Ann Surg Treat Res.
2022 Feb;102(2):110-116. 10.4174/astr.2022.102.2.110.
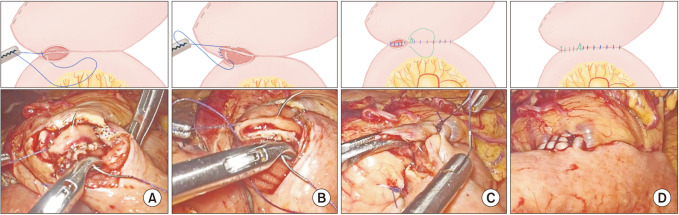
A reinforced suture method for stapled gastrointestinal anastomosis to reduce gastrointestinal hemorrhage during Whipple operation in laparoscopy
- Affiliations
-
- 1Department of Hepatobiliary Surgery, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China
- 2Department of Pathology, Chongqing Medical University, Chongqing, China
- KMID: 2525448
- DOI: http://doi.org/10.4174/astr.2022.102.2.110
Abstract
- Purpose
Laparoscopy is being increasingly accepted for pancreaticoduodenectomy. Stapled anastomosis (SA) is used extensively to facilitate laparoscopic pancreaticoduodenectomy (LPD); however, the incidence of anastomotic bleeding after stapled gastrointestinal anastomosis is still high.
Methods
One hundred and thirty-nine patients who underwent LPD using Whipple method were enrolled in our study. We performed the SA with our reinforced method (n = 68, R method) and without the method (n = 71, NR method). We compared the clinical characteristics and anastomosis methods of patients with or without gastrointestinal-anastomotic hemorrhage (GAH), and operative parameters were also compared between the anastomotic methods.
Results
Of the 139 patients undergoing LPD, 15 of them developed GAH. The clinical characteristics of patients with or without GAH were not significantly different except in the anastomotic method (P < 0.001). In the univariate logistic regression analyses, only the anastomotic method was associated with GAH. Furthermore, patients with the NR method had significantly higher incidences of GAH (P < 0.001) and Clavien-Dindo grade ≥ III complications (P < 0.001).
Conclusion
Our retrospective analysis showed that the SA performed with reinforced method might be a reform of SA without the reinforcement, as indicated by the lower incidence of GAH. However, further research is necessary to evaluate the utility of this reinforced method.
Figure
Reference
-
1. de Rooij T, Klompmaker S, Abu Hilal M, Kendrick ML, Busch OR, Besselink MG. Laparoscopic pancreatic surgery for benign and malignant disease. Nat Rev Gastroenterol Hepatol. 2016; 13:227–238. PMID: 26882881.
Article2. Gagner M, Pomp A. Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc. 1994; 8:408–410. PMID: 7915434.
Article3. Wang M, Peng B, Liu J, Yin X, Tan Z, Liu R, et al. Practice patterns and perioperative outcomes of laparoscopic pancreaticoduodenectomy in China: a retrospective multicenter analysis of 1029 patients. Ann Surg. 2021; 273:145–153. PMID: 30672792.
Article4. Liu BW, Liu Y, Liu JR, Feng ZX. Comparison of hand-sewn and stapled anastomoses in surgeries of gastrointestinal tumors based on clinical practice of China. World J Surg Oncol. 2014; 12:292. PMID: 25240386.
Article5. Sandini M, Ruscic KJ, Ferrone CR, Qadan M, Eikermann M, Warshaw AL, et al. Major complications independently increase long-term mortality after pancreatoduodenectomy for cancer. J Gastrointest Surg. 2019; 23:1984–1990. PMID: 30225794.
Article6. Lubrano J, Bachelier P, Paye F, Le Treut YP, Chiche L, Sa-Cunha A, et al. Severe postoperative complications decrease overall and disease free survival in pancreatic ductal adenocarcinoma after pancreaticoduodenectomy. Eur J Surg Oncol. 2018; 44:1078–1082. PMID: 29685757.
Article7. Kondo N, Murakami Y, Uemura K, Nakagawa N, Okada K, Takahashi S, et al. Prognostic impact of postoperative complication after pancreatoduodenectomy for pancreatic adenocarcinoma stratified by the resectability status. J Surg Oncol. 2018; 118:1105–1114. PMID: 29878355.
Article8. Ravitch MM, Steichen FM. A stapling instrument for end-to-end inverting anastomoses in the gastrointestinal tract. Ann Surg. 1979; 189:791–797. PMID: 453950.
Article9. Hajibandeh S, Hajibandeh S, Khan RM, Malik S, Mansour M, Kausar A, et al. Stapled anastomosis versus hand-sewn anastomosis of gastro/duodenojejunotomy in pancreaticoduodenectomy: a systematic review and meta-analysis. Int J Surg. 2017; 48:1–8. PMID: 28987557.
Article10. Zhou J, Xin C, Xia T, Mou Y, Xu X, Zhang R, et al. Laparoscopic pancreaticoduodenectomy in A-92-older Chinese patient for cancer of head of the pancreas: a case report. Medicine (Baltimore). 2017; 96:e5962. PMID: 28099362.11. Guo CX, Shen YN, Zhang Q, Zhang XZ, Wang JL, Gao SL, et al. Prediction of postoperative pancreatic fistula using a nomogram based on the updated definition. Ann Surg Treat Res. 2020; 98:72–81. PMID: 32051815.
