J Surg Ultrasound.
2021 Nov;8(2):48-54. 10.46268/jsu.2021.8.2.48.
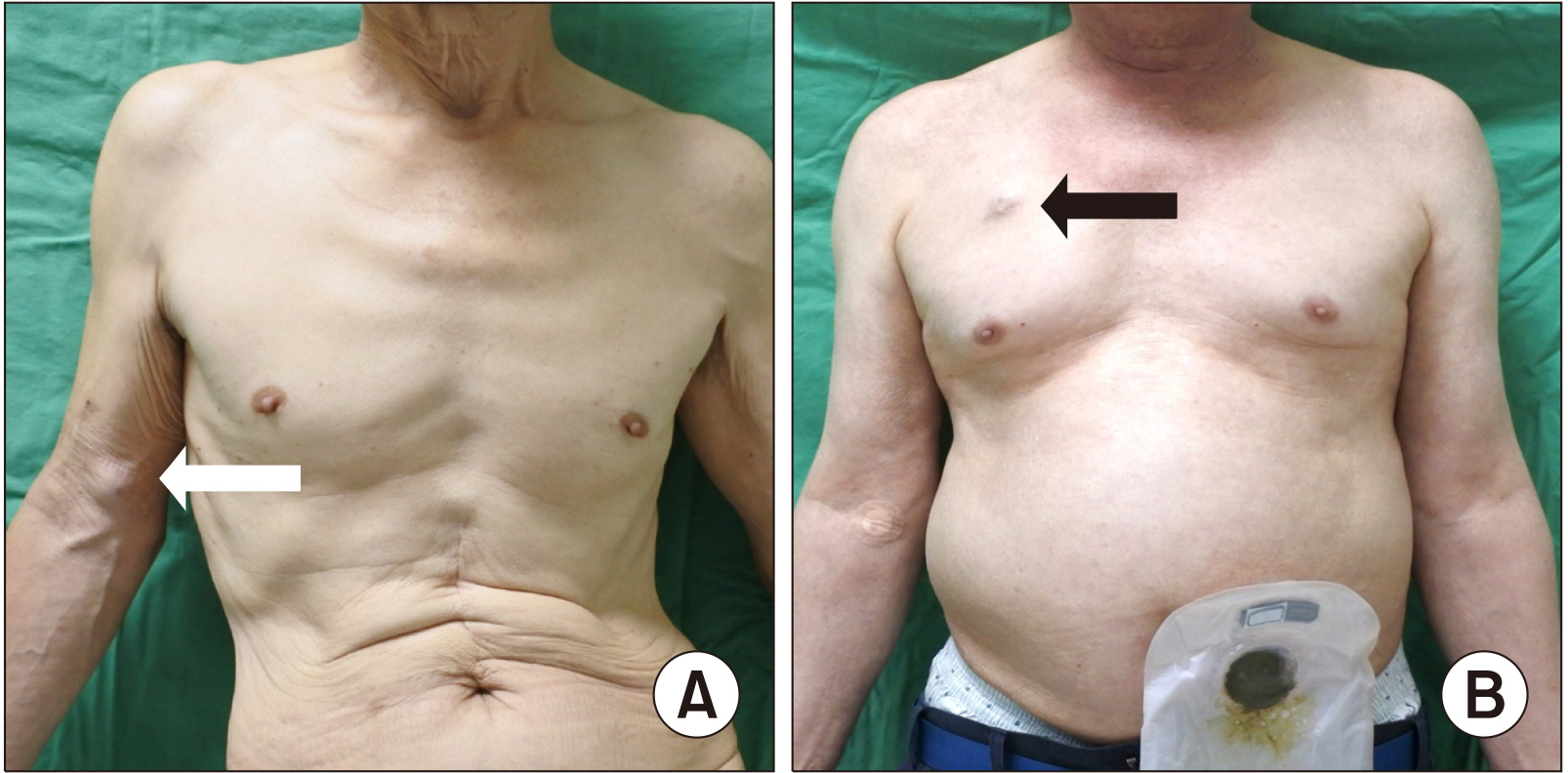
Ultrasound-Guided Totally Implantable Venous Access: Comparison between Arm and Chest Ports in Solid Organ Cancer Patients
- Affiliations
-
- 1Department of Surgery, Jeonbuk National University Medical School and Hospital, Korea
- 2Biomedical Research Institute, Jeonbuk National University Hospital, Korea
- 3Research Institute of Clinical Medicine, Jeonbuk National University, Jeonjuc, Korea
- KMID: 2525884
- DOI: http://doi.org/10.46268/jsu.2021.8.2.48
Abstract
- Purpose
The purpose of this study was to evaluate the safety, technical feasibility, and complications of ultrasound-guided placement of totally implantable venous access ports (TIVAPs) in the arm compared to the chest for patients with cancer in a single center.
Methods
We retrospectively identified 371 patients who underwent TIVAP implantation in the upper arm or chest between July 2018 and June 2019. Implantation via the upper arm (arm port) or the jugular vein (chest port) was performed under sonographic and fluoroscopic guidance after administering local anesthesia. Medical records were reviewed to determine technical success, complications, and the causes of port removal were analyzed.
