J Yeungnam Med Sci.
2022 Jan;39(1):18-23. 10.12701/yujm.2021.01109.
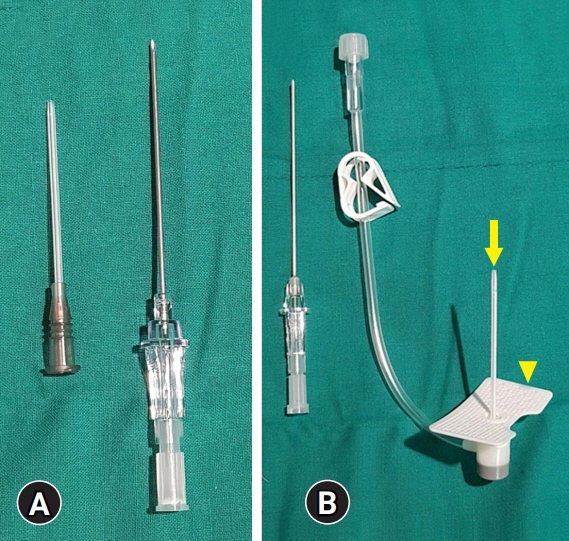
Puncture needle with a hard plastic sheath and plastic wings minimizes repuncture attempts in ultrasound-guided paracentesis: a retrospective case-control study
- Affiliations
-
- 1Department of Radiology, Dongnam Institution of Radiological & Medical Sciences, Busan, Korea
- 2Department of Radiology, Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea
- 3Department of Radiology, Busan Medical Center, Busan, Korea
- 4Department of Internal Medicine, Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea
- KMID: 2525023
- DOI: http://doi.org/10.12701/yujm.2021.01109
Abstract
- Background
This study was performed to evaluate periprocedural factors, complications, and repuncture rate of the newly developed puncture needle and compare it with the routinely used puncture needle for ultrasound (US)-guided paracentesis.
Methods
We retrospectively identified 137 patients who underwent US-guided paracentesis between July 2018 and March 2019. Among them, 82 patients underwent US-guided paracentesis with a newly developed puncture needle. The other 55 patients underwent US-guided paracentesis with a routinely used puncture needle. The periprocedural factors, complications, and repuncture rate were compared between the two groups using the Mann-Whitney U test and Fisher exact test. The repuncture-associated factors were assessed using logistic regression analysis.
Results
There were no major or minor complications in either group. The rate of repuncture was significantly lower in the group using the newly developed puncture needle compared with the group using the routinely used puncture needle (p=0.01). The duration of the procedure was significantly shorter with the newly developed puncture needle compared with the routinely used puncture needle (p=0.01). In univariate analysis, the thickness of the abdominal wall (p=0.04) and the use of the newly developed puncture needle (p=0.01) were significantly associated with the rate of repuncture. In multivariate analysis, only the use of the newly developed puncture needle was significantly associated with the rate of repuncture.
Conclusion
Using this novel puncture needle with a hard plastic sheath and plastic wings, the rate of repuncture and the duration of the procedure were decreased without complications of US-guided paracentesis.