Article12. Wu MB, Zhang WF, Zhang YL, Mu D, Gong JP. Choledochoduodenal fistula in Mainland China: a review of epidemiology, etiology, diagnosis and management. Ann Surg Treat Res. 2015; 89:240–246. PMID: 26576403.
Article13. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007; 142:761–768. PMID: 17981197.
Article14. Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007; 142:20–25. PMID: 17629996.
Article15. Baker MS, Sherman KL, Stocker SJ, Hayman AV, Bentrem DJ, Prinz RA, et al. Using a modification of the Clavien-Dindo system accounting for readmissions and multiple interventions: defining quality for pancreaticoduodenectomy. J Surg Oncol. 2014; 110:400–406. PMID: 24861871.
Article16. Li T, D’Cruz RT, Lim SY, Shelat VG. Somatostatin analogues and the risk of post-operative pancreatic fistulas after pancreatic resection: a systematic review & meta-analysis. Pancreatology. 2020; 20:158–168. PMID: 31980352.
Article17. Bollo J, Turrado V, Rabal A, Carrillo E, Gich I, Martinez MC, et al. Randomized clinical trial of intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy (IEA trial). Br J Surg. 2020; 107:364–372. PMID: 31846067.
Article18. Allaix ME, Degiuli M, Bonino MA, Arezzo A, Mistrangelo M, Passera R, et al. Intracorporeal or extracorporeal ileocolic anastomosis after laparoscopic right colectomy: a double-blinded randomized controlled trial. Ann Surg. 2019; 270:762–767. PMID: 31592811.
Article19. Hemming K, Pinkney T, Futaba K, Pennant M, Morton DG, Lilford RJ. A systematic review of systematic reviews and panoramic meta-analysis: staples versus sutures for surgical procedures. PLoS One. 2013; 8:e75132. PMID: 24116028.
Article20. Murata Y, Tanemura A, Kato H, Kuriyama N, Azumi Y, Kishiwada M, et al. Superiority of stapled side-to-side gastrojejunostomy over conventional hand-sewn end-to-side gastrojejunostomy for reducing the risk of primary delayed gastric emptying after subtotal stomach-preserving pancreaticoduodenectomy. Surg Today. 2017; 47:1007–1017. PMID: 28337543.
Article21. Sakamoto Y, Kajiwara T, Esaki M, Shimada K, Nara S, Kosuge T. Roux-en-Y reconstruction using staplers during pancreaticoduodenectomy: results of a prospective preliminary study. Surg Today. 2009; 39:32–37. PMID: 19132465.
Article22. Vâlcea S, Beuran M, Vartic M. Intraluminal postpancreatoduodenectomy hemorrhage: last 5 years experience. Chirurgia (Bucur). 2017; 112:39–45. PMID: 28266291.
Article23. Kim KH, Kim MC, Jung GJ, Jang JS, Choi SR. Endoscopic treatment and risk factors of postoperative anastomotic bleeding after gastrectomy for gastric cancer. Int J Surg. 2012; 10:593–597. PMID: 23022923.
Article24. Balachandran P, Sikora SS, Raghavendra Rao RV, Kumar A, Saxena R, Kapoor VK. Haemorrhagic complications of pancreaticoduodenectomy. ANZ J Surg. 2004; 74:945–950. PMID: 15550080.
Article25. Choi YY, Bae J, Hur KY, Choi D, Kim YJ. Reinforcing the staple line during laparoscopic sleeve gastrectomy: does it have advantages?: a meta-analysis. Obes Surg. 2012; 22:1206–1213. PMID: 22661018.
Article26. Sakamoto Y, Hori S, Oguro S, Arita J, Kishi Y, Nara S, et al. Delayed gastric emptying after stapled versus hand-sewn anastomosis of duodenojejunostomy in pylorus-preserving pancreaticoduodenectomy: a randomized controlled trial. J Gastrointest Surg. 2016; 20:595–603. PMID: 26403716.
Article27. Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992; 111:518–526. PMID: 1598671.28. Wang WG, Babu SR, Wang L, Chen Y, Tian BL, He HB. Use of Clavien-Dindo classification in evaluating complications following pancreaticoduodenectomy in 1,056 cases: a retrospective analysis from one single institution. Oncol Lett. 2018; 16:2023–2029. PMID: 30008896.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Study of Delayed Gastric Emptying between Manual and Stapled Anastomosis in Patients Undergoing Subtotal Gastrectomy with Billroth I Gastroduodenostomy for Early Gastric Cancer
- Fish-Mouth Closure of the Pancreatic Stump and Parachuting of the Pancreatic End with Double U Trans-Pancreatic Sutures for Pancreatico-Jejunostomy
- Large Cavernous Hemangioma in the Jejunum of a 2-year-old Boy Treated by Laparoscopy-assisted Resection
- Major Pelvic Bleeding Following a Stapled Transanal Rectal Resection: Use of Laparoscopy as a Diagnostic Tool
- Mid-term Outcomes of Side-to-Side Stapled Anastomosis in Cervical Esophagogastrostomy