Intest Res.
2022 Jan;20(1):124-133. 10.5217/ir.2020.00050.
An evaluation of dietary adequacy among patients with constipation-predominant irritable bowel syndrome in Malaysia
- Affiliations
-
- 1Department of Medicine, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
- 2Dietetics Programme, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
- 3GUT Research Group, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
- 4Department of Physiology, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
- 5Gastroenterology Unit, Department of Medicine, UKM Medical Centre, Kuala Lumpur, Malaysia
- KMID: 2525079
- DOI: http://doi.org/10.5217/ir.2020.00050
Abstract
- Background/Aims
Substantial proportions of patients with constipation-predominant irritable bowel syndrome (IBS-C) linked their symptoms with particular intake of foods. However, there is lack of current data regarding the intake among IBS-C patients before any dietary interventions. Thus, this study aimed to evaluate the dietary adequacy among IBS-C against the standard recommended nutrient intake (RNI) and healthy controls.
Methods
A retrospective case-control study was conducted involving IBS-C patients and healthy control subjects. A validated 126-food items frequency questionnaire was administered to all the subjects to assess their dietary intake, guided by dietitians. The calculated nutrients intake for IBS-C patients was then compared against the standard RNI and healthy controls.
Results
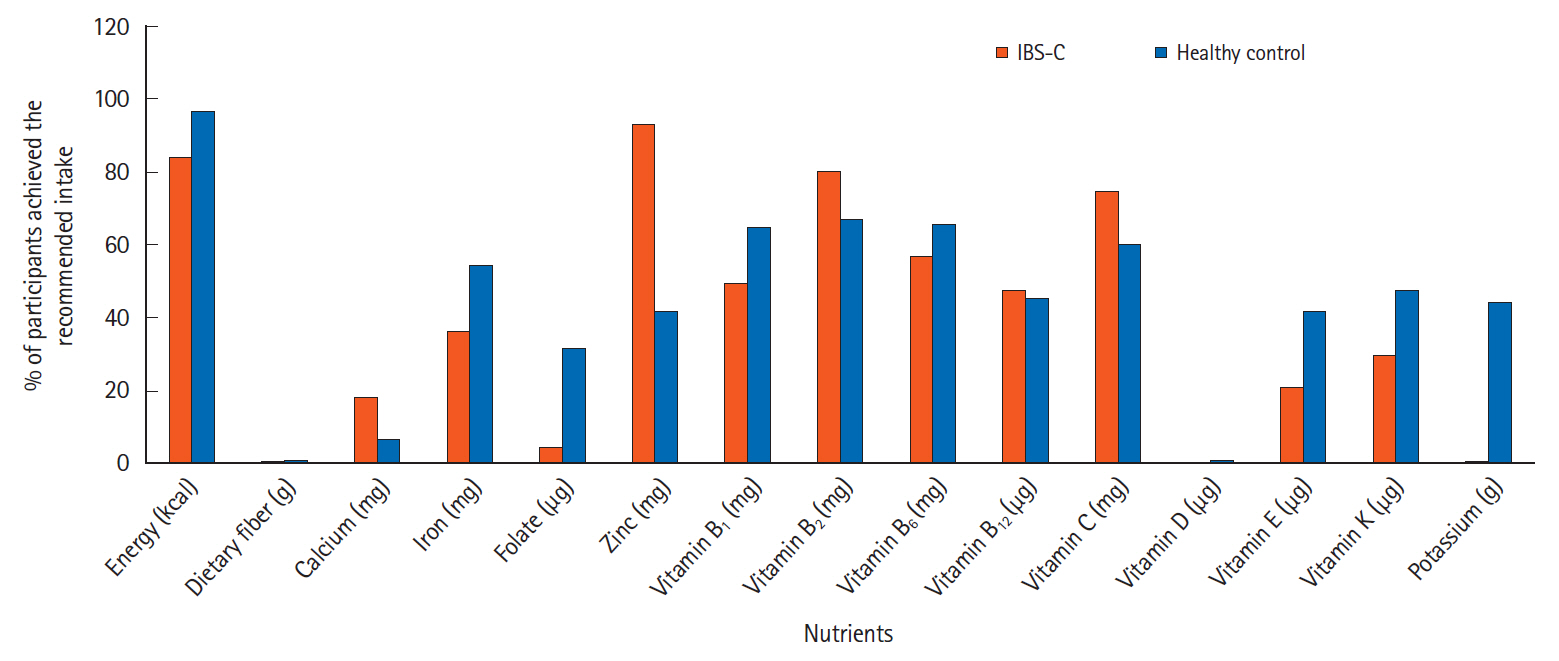
A total of 306 subjects were recruited, among which 218 were diagnosed with IBS-C and 88 were included as healthy controls. IBS-C patients had significantly lower intake of wholegrain products, fried foods, dairy products, fruits, and vegetables compared to healthy controls. The daily intake of energy, certain macronutrients, and micronutrients among IBS-C patients was significantly lower than the healthy subjects. Less than 5% of IBS-C patients and healthy subjects achieved the standard recommendation for dietary fiber. Also, various vitamin intake (B1, B2, B6, folate, B12, E, K, and potassium) among IBS-C patients did not meet the standard RNI.
