J Dent Rehabil Appl Sci.
2021 Sep;37(3):130-137. 10.14368/jdras.2021.37.3.130.
3D analysis of soft tissue around implant after flap folding suture
- Affiliations
-
- 1Department of Periodontology, College of Dentistry, Dankook University, Cheonan, Republic of Korea
- 2Department of Periodontology, Dankook University Dental Hospital, Cheonan, Republic of Korea
- KMID: 2525987
- DOI: http://doi.org/10.14368/jdras.2021.37.3.130
Abstract
- Purpose
The various suture techniques can be utilized in order to maximize the keratinized tissue healing around dental implants. The aim of this study is to compare the soft tissue healing pattern between two different suture techniques after implant placement.
Materials and Methods
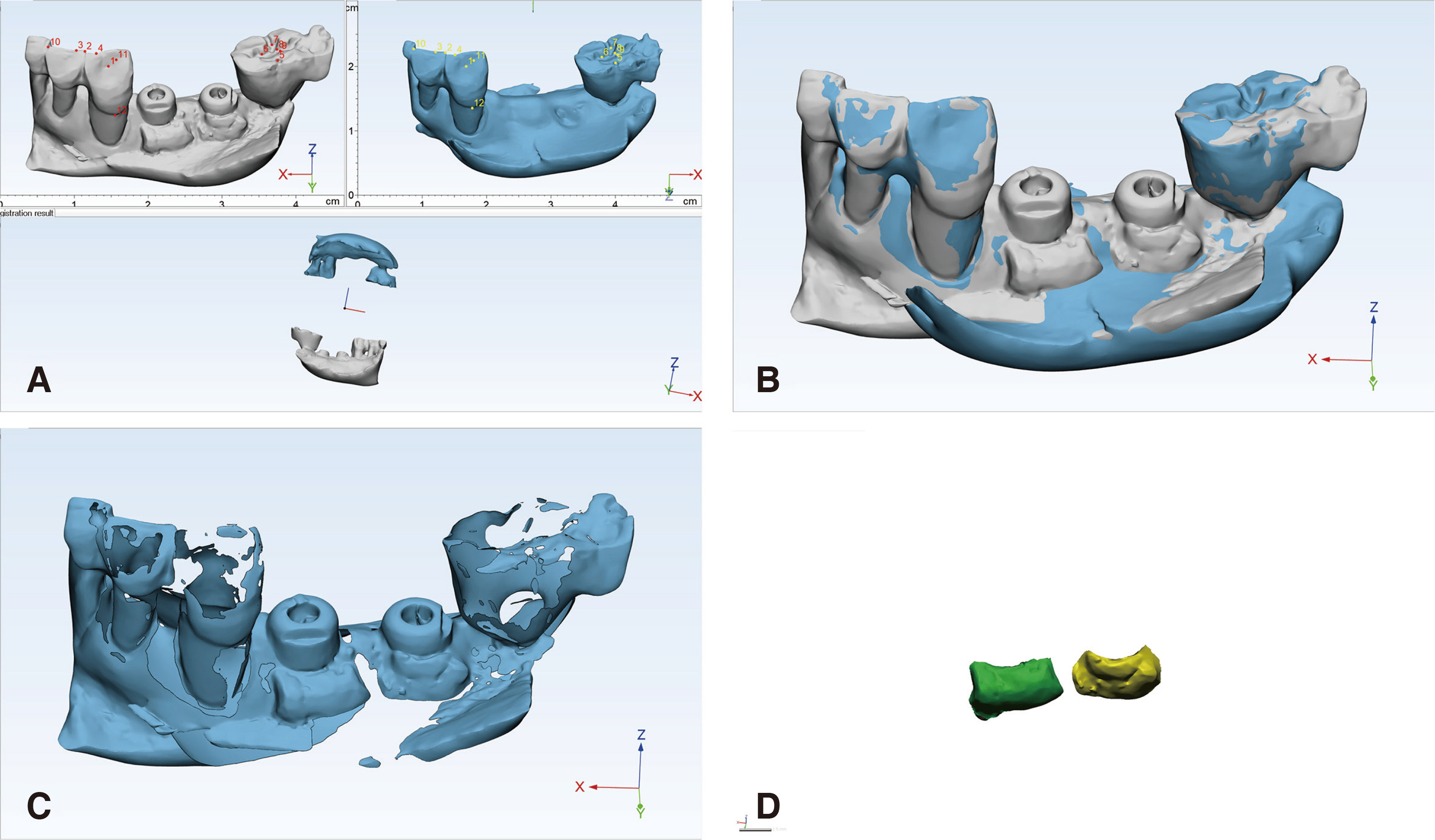
15 patients with 18 implants were enrolled in this study. Simple implant placement without any additional bone graft was performed. Two different suture techniques were used to tug in the mobilized flap near the healing abutment after paramarginal flap design. Digital intraoral scan was performed at baseline, post-operation, stitch out, and 3 months after operation. The scan data were aligned using multiple points such as cusp, fossa of adjacent teeth, and/or healing abutment. After subtracting scan data at baseline with other time-point results, closed space indicating volume increment of peri-implant mucosa was selected. The volume of the close space was measured in mm 3 . The volume between two suture techniques at three time-points was compared using nonparametric rank-based analysis.
