J Korean Med Sci.
2022 Feb;37(6):e46. 10.3346/jkms.2022.37.e46.
Mother-Adolescent Discrepancies in Reporting Sleep Disturbances: Effects of Diagnosis and Mother’s Occupation
- Affiliations
-
- 1Department of Psychiatry, Konkuk University Medical Center, Seoul, Korea
- 2Department of Psychiatry, Soonchunhyang University Seoul Hospital, College of Medicine, Soonchunhyang University, Seoul, Korea
- 3Department of Psychiatry, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea
- KMID: 2526034
- DOI: http://doi.org/10.3346/jkms.2022.37.e46
Abstract
- Background
Sleep disturbances are common in children and adolescents. However, they are rarely diagnosed and treated because parents, who often report the symptoms, may fail to notice the problems. Factors that can affect parent-child discrepancy include child’s diagnosis, parent’s occupation, and child’s sex. The current study retrospectively analyzed the effect of these factors on parent-child discrepancies of sleep disturbance scores.
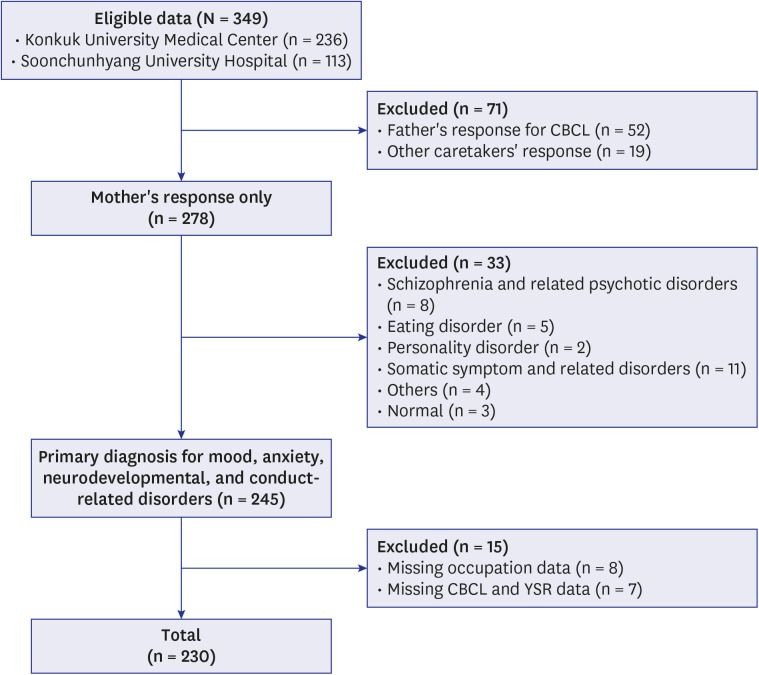
Methods
Data for sleep-related items in Youth Self-Report (YSR) and Child Behavior Checklist (CBCL) from 2014 to 2020 August in South Korea were collected from psychiatric outpatient clinics at Konkuk University Medical Center and Soonchunhyang University Hospital.
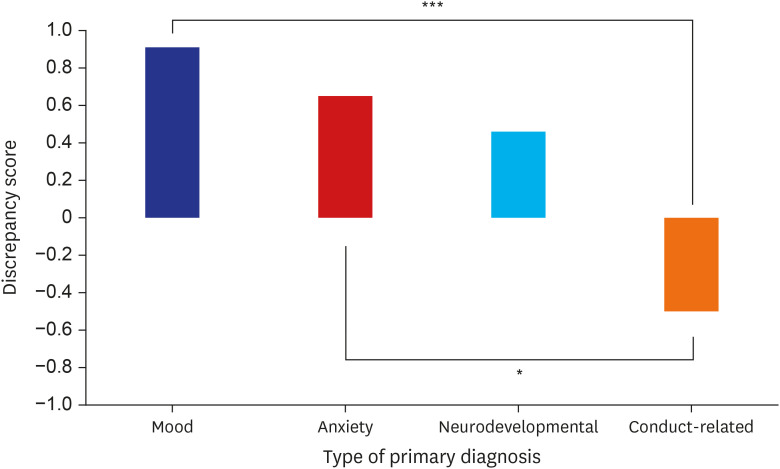
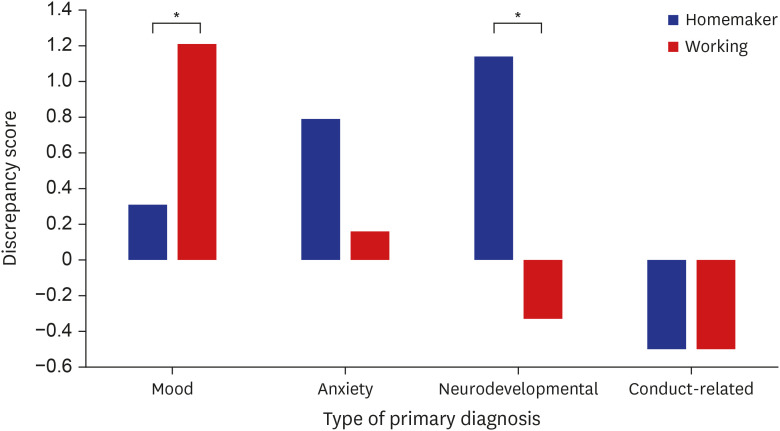
Results
A three-way analysis of variance revealed main effect of diagnosis type and interaction between diagnosis type and mother’s occupation. Discrepancies were greater for mood and anxiety disorders compared to conduct-related disorder. Interaction effect revealed greater discrepancies in mood disorders for reports completed by working mothers compared to homemaker mothers.