Conclusions
Dietary intakes of IBS-C patients did not meet the recommended intake for Malaysian and showed the nutritional inadequacies compared to the control subjects. Our study highlighted the importance of dietary evaluation prior to planning strategies for dietary intervention targeting IBS-C patients.
Figure
Cited by 1 articles
-
An Asian perspective on irritable bowel syndrome
Kee Wook Jung, Seung-Jae Myung
Intest Res. 2023;21(2):189-195. doi: 10.5217/ir.2021.00136.
Reference
-
1. Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015; 313:949–958.2. Tillisch K, Labus JS, Naliboff BD, et al. Characterization of the alternating bowel habit subtype in patients with irritable bowel syndrome. Am J Gastroenterol. 2005; 100:896–904.
Article3. Basandra S, Bajaj D. Epidemiology of dyspepsia and irritable bowel syndrome (IBS) in medical students of northern India. J Clin Diagn Res. 2014; 8:JC13–JC16.4. Grundmann O, Yoon SL. Irritable bowel syndrome: epidemiology, diagnosis and treatment: an update for health-care practitioners. J Gastroenterol Hepatol. 2010; 25:691–699.
Article5. Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012; 10:712–721.
Article6. Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002; 123:2108–2131.
Article7. Tan YM, Goh KL, Muhidayah R, Ooi CL, Salem O. Prevalence of irritable bowel syndrome in young adult Malaysians: a survey among medical students. J Gastroenterol Hepatol. 2003; 18:1412–1416.
Article8. Bensoussan A, Kellow JE, Bourchier SJ, et al. Efficacy of a Chinese herbal medicine in providing adequate relief of constipation-predominant irritable bowel syndrome: a randomized controlled trial. Clin Gastroenterol Hepatol. 2015; 13:1946–1954.
Article9. Shepherd SJ, Lomer MC, Gibson PR. Short-chain carbohydrates and functional gastrointestinal disorders. Am J Gastroenterol. 2013; 108:707–717.
Article10. Zhu Y, Zheng X, Cong Y, et al. Bloating and distention in irritable bowel syndrome: the role of gas production and visceral sensation after lactose ingestion in a population with lactase deficiency. Am J Gastroenterol. 2013; 108:1516–1525.
Article11. Vazquez-Roque MI, Camilleri M, Smyrk T, et al. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: effects on bowel frequency and intestinal function. Gastroenterology. 2013; 144:903–911.
Article12. Rao SS, Yu S, Fedewa A. Systematic review: dietary fibre and FODMAP-restricted diet in the management of constipation and irritable bowel syndrome. Aliment Pharmacol Ther. 2015; 41:1256–1270.
Article13. Didari T, Mozaffari S, Nikfar S, Abdollahi M. Effectiveness of probiotics in irritable bowel syndrome: updated systematic review with meta-analysis. World J Gastroenterol. 2015; 21:3072–3084.
Article14. McKenzie YA, Bowyer RK, Leach H, et al. British Dietetic Association systematic review and evidence-based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update). J Hum Nutr Diet. 2016; 29:549–575.
Article15. Simrén M, Månsson A, Langkilde AM, et al. Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion. 2001; 63:108–115.
Article16. Böhn L, Störsrud S, Törnblom H, Bengtsson U, Simrén M. Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. Am J Gastroenterol. 2013; 108:634–641.
Article17. Hayes PA, Fraher MH, Quigley EM. Irritable bowel syndrome: the role of food in pathogenesis and management. Gastroenterol Hepatol (N Y). 2014; 10:164–174.18. Cuomo R, Andreozzi P, Zito FP, Passananti V, De Carlo G, Sarnelli G. Irritable bowel syndrome and food interaction. World J Gastroenterol. 2014; 20:8837–8845.19. Torres MJ, Sabate JM, Bouchoucha M, Buscail C, Hercberg S, Julia C. Food consumption and dietary intakes in 36,448 adults and their association with irritable bowel syndrome: Nutrinet-Santé study. Therap Adv Gastroenterol. 2018; 11:1756283X17746625.
Article20. Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology. 2016; 150:1393–1407.
Article21. Ministry of Health Malaysia, Nutrition Section, Family Health Development Division. Malaysian Adult Nutrition Survey 2003: Methodology. Putrajaya: Ministry of Health Malaysia;2008.22. Leong-Salobir C. Food culture in colonial Asia: a taste of empire. Hoboken: Taylor & Francis;2011.23. Raji MNA, Ab Karim S, Ishak FAC, Arshad MM. Past and present practices of the Malay food heritage and culture in Malaysia. J Ethn Food. 2017; 4:221–231.