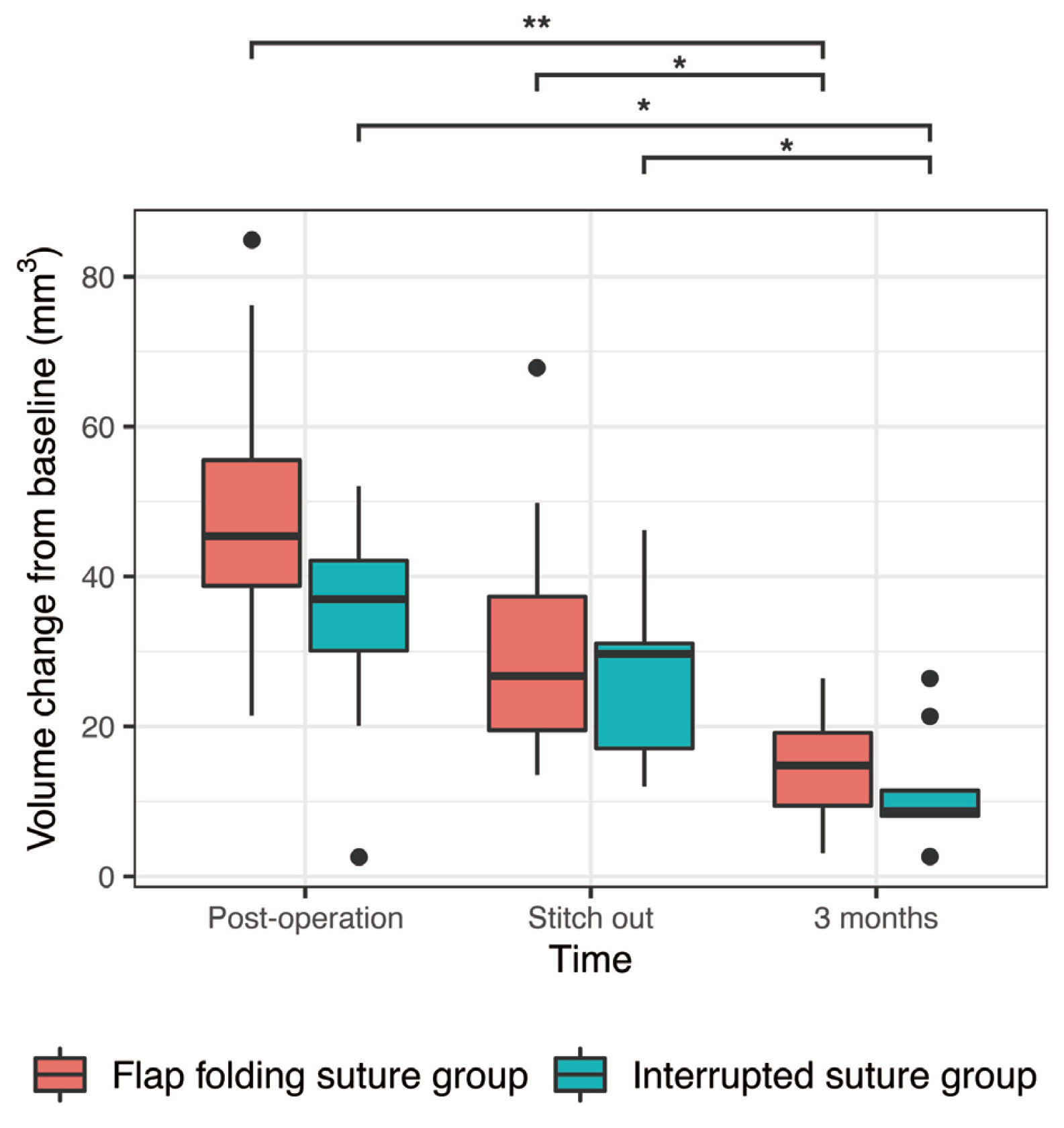
Results
Healing was uneventful in both groups. Both suture technique groups showed increased soft tissue volume immediately after surgery. The amount of volume increment significantly decreased after 3 months (P < 0.001). Flap folding suture group showed higher median of volume increment than interrupted suture group after 3 months without any statistical significance (P > 0.05).
