J Dent Rehabil Appl Sci.
2021 Dec;37(4):225-231. 10.14368/jdras.2021.37.4.225.
Analysis of splint weaning in temporomandibular disorder patients
- Affiliations
-
- 1Department of Orofacial Pain and Oral Medicine, Yonsei University College of Dentistry, Seoul, Republic of Korea
- 2Department of Biology, Lake Forest College, Illinois, USA
- 3TMJ & Orofacial Pain Center, Los Angeles, USA
- KMID: 2525997
- DOI: http://doi.org/10.14368/jdras.2021.37.4.225
Abstract
- Purpose
There are many studies on the indications and efficacy of splint therapy commonly used in patients with temporomandibular disorders (TMD). However, there have been no studies on the splint weaning in terms of the splint use tapering period in relation to symptom improvement of TMD. This retrospective study aims to analyze a proper splint weaning method in patients with TMD based on symptom improvement.
Materials and Methods
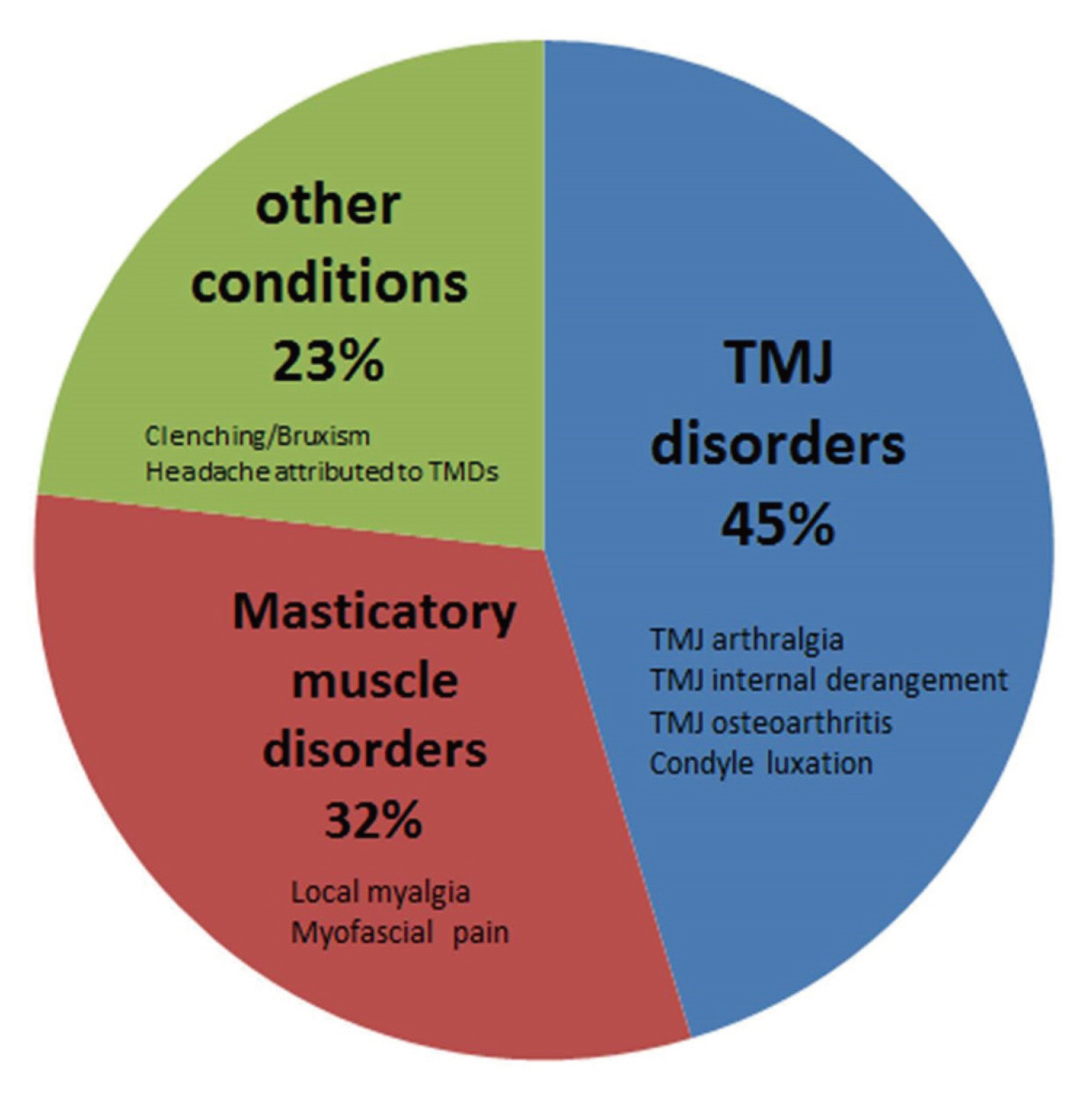
The authors examined 130 TMD patients with TMJ disorders, masticatory muscle disorders, and clenching/bruxism who had received splint therapy (occlusion stabilization splint, anterior positioning splint) of patients who visited the Department of Orofacial Pain and Oral Medicine at Yonsei University Dental Hospital from 2015 to 2020. They were evaluated according to the method to wean splints.