Results
In total, 371 devices were implanted, 252 in the upper arm (n = 252) and 119 in the upper chest wall (n = 119). The technical success rate was 100%. There were fewer complications observed in the arm port group compared to the chest port group (13 vs 23 patients; 5.2% vs 19.3%), which was statistically significant (P = 0.002). The chest port group developed more complications per 1000 catheter days and had a higher total complication rate than the arm port group (P < 0.001). Local infection with abscess and wound dehiscence were the most common cause of port removal. Multivariate analysis showed that the implantable port in the arm involved a less complicated procedure (P = 0.002).
Conclusion
Implantation of TIVAPs in the upper arm is a safe and feasible procedure with a low rate of complications. TIVAPs in the upper arm may be a good alternative to TIVAPs in the chest.
Keyword
Figure
Reference
-
1. Kato K, Iwasaki Y, Onodera K, Higuchi M, Kato K, Kato Y, et al. 2016; Totally implantable venous access port via the femoral vein in a femoral port position with CT-venography. J Surg Oncol. 114:1024–8. DOI: 10.1002/jso.24441. PMID: 27658579.
Article2. Li G, Zhang Y, Ma H, Zheng J. 2019; Arm port vs chest port: a systematic review and meta-analysis. Cancer Manag Res. 11:6099–112. DOI: 10.2147/CMAR.S205988. PMID: 31308748. PMCID: PMC6613605.3. Gallieni M, Pittiruti M, Biffi R. 2008; Vascular access in oncology patients. CA Cancer J Clin. 58:323–46. DOI: 10.3322/CA.2008.0015. PMID: 18971486.
Article4. Sousa B, Furlanetto J, Hutka M, Gouveia P, Wuerstlein R, Mariz JM, et al. 2015; Central venous access in oncology: ESMO clinical practice guidelines. Ann Oncol. 26 Suppl 5:v152–68. DOI: 10.1093/annonc/mdv296. PMID: 26314776.
Article5. Yang SS, Ahn MS. 2018; A comparison between upper arm and chest for optimal site of totally implanted venous access ports in patients with female breast cancer. Ann Vasc Surg. 50:128–34. DOI: 10.1016/j.avsg.2017.11.059. PMID: 29481918.
Article6. Xu H, Chen R, Jiang C, You S, Zhu Q, Li Y, et al. 2020; Implanting totally implantable venous access ports in the upper arm is feasible and safe for patients with early breast cancer. J Vasc Access. 21:609–14. DOI: 10.1177/1129729819894461. PMID: 31841061.
Article7. Marcy PY, Figl A, Amoretti N, Ianessi A. 2010; Arm port implantation in cancer patients. Int J Clin Oncol. 15:328–30. DOI: 10.1007/s10147-010-0041-1. PMID: 20195679.
Article8. Magallón-Pedrera I, Pérez-Altozano J, Virizuela Echaburu JA, Beato-Zambrano C, Borrega-García P, de la Torre-Montero JC. 2020; ECO-SEOM-SEEO safety recommendations guideline for cancer patients receiving intravenous therapy. Clin Transl Oncol. 22:2049–60. DOI: 10.1007/s12094-020-02347-1. PMID: 32356275. PMCID: PMC7505883.
Article9. Nocito A, Wildi S, Rufibach K, Clavien PA, Weber M. 2009; Randomized clinical trial comparing venous cutdown with the Seldinger technique for placement of implantable venous access ports. Br J Surg. 96:1129–34. DOI: 10.1002/bjs.6730. PMID: 19731229.
Article10. Bertoglio S, Cafiero F, Meszaros P, Varaldo E, Blondeaux E, Molinelli C, et al. 2020; PICC-PORT totally implantable vascular access device in breast cancer patients undergoing chemo-therapy. J Vasc Access. 21:460–6. DOI: 10.1177/1129729819884482. PMID: 31674857.
Article11. Marcy PY, Magné N, Castadot P, Italiano A, Amoretti N, Bailet C, et al. 2007; Is radiologic placement of an arm port mandatory in oncology patients?: analysis of a large bi-institutional experience. Cancer. 110:2331–8. DOI: 10.1002/cncr.23040. PMID: 17886248.
Article12. Kehagias E, Tsetis D. 2019; The "Arm-to-Chest Tunneling" technique: a modified technique for arm placement of implantable ports or central catheters. J Vasc Access. 20:771–7. DOI: 10.1177/1129729819826039. PMID: 30939969.
Article13. 2020; Practice Guidelines for Central Venous Access 2020: an updated report by the American Society of Anesthesiologists Task Force on Central Venous Access. Anesthesiology. 132:8–43. DOI: 10.1097/ALN.0000000000002864. PMID: 31821240.14. Lebeaux D, Larroque B, Gellen-Dautremer J, Leflon-Guibout V, Dreyer C, Bialek S, et al. 2012; Clinical outcome after a totally implantable venous access port-related infection in cancer patients: a prospective study and review of the literature. Medicine (Baltimore). 91:309–18. DOI: 10.1097/MD.0b013e318275ffe1. PMID: 23117849.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety of a Totally Implantable Central Venous Port System with Percutaneous Subclavian Vein Access
- Inversion of Implantable Central Venous Port in Children: 2 cases report
- An analysis of the outcomes of totally implantable access port implantation performed by surgical residents
- Totally Implantable Venous Access Devices In Pediatric Surgery Patients
- Catheter Fracture of a Totally Implantable Venous Device Due to Pinch Off Syndrome in Breast Cancer: A Case Report