Conclusion
After paramarginal flap reflection, the raised flaps stabilized by flap folding suture showed relatively higher volume maintenance after 3-month healing period. However, further studies are warranted.
Figure
Reference
-
References
1. Sicilia A, Botticelli D, Working G. 2012; Computer-guided implant therapy and soft- and hard-tissue aspects. The Third EAO Consensus Conference 2012. Clin Oral Implants Res. 23 Suppl 6:157–61. DOI: 10.1111/j.1600-0501.2012.02553.x. PMID: 23062140.2. Wennström JL, Derks J. 2012; Is there a need for keratinized mucosa around implants to maintain health and tissue stability? Clin Oral Implants Res. 23 Suppl 6:136–46. DOI: 10.1111/j.1600-0501.2012.02540.x. PMID: 23062138.3. Roccuzzo M, Grasso G, Dalmasso P. 2016; Keratinized mucosa around implants in partially edentulous posterior mandible: 10-year results of a prospective comparative study. Clin Oral Implants Res. 27:491–6. DOI: 10.1111/clr.12563. PMID: 25706508.4. Oh SL, Ji C, Azad S. 2020; Free gingival grafts for implants exhibiting a lack of keratinized mucosa: extended follow-up of a randomized controlled trial. J Clin Periodontol. 47:777–85. DOI: 10.1111/jcpe.13272. PMID: 32096243.5. Thoma DS, Lim HC, Paeng KW, Kim MJ, Jung RE, Hämmerle CHF, Jung UW. 2020; Augmentation of keratinized tissue at tooth and implant sites by using autogenous grafts and collagen-based soft-tissue substitutes. J Clin Periodontol. 47:64–71. DOI: 10.1111/jcpe.13194. PMID: 31518443.6. Park SH, Wang HL. 2012; Pouch roll technique for implant soft tissue augmentation: a variation of the modified roll technique. Int J Periodontics Restorative Dent. 32:e116–21. PMID: 22408781.7. Lim HC, Lee J, Kang DY, Cho IW, Shin HS, Park JC. 2021; Digital assessment of gingival dimensions of healthy periodontium. J Clin Med. 10:1550. DOI: 10.3390/jcm10081550. PMID: 33917248. PMCID: PMC8068027.8. Suárez-López Del Amo F, Lin GH, Monje A, Galindo-Moreno P, Wang HL. 2016; Influence of soft tissue thickness on peri-implant marginal bone loss: a systematic review and meta-analysis. J Periodontol. 87:690–9. DOI: 10.1902/jop.2016.150571. PMID: 26777766.9. Linkevicius T, Apse P, Grybauskas S, Puisys A. 2009; Reaction of crestal bone around implants depending on mucosal tissue thickness. A 1-year prospective clinical study. Stomatologija. 11:83–91. PMID: 19996674.10. Puisys A, Linkevicius T. 2015; The influence of mucosal tissue thickening on crestal bone stability around bone-level implants. A prospective controlled clinical trial. Clin Oral Implants Res. 26:123–9. DOI: 10.1111/clr.12301. PMID: 24313250.11. Noguchi K, Gel YR, Brunner E, Konietschke F. 2012; nparLD: An R software package for the nonparametric analysis of longitudinal data in factorial experiments. J Stat Softw. 50(12):DOI: 10.18637/jss.v050.i12.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Free Vasularized Scapular and Parascapular Flap
- Soft-tissue management for primary closure in immediate implant placement
- A Combined Scapular Flap and Latissimus Dorsi Flap
- Augmentation of the Chin with a Silicone Implant
- Ridge Augmentation Using Vascularized Interpositional Periosteal- Connective Tissue (VIP-CT) in Conjunction with Anterior Implant Placement in Maxilla: Report of Three Cases