Results
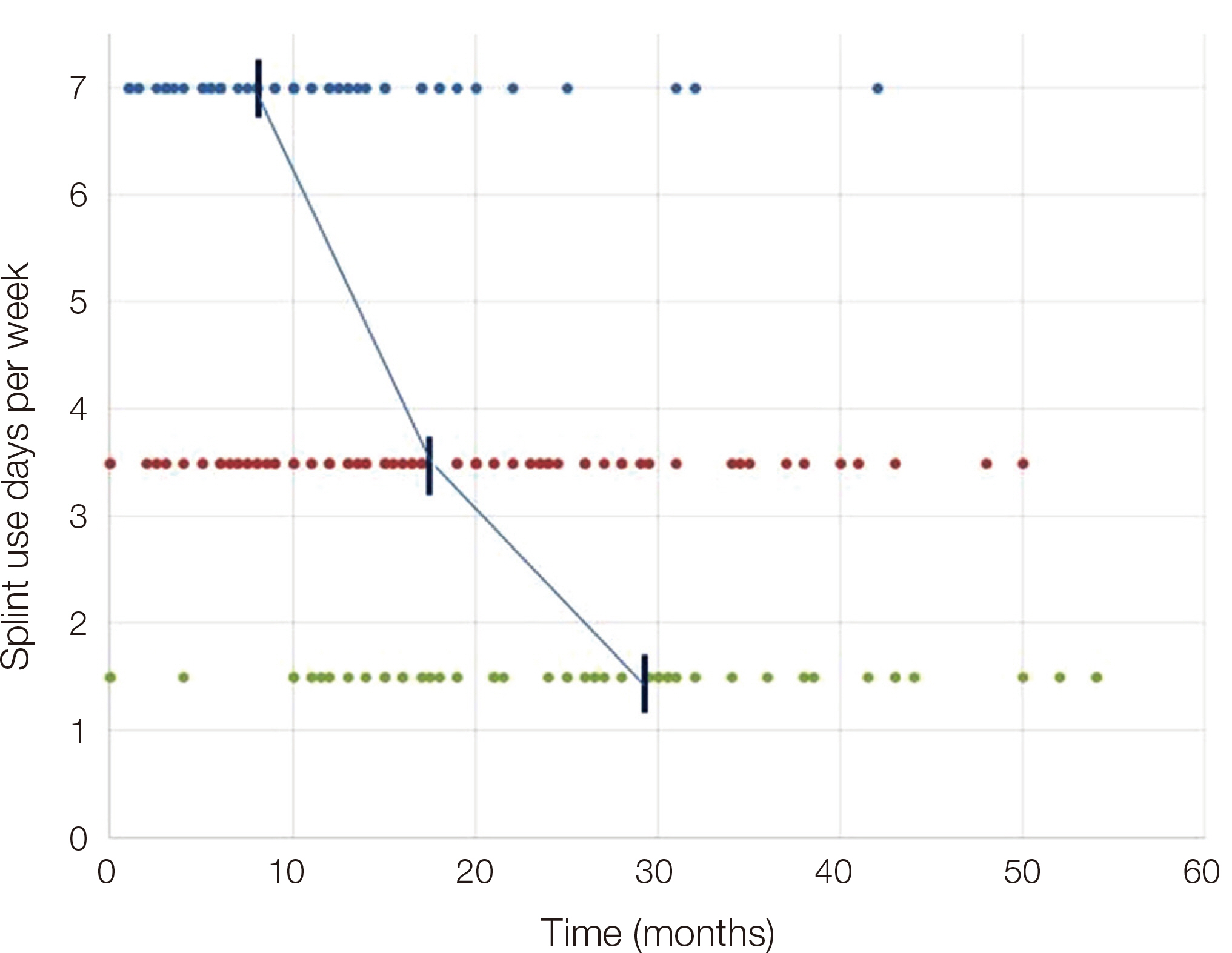
The mean splint therapy period was 29.0 months, during which patients wore splints 7 days a week for 8.4 months, 3 - 4 days a week for 9.5 months, and finally 1 - 2 days a week for 11.1 months (a total of 29.0 months, about 2.5 years).