Conclusion
The results of this study emphasize the need to explore with caution the selfreported sleep disturbances in adolescents, especially in those with mood disorders. The results also suggest that mother’s occupation should be taken into account when evaluating sleep reports of parents and adolescents.
Keyword
Figure
Reference
-
1. Blader JC, Koplewicz HS, Abikoff H, Foley C. Sleep problems of elementary school children. A community survey. Arch Pediatr Adolesc Med. 1997; 151(5):473–480. PMID: 9158439.2. Fricke-Oerkermann L, Plück J, Schredl M, Heinz K, Mitschke A, Wiater A, et al. Prevalence and course of sleep problems in childhood. Sleep. 2007; 30(10):1371–1377. PMID: 17969471.3. Beebe DW. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin North Am. 2011; 58(3):649–665. PMID: 21600347.4. Yoo MA, Kang NG, Lee HJ. Relationships between sleep habits, daytime sleepiness and problem behaviors among adolescents. J Digit Converg. 2017; 15(5):305–315.5. Kim SJ. A study of the association between sleep habits and cognitive, emotional, behavioral outcomes in preschool children. J Korean Counc Child Rights. 2015; 19(3):319–341.6. Armstrong JM, Ruttle PL, Klein MH, Essex MJ, Benca RM. Associations of child insomnia, sleep movement, and their persistence with mental health symptoms in childhood and adolescence. Sleep (Basel). 2014; 37(5):901–909.7. Fallone G, Owens JA, Deane J. Sleepiness in children and adolescents: clinical implications. Sleep Med Rev. 2002; 6(4):287–306. PMID: 12531133.8. Sadeh A, Gruber R, Raviv A. Sleep, neurobehavioral functioning, and behavior problems in school-age children. Child Dev. 2002; 73(2):405–417. PMID: 11949899.9. Chervin RD, Archbold KH, Panahi P, Pituch KJ. Sleep problems seldom addressed at two general pediatric clinics. Pediatrics. 2001; 107(6):1375–1380. PMID: 11389260.10. Thome M, Skuladottir A. Changes in sleep problems, parents distress and impact of sleep problems from infancy to preschool age for referred and unreferred children. Scand J Caring Sci. 2005; 19(2):86–94. PMID: 15877633.11. De Los Reyes A, Augenstein TM, Wang M, Thomas SA, Drabick DA, Burgers DE, et al. The validity of the multi-informant approach to assessing child and adolescent mental health. Psychol Bull. 2015; 141(4):858–900. PMID: 25915035.12. Van Roy B, Groholt B, Heyerdahl S, Clench-Aas J. Understanding discrepancies in parent-child reporting of emotional and behavioural problems: effects of relational and socio-demographic factors. BMC Psychiatry. 2010; 10(1):56. PMID: 20637090.13. Kim J, Chan YF, McCauley E, Stoep AV. Parent-child discrepancies in reporting of child depression in ethnic groups. J Nurse Pract. 2016; 12(6):374–380. PMID: 27672356.14. Behrens B, Swetlitz C, Pine DS, Pagliaccio D. The Screen for Child Anxiety Related Emotional Disorders (SCARED): informant discrepancy, measurement invariance, and test-retest reliability. Child Psychiatry Hum Dev. 2019; 50(3):473–482. PMID: 30460424.15. Makol BA, Polo AJ. Parent-child endorsement discrepancies among youth at chronic-risk for depression. J Abnorm Child Psychol. 2018; 46(5):1077–1088. PMID: 29124497.16. Klaus NM, Mobilio A, King CA. Parent-adolescent agreement concerning adolescents’ suicidal thoughts and behaviors. J Clin Child Adolesc Psychol. 2009; 38(2):245–255. PMID: 19283602.17. Treutler CM, Epkins CC. Are discrepancies among child, mother, and father reports on children’s behavior related to parents’ psychological symptoms and aspects of parent-child relationships? J Abnorm Child Psychol. 2003; 31(1):13–27. PMID: 12597696.18. Combs D, Goodwin JL, Quan SF, Morgan WJ, Hsu CH, Edgin JO, et al. Mother knows best? Comparing child report and parent report of sleep parameters with polysomnography. J Clin Sleep Med. 2019; 15(1):111–117. PMID: 30621839.19. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Arlington, VA, USA: American Psychiatric Association;2013.20. Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT, USA: University of Vermont, Research Center for Children, Youth & Families;2001.21. Oh KJ, Kim YA, Ha EH, Lee HI, Hong KE. Child Behavior Checklist 6-18: CBCL 6-18. Seoul, Korea: HUNO;2010.22. Thompson EC, Fox KA, Lapomardo A, Hunt JI, Wolff JC. Youth self report thought problems and sleep difficulties are linked to suicidal ideation among psychiatrically hospitalized adolescents. J Child Adolesc Psychopharmacol. 