Article24. Suzana S, Noor Aini MY, Nik Shanita S, Rafidah G, Roslina A. Atlas of food exchanges and portion sizes. 2nd ed. Kuala Lumpur: MDC Publishers;2009.25. Norimah AK Jr, Safiah M, Jamal K, et al. Food consumption patterns: findings from the Malaysian Adult Nutrition Survey (MANS). Malays J Nutr. 2008; 14:25–39.26. Tee ES, Mohd Ismail N, Mohd Nasir A, Khatijah I. Nutrients composition of Malaysian foods. 4th ed. Kuala Lumpur: Malaysian Food Composition Database Programme c/o Institute for Medical Research;1997.27. Gibson PR. Food intolerance in functional bowel disorders. J Gastroenterol Hepatol. 2011; 26 Suppl 3:128–131.
Article28. Mullin GE, Shepherd SJ, Chander Roland B, Ireton-Jones C, Matarese LE. Irritable bowel syndrome: contemporary nutrition management strategies. JPEN J Parenter Enteral Nutr. 2014; 38:781–799.29. Williams EA, Nai X, Corfe BM. Dietary intakes in people with irritable bowel syndrome. BMC Gastroenterol. 2011; 11:9.
Article30. Böhn L, Störsrud S, Simrén M. Nutrient intake in patients with irritable bowel syndrome compared with the general population. Neurogastroenterol Motil. 2013; 25:23–30.
Article31. Stevenson C, Blaauw R, Fredericks E, Visser J, Stevenson S. Food avoidance in irritable bowel syndrome leads to a nutrition-deficient diet. South Afr J Clin Nutr. 2014; 27:25–30.
Article32. Faresjö A, Johansson S, Faresjö T, Roos S, Hallert C. Sex differences in dietary coping with gastrointestinal symptoms. Eur J Gastroenterol Hepatol. 2010; 22:327–333.
Article33. Moayyedi P, Quigley EM, Lacy BE, et al. The effect of fiber supplementation on irritable bowel syndrome: a systematic review and meta-analysis. Am J Gastroenterol. 2014; 109:1367–1374.
Article34. El-Salhy M, Ystad SO, Mazzawi T, Gundersen D. Dietary fiber in irritable bowel syndrome (Review). Int J Mol Med. 2017; 40:607–613.
Article35. Gibson PR. History of the low FODMAP diet. J Gastroenterol Hepatol. 2017; 32 Suppl 1:5–7.
Article36. Ong DK, Mitchell SB, Barrett JS, et al. Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. J Gastroenterol Hepatol. 2010; 25:1366–1373.
Article37. Eswaran S, Muir J, Chey WD. Fiber and functional gastrointestinal disorders. Am J Gastroenterol. 2013; 108:718–727.
Article38. Wong Z, Mok CZ, Majid HA, Mahadeva S. Early experience with a low FODMAP diet in Asian patients with irritable bowel syndrome. JGH Open. 2018; 2:178–181.
Article39. Feinle-Bisset C, Azpiroz F. Dietary lipids and functional gastrointestinal disorders. Am J Gastroenterol. 2013; 108:737–747.
Article40. Simrén M, Abrahamsson H, Björnsson ES. Lipid-induced colonic hypersensitivity in the irritable bowel syndrome: the role of bowel habit, sex, and psychologic factors. Clin Gastroenterol Hepatol. 2007; 5:201–208.
Article41. Ostgaard H, Hausken T, Gundersen D, El-Salhy M. Diet and effects of diet management on quality of life and symptoms in patients with irritable bowel syndrome. Mol Med Rep. 2012; 5:1382–1390.42. El-Salhy M, Gundersen D. Diet in irritable bowel syndrome. Nutr J. 2015; 14:36.
Article43. Dugum M, Barco K, Garg S. Managing irritable bowel syndrome: the low-FODMAP diet. Cleve Clin J Med. 2016; 83:655–662.
Article44. Ikechi R, Fischer BD, DeSipio J, Phadtare S. Irritable bowel syndrome: clinical manifestations, dietary influences, and management. Healthcare (Basel). 2017; 5:21.
Article45. Shepherd SJ, Halmos E, Glance S. The role of FODMAPs in irritable bowel syndrome. Curr Opin Clin Nutr Metab Care. 2014; 17:605–609.
Article46. Tuck C, Barrett J. Re-challenging FODMAPs: the low FODMAP diet phase two. J Gastroenterol Hepatol. 2017; 32 Suppl 1:11–15.
Article47. Lenhart A, Ferch C, Shaw M, Chey WD. Use of dietary management in irritable bowel syndrome: results of a survey of over 1500 United States Gastroenterologists. J Neurogastroenterol Motil. 2018; 24:437–451.
Article48. Barrett JS. How to institute the low-FODMAP diet. J Gastroenterol Hepatol. 2017; 32 Suppl 1:8–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Irritable Bowel Syndrome
- Differences of Anorectal Manometry Between Diarrhea- and Constipation-predominant Irritable Bowel Syndrome
- Association Between Constipation-Predominant Irritable Bowel Syndrome and Dietary Habits of the Elderly Aged Over 65
- Emerging Pharmacologic Therapies for Constipation-predominant Irritable Bowel Syndrome and Chronic Constipation
- Anxiety, Depression and Sleep Disturbance in Female Constipation Predominant Irritable Bowel Syndrome