Conclusion
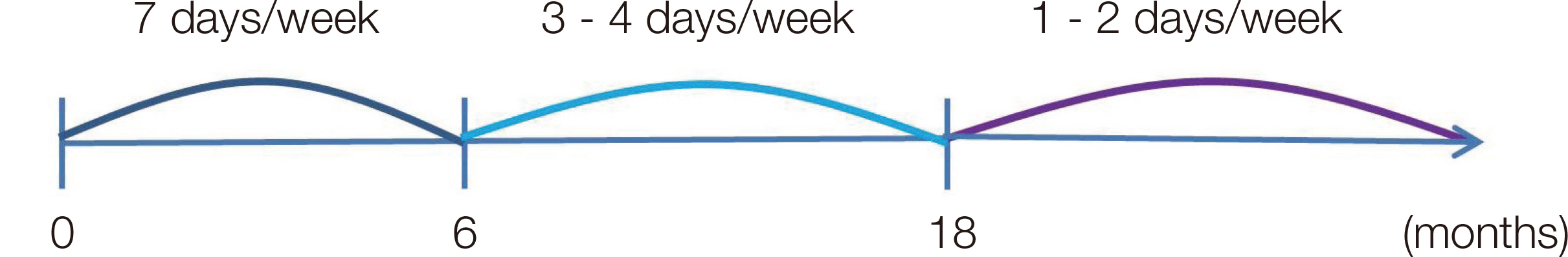
It seems that TMD symptoms can be alleviated and side effects such as occlusal change can be minimized if patients wear a splint 7 days a week for the first 6 months, followed by 3 - 4 days a week for the next 6 to 18 months, and finally 1 - 2 days a week after 18 months.
Figure
Reference
-
References
1. Lee HJ, Kim ST. 2020; A questionnaire-based study of sleep-wake patterns and sleep quality in a TMJ and orofacial pain clinic. Cranio. 38:213–20. DOI: 10.1080/08869634.2018.1550134. PMID: 30477395.2. Alajbeg IZ, Boric Brakus R, Brakus I. 2018; Comparison of amitriptyline with stabilization splint and placebo in chronic TMD patients: a pilot study. Acta Stomatol Croat. 52:114–22. DOI: 10.15644/asc52/2/4. PMID: 30034010. PMCID: PMC6047595.3. Peck CC, Goulet JP, Lobbezoo F, Schiffman EL, Alstergren P, Anderson GC, de Leeuw R, Jensen R, Michelotti A, Ohrbach R, Petersson A, List T. 2014; Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. J Oral Rehabil. 41:2–23. DOI: 10.1111/joor.12132. PMID: 24443898. PMCID: PMC4520529.4. de Resende CMBM, de Oliveira Medeiros FGL, de Figueiredo Rêgo CR, Bispo ASL, Barbosa GAS. 2021; de Analysis of splint weaning in Temporomandibular disorder patients Almeida EO. Short-term effectiveness of conservative therapies in pain, quality of life, and sleep in patients with temporomandibular disorders: A randomized clinical trial. Cranio. 39:335–43. DOI: 10.1080/08869634.2019.1627068. PMID: 31204605.5. Zhang C, Wu JY, Deng DL, He BY, Tao Y, Niu YM, Deng MH. 2016; Efficacy of splint therapy for the management of temporomandibular disorders: a meta-analysis. Oncotarget. 7:84043–53. DOI: 10.18632/oncotarget.13059. PMID: 27823980. PMCID: PMC5356643.6. Akbulut N, Altan A, Akbulut S, Atakan C. 2018; Evaluation of the 3 mm Thickness Splint Therapy on Temporomandibular Joint Disorders (TMDs). Pain Res Manag. 2018:3756587. DOI: 10.1155/2018/3756587. PMID: 30651901. PMCID: PMC6311873.7. Pedroni CR, De Oliveira AS, Guaratini MI. 2003; Prevalence study of signs and symptoms of temporomandibular disorders in university students. J Oral Rehabil. 30:283–9. DOI: 10.1046/j.1365-2842.2003.01010.x. PMID: 12588501.8. Sharma S, Gupta DS, Pal US, Jurel SK. 2011; Etiological factors of temporomandibular joint disorders. Natl J Maxillofac Surg. 2:116–9. DOI: 10.4103/0975-5950.94463. PMID: 22639496. PMCID: PMC3343405.9. van Grootel RJ, Buchner R, Wismeijer D, van der Glas HW. 2017; Towards an optimal therapy strategy for myogenous TMD, physiotherapy compared with occlusal splint therapy in an RCT with therapy-andpatient-specific treatment durations. BMC Musculoskelet Disord. 18:76. DOI: 10.1186/s12891-017-1404-9. PMID: 28183288. PMCID: PMC5301345.10. Furquim BD, Flamengui LM, Conti PC. 2015; TMD and chronic pain: a current view. Dental Press J Orthod. 