2020; 30(8):522–525. PMID: 32053009.23. Kozak M, Piepho HP. What’s normal anyway? Residual plots are more telling than significance tests when checking ANOVA assumptions. J Agron Crop Sci. 2018; 204(1):86–98.24. Kovacs M, Devlin B. Internalizing disorders in childhood. J Child Psychol Psychiatry. 1998; 39(1):47–63. PMID: 9534086.25. Gomez R, Vance A, Gomez RM. Analysis of the convergent and discriminant validity of the CBCL, TRF, and YSR in a clinic-referred sample. J Abnorm Child Psychol. 2014; 42(8):1413–1425. PMID: 24824190.26. Bajeux E, Klemanski DH, Husky M, Leray E, Chan Chee C, Shojaei T, et al. Factors associated with parent-child discrepancies in reports of mental health disorders in young children. Child Psychiatry Hum Dev. 2018; 49(6):1003–1010. PMID: 29869765.27. Aronen ET, Lampenius T, Fontell T, Simola P. Sleep in children with disruptive behavioral disorders. Behav Sleep Med. 2014; 12(5):373–388. PMID: 24180372.28. Chervin RD, Dillon JE, Archbold KH, Ruzicka DL. Conduct problems and symptoms of sleep disorders in children. J Am Acad Child Adolesc Psychiatry. 2003; 42(2):201–208. PMID: 12544180.29. Kamphuis J, Meerlo P, Koolhaas JM, Lancel M. Poor sleep as a potential causal factor in aggression and violence. Sleep Med. 2012; 13(4):327–334. PMID: 22305407.30. Bates JE, Viken RJ, Alexander DB, Beyers J, Stockton L. Sleep and adjustment in preschool children: sleep diary reports by mothers relate to behavior reports by teachers. Child Dev. 2002; 73(1):62–74. PMID: 14717244.31. Chorney DB, Detweiler MF, Morris TL, Kuhn BR. The interplay of sleep disturbance, anxiety, and depression in children. J Pediatr Psychol. 2008; 33(4):339–348. PMID: 17991689.32. Stores G. Multifactorial influences, including comorbidities, contributing to sleep disturbance in children with a neurodevelopmental disorder. CNS Neurosci Ther. 2016; 22(11):875–879. PMID: 27283112.33. Yang CK, Hahn HM. Cosleeping in young Korean children. J Dev Behav Pediatr. 2002; 23(3):151–157. PMID: 12055497.34. McStay RL, Dissanayake C, Scheeren A, Koot HM, Begeer S. Parenting stress and autism: the role of age, autism severity, quality of life and problem behaviour of children and adolescents with autism. Autism. 2014; 18(5):502–510. PMID: 24104515.35. Lee JK, Chiang HM. Parenting stress in South Korean mothers of adolescent children with autism spectrum disorder. Int J Dev Disabil. 2017; 64(2):120–127. PMID: 34141299.36. Almogbel YS, Goyal R, Sansgiry SS. Association between parenting stress and functional impairment among children diagnosed with neurodevelopmental disorders. Community Ment Health J. 2017; 53(4):405–414. PMID: 28176211.37. Kroes G, Veerman JW, De Bruyn EE. Bias in parental reports? Maternal psychopathology and the reporting of problem behavior in clinic-referred children. Eur J Psychol Assess. 2003; 19(3):195–203.38. Chandler S, Howlin P, Simonoff E, Kennedy J, Baird G. Comparison of parental estimate of developmental age with measured IQ in children with neurodevelopmental disorders. Child Care Health Dev. 2016; 42(4):486–493. PMID: 27126521.39. Lerner MD, Calhoun CD, Mikami AY, De Los Reyes A. Understanding parent-child social informant discrepancy in youth with high functioning autism spectrum disorders. J Autism Dev Disord. 2012; 42(12):2680–2692. PMID: 22456819.40. Willinger M, Ko CW, Hoffman HJ, Kessler RC, Corwin MJ. National Infant Sleep Position study. Trends in infant bed sharing in the United States, 1993-2000: the National Infant Sleep Position study. Arch Pediatr Adolesc Med. 2003; 157(1):43–49. PMID: 12517193.41. Koh SK. Factors affecting children’s sleep duration and sleep time poverty. J Fam Resour Manage Policy Rev. 2017; 21(3):141–159.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Study of Mother's Nursing Need and Perceived Her Role During Puerperium Period
- A Study on the Correlation between Stress, Mother-adolescent Communication and Quality of Life in the Adolescents
- Effects of a Mother-fetus Interaction Promotion Program on Sleep and Activity in Mothers and Infants
- Effects of Hearing Recorded Mother's Voice on Physiological Reactions and Behavioral State of Sleep, Weight of Very Low Birth Weight Infants
- Model Structure for Mother-Child Relationship for Korean Infants and Toddlers and Their Mothers