Keyword
Figure
Reference
-
References
1. European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010; 53:397–417.2. Hwangbo Y, Jung JH, Shim J, Kim BH, Jung SH, Lee CK, et al. Etiologic and laboratory analyses of ascites in patients who underwent diagnostic paracentesis. Korean J Hepatol. 2007; 13:185–95.3. Ginés P, Quintero E, Arroyo V, Terés J, Bruguera M, Rimola A, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1987; 7:122–8.4. Moore KP, Wong F, Gines P, Bernardi M, Ochs A, Salerno F, et al. The management of ascites in cirrhosis: report on the consensus conference of the International Ascites Club. Hepatology. 2003; 38:258–66.5. Runyon BA, Montano AA, Akriviadis EA, Antillon MR, Irving MA, McHutchison JG. The serum-ascites albumin gradient is superior to the exudate-transudate concept in the differential diagnosis of ascites. Ann Intern Med. 1992; 117:215–20.6. al Karawi MA, Mohamed AE, Yasawy MI, Graham DY, Shariq S, Ahmed AM, et al. Protean manifestation of gastrointestinal tuberculosis: report on 130 patients. J Clin Gastroenterol. 1995; 20:225–32.7. Runyon BA; AASLD Practice Guidelines Committee. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009; 49:2087–107.8. Poonawala A, Nair SP, Thuluvath PJ. Prevalence of obesity and diabetes in patients with cryptogenic cirrhosis: a case-control study. Hepatology. 2000; 32(4 Pt 1):689–92.9. DeSitter L, Rector WG Jr. The significance of bloody ascites in patients with cirrhosis. Am J Gastroenterol. 1984; 79:136–8.10. Runyon BA, Akriviadis EA, Keyser AJ. The opacity of portal hypertension-related ascites correlates with the fluid’s triglyceride concentration. Am J Clin Pathol. 1991; 96:142–3.11. Moore KP, Aithal GP. Guidelines on the management of ascites in cirrhosis. Gut. 2006; 55(Suppl 6):vi1–12.12. Evans TW. Review article: albumin as a drug. Biological effects of albumin unrelated to oncotic pressure. Aliment Pharmacol Ther. 2002; 16(Suppl 5):6–11.13. Cho J, Jensen TP, Reierson K, Mathews BK, Bhagra A, Franco-Sadud R, et al. Recommendations on the use of ultrasound guidance for adult abdominal paracentesis: a position statement of the Society of Hospital Medicine. J Hosp Med. 2019; 14:E7–15.14. Omary RA, Bettmann MA, Cardella JF, Bakal CW, Schwartzberg MS, Sacks D, et al. Quality improvement guidelines for the reporting and archiving of interventional radiology procedures. J Vasc Interv Radiol. 2003; 14(9 Pt 2):S293–5.15. Tirkes T, Sandrasegaran K, Patel AA, Hollar MA, Tejada JG, Tann M, et al. Peritoneal and retroperitoneal anatomy and its relevance for cross-sectional imaging. Radiographics. 2012; 32:437–51.16. Churg A, Cagle PT, Roggli VL. Tumors of the serosal membranes. Washington, DC: American Registry of Pathology;2006.17. Hanbidge AE, Lynch D, Wilson SR. US of the peritoneum. Radiographics. 2003; 23:663–84.18. Runyon BA. Paracentesis of ascitic fluid. A safe procedure. Arch Intern Med. 1986; 146:2259–61.19. McVay PA, Toy PT. Lack of increased bleeding after paracentesis and thoracentesis in patients with mild coagulation abnormalities. Transfusion. 1991; 31:164–71.20. Pache I, Bilodeau M. Severe haemorrhage following abdominal paracentesis for ascites in patients with liver disease. Aliment Pharmacol Ther. 2005; 21:525–9.21. Mercaldi CJ, Lanes SF. Ultrasound guidance decreases complications and improves the cost of care among patients undergoing thoracentesis and paracentesis. Chest. 2013; 143:532–8.22. Patel PA, Ernst FR, Gunnarsson CL. Evaluation of hospital complications and costs associated with using ultrasound guidance during abdominal paracentesis procedures. J Med Econ. 2012; 15:1–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A 45degrees set Square Method for Accurate Needle Insertion in Ultrasound-guided Internal Jugular Venous Catheterization
- Fine-Needle Biopsy: Should This Be the First Choice in Endoscopic Ultrasound-Guided Tissue Acquisition?
- Stent occlusion in endoscopic ultrasound-guided gallbladder drainage from bleeding mitigated by double pigtail plastic stent deployment within lumen apposing metal stent
- A New Ultrasound-Guided Puncture Device with Augmented Degrees of Performance Freedom and Ability to Attach to Most Convex Probes
- Ultrasound-guided central cluster approach for the supraclavicular brachial plexus block: a case series