20:127–33. DOI: 10.1590/2176-9451.20.1.127-133.sar. PMID: 25741834. PMCID: PMC4373025.11. Song YL, Yap AU. 2018; Outcomes of therapeutic TMD interventions on oral health related quality of life: A qualitative systematic review. Quintessence Int. 49:487–96. DOI: 10.3290/j.qi.a40340. PMID: 29700502.12. Armijo-Olivo S, Pitance L, Singh V, Neto F, Thie N, Michelotti A. 2016; Effectiveness of Manual Therapy and Therapeutic Exercise for Temporomandibular Disorders: Systematic Review and Meta-Analysis. Phys Ther. 96:9–25. DOI: 10.2522/ptj.20140548. PMID: 26294683. PMCID: PMC4706597.13. Al-Ani Z, Gray RJ, Davies SJ, Sloan P, Glenny AM. 2005; Stabilization splint therapy for the treatment of temporomandibular myofascial pain: a systematic review. J Dent Educ. 69:1242–50. DOI: 10.1002/j.0022-0337.2005.69.11.tb04023.x. PMID: 16275687.14. Lin SL, Wu SL, Ko SY, Yen CY, Yang JW. 2017; Effect of Flat-Plane Splint Vertical Thickness on Disc Displacement Without Reduction: A Retrospective Matched-Cohort Study. J Oral Maxillofac Surg. 75:1627–36. DOI: 10.1016/j.joms.2016.12.047. PMID: 28157490.15. Klasser GD, Greene CS. 2009; Oral appliances in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 107:212–23. DOI: 10.1016/j.tripleo.2008.10.007. PMID: 19138639.16. He S, Wang S, Song F, Wu S, Chen J, Chen S. 2021; Effect of the use of stabilization splint on masticatory muscle activities in TMD patients with centric relation-maximum intercuspation discrepancy and absence of anterior/lateral guidance. Cranio. 39:424–32. DOI: 10.1080/08869634.2019.1655861. PMID: 31429383.17. Zhu H, He D, Yang Z, Song X, Ellis E 3rd. 2019; The effect of disc repositioning and post-operative functional splint for the treatment of anterior disc displacement in juvenile patients with Class II malocclusion. J Craniomaxillofac Surg. 47:66–72. DOI: 10.1016/j.jcms.2018.09.035. PMID: 30497948.18. Kuzmanovic Pficer J, Dodic S, Lazic V, Trajkovic G, Milic N, Milicic B. 2017; Occlusal stabilization splint for patients with temporomandibular disorders: Metaanalysis of short and long term effects. PLoS One. 12:e0171296. DOI: 10.1371/journal.pone.0171296. PMID: 28166255. PMCID: PMC5293221.19. Nitzan DW. 1994; Intraarticular pressure in the functioning human temporomandibular joint and its alteration by uniform elevation of the occlusal plane. J Oral Maxillofac Surg. 52:671–9. DOI: 10.1016/0278-2391(94)90476-6. PMID: 8006730.20. Vrbanovic E, Alajbeg IZ. 2019; Long-term Effectiveness of Occlusal Splint Therapy Compared to Placebo in Patients with Chronic Temporomandibular Disorders. Acta Stomatol Croat. 53:195–206. DOI: 10.15644/asc53/3/1. PMID: 31749451. PMCID: PMC6820445.21. Perez CV, de Leeuw R, Okeson JP, Carlson CR, Li HF, Bush HM, Falace DA. 2013; The incidence and prevalence of temporomandibular disorders and posterior open bite in patients receiving mandibular advancement device therapy for obstructive sleep apnea. Sleep Breath. 17:323–32. DOI: 10.1007/s11325-012-0695-1. PMID: 22477031.22. Okeson JP. 2013. Management of temporomandibular disorders and occlusion. 7th ed. Elsevier;St. Louis: p. 364.23. Pertes RA, Gross SG. 1995. Clinical management of temporomandibular disorders and orofacial pain. Quintessence Pub;Chicago: p. 65.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recovery from Acute Malocclusion in Temporomandibular Disorders with Stabilization Splint: Case Report
- AN EFFECT OF COMBINATION WITH ARTHROCENTESIS AND STABILIZATION SPLINT TREATMENT ON TEMPOROMANDIBULAR JOINT DISORDER PATIENT
- Clinical Features of the Temporomandibular Disorder Patients with Occlusal Splint Therapy
- Analysis of the clinical symptoms and the temporomandibular joint disk by magnetic resonance imaging after conservative treatment with anterior repositioning splint
- Temporomandibular Joint Disorder and Occlusal Changes: Case Reports