux, a Rare Cause of Neurological Manifestations in Hemodialysis Patients: A Case Report and Literature Review
- Affiliations
-
- 1Department of Neurology, Hospital Británico, Buenos Aires, Argentina
- 2Department of Neuroradiology, Hospital Británico, Buenos Aires, Argentina
- 3Department of Interventional Neuroradiology, Hospital Británico, Buenos Aires, Argentina
- 4Department of Nephrology, Hospital Británico, Buenos Aires, Argentina
- KMID: 2526628
- DOI: http://doi.org/10.5469/neuroint.2021.00444
Abstract
- Central venous disease (CVD) is a serious complication in hemodialysis patients. Neurological manifestations are rare. We describe a female with end-stage renal disease with throbbing headache accompanied by paresthesia, weakness, and abnormal posture of her right hand during dialysis sessions. Motor symptoms completely resolved after each dialysis session, although the headaches persisted for several hours. No neurological deficit was evidenced on physical examination. Digital subtraction angiography identified an incomplete thrombosis of the left brachiocephalic vein with retrograde flow in the internal jugular vein, sigmoid sinus, and transverse sinus on the left side. This case illustrates that cerebral venous congestion due to CVD can produce neurological symptoms. Furthermore, we systematically review the literature to identify the characteristics of the cases described so far. This allows clinicians to know the entity and have a high index of suspicion in a hemodialysis patient who develops neurological symptoms.
Keyword
Figure
Reference
-
1. Haruma J, Escalard S, Smajda S, Piotin M. Left temporal hemorrhage caused by cerebral venous reflux of a brachio-brachial hemodialysis fistula. Neuroradiology. 2020; 62:1341–1344.
Article2. Prasad V, Baghai S, Gandhi D, Moeslein F, Jindal G. Cerebral infarction due to central vein occlusion in a hemodialysis patient. J Neuroimaging. 2015; 25:494–496.
Article3. Herzig DW, Stemer AB, Bell RS, Liu AH, Armonda RA, Bank WO. Neurological sequelae from brachiocephalic vein stenosis. J Neurosurg. 2013; 118:1058–1062.
Article4. Salama GR, Farinhas JM, Pasquale DD, Wertenbaker C, Bello JA. Central venous occlusion mimics carotid cavernous fistula: a case report and review of the literature. Clin Imaging. 2014; 38:884–887.
Article5. Cleper R, Goldenberg-Cohen N, Kornreich L, Krause I, Davidovits M. Neurologic and ophthalmologic complications of vascular access in a hemodialysis patient. Pediatr Nephrol. 2007; 22:1377–1382.
Article6. Samaniego EA, Abrams KJ, Dabus G, Starr R, Linfante I. Severe venous congestive encephalopathy secondary to a dialysis arteriovenous graft. J Neurointerv Surg. 2013; 5:e37.
Article7. Nishimoto H, Ogasawara K, Miura K, Ohmama S, Kashimura H, Ogawa A. Acute intracranial hypertension due to occlusion of the brachiocephalic vein in a patient undergoing hemodialysis. Cerebrovasc Dis. 2005; 20:207–208.
Article8. Kim CH, Kang J, Choi DS, Park JH. Intracranial venous reflux caused by occlusion of the brachiocephalic vein mimicking dural arteriovenous fistula. World Neurosurg. 2018; 120:438–441.
Article9. Mackay DD, Biousse V. Hemodialysis graft-induced intracranial hypertension. Neurol Clin Pract. 2015; 5:494–497.
Article10. Lal SM, Twardowski ZJ, Van Stone J, Keniston D, Scott WJ, Berg GG, et al. Benign intracranial hypertension: a complication of subclavian vein catheterization and arteriovenous fistula. Am J Kidney Dis. 1986; 8:262–264.
Article11. Molina JC, Martinez-Vea A, Riu S, Callizo J, Barbod A, Garcia C, et al. Pseudotumor cerebri: an unusual complication of brachiocephalic vein thrombosis associated with hemodialysis catheters. Am J Kidney Dis. 1998; 31:E3.
Article12. Varelas PN, Bertorini TE, Halford H. Bilateral ophthalmoplegia and exophthalmos complicating central hemodialysis catheter placement. Am J Kidney Dis. 1999; 33:966–969.
Article13. Hartmann A, Mast H, Stapf C, Koch HC, Marx P. Peripheral hemodialysis shunt with intracranial venous congestion. Stroke. 2001; 32:2945–2946.
Article14. Chang S, Masaryk TJ, Lee MS. Optic nerve edema: complication of peripheral hemodialysis shunt. Semin Ophthalmol. 2004; 19:88–90.
Article15. Cuadra SA, Padberg FT, Turbin RE, Farkas J, Frohman LP. Cerebral venous hypertension and blindness: a reversible complication. J Vasc Surg. 2005; 42:792–795.
Article16. Watson RR, Russo C. Upper extremity arteriovenous dialysis fistula resulting in cavernous sinus arterialized blood flow. AJNR Am J Neuroradiol. 2007; 28:1155–1156.
Article17. Nishijima H, Tomiyama M, Haga R, Ueno T, Miki Y, Arai A, et al. Venous cerebral infarction in a patient with peripheral hemodialysis shunt and occlusion of the left brachiocephalic vein. J Stroke Cerebrovasc Dis. 2011; 20:381–383.
Article18. Saha MK, Hamieh T, Larkin B, Mcmillan W. Cerebral hemorrhage due to internal jugular vein stenosis in a hemodialysis patient. Clin Exp Nephrol. 2012; 16:345–349.
Article19. Simon MA, Duffis EJ, Curi MA, Turbin RE, Prestigiacomo CJ, Frohman LP. Papilledema due to a permanent catheter for renal dialysis and an arteriovenous fistula: a “two hit” hypothesis. J Neuroophthalmol. 2014; 34:29–33.
Article20. Iguchi T, Harada M, Kurihara S, Ichikawa T, Satoh S, Kobayashi M. Neurological symptoms due to intracranial venous congestion in a hemodialysis patient with arteriovenous shunted flow. Kidney Int Rep. 2020; 5:2097–2101.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Resolved Cerebral Venous Hypertension after Angioplasty of Central Venous Stenosis in a Hemodialysis Patient: A Case Report
- A Case of Pseudoaneurysm of the Common Carotid Artery Associated with Central Venous Catheterization in a Patient on Hemodialysis
- A Rare Case of Massive Hemothorax due to Central Venous Catheterization Treated with Angiographic Stent Implantation
- Cerebral Venous Infarction Due to Brachial Artery-Jugular Vein Jump Graft in a Hemodialysis Patient
- Cerebral Air Embolism after Central Venous Catheter Removal in a Patient with a Patent Foramen Ovale: A Case Report and Literature Review