J Korean Med Sci.
2022 Jan;37(4):e29. 10.3346/jkms.2022.37.e29.
Clinical Effect of Hepatitis B Virus on COVID-19 Infected Patients: A Nationwide Population-Based Study Using the Health Insurance Review & Assessment Service Database
- Affiliations
-
- 1Department of Internal Medicine, Korea University Ansan Hospital, Ansan, Korea
- 2Health Insurance Review and Assessment Service, Wonju, Korea
- KMID: 2525010
- DOI: http://doi.org/10.3346/jkms.2022.37.e29
Abstract
- Background
Several studies have recently suggested that liver disease and cirrhosis were risk factors for poor outcomes in patients with coronavirus disease 2019 (COVID-19) infections. However, no large data study has reported the clinical course of COVID-19 patients with chronic hepatitis B virus (HBV) infections. This study investigated whether HBV infection had negative impacts on the clinical outcomes of COVID-19 patients.
Methods
We performed a nationwide population-based cohort study with 19,160 COVID-19-infected patients in 2020 from the Korean Health Insurance Review and Assessment database. The clinical outcomes of COVID-19 patients with chronic HBV infections were assessed and compared to those of non-HBV-infected patients.
Results
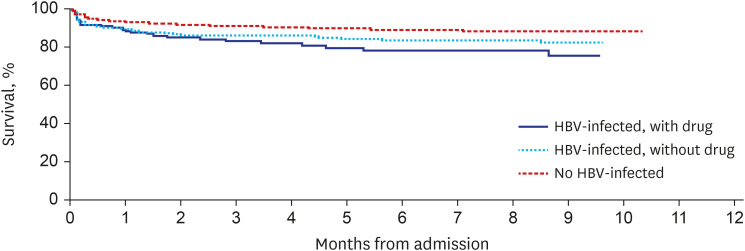
Of the 19,160 patients diagnosed with COVID-19, 675 (3.5%) patients had chronic HBV infections. The HBV-infected patients were older and had more commodities than the non-HBV infected COVID-19 patients. During the observation period, COVID-19-related mortality was seen in 1,524 (8.2%) of the non-HBV-infected 18,485 patients, whereas 91 (13.5%) in HBV-infected 675 patients died of COVID-19 infection. Compared to patients without HBV infections, a higher proportion of patients with chronic HBV infections required intensive care unit (ICU) admission and had organ failures. However, odds ratios for mortality, ICU admission, and organ failure were comparable between the two groups after adjusting for age, sex, and comorbid diseases including liver cirrhosis and hepatocellular carcinoma.
Conclusion
COVID-19-infected patients with HBV infections showed worse clinical courses than non-HBV-infected COVID-19 patients. However, after adjustment, chronic HBV infection itself does not seem to affect the clinical outcomes in COVID-19 patients.
Keyword
Figure
Cited by 1 articles
-
The Health Status and Management of Migrant Workers in Cheonan: A Comparison Study With Korean Citizens
Sungyeon Kim, Dong Jun Lee, Seung Hyeon Kim, Min Su Byun, Young Sun Yun, Nam Kyu Lim
J Korean Med Sci. 2023;38(46):e398. doi: 10.3346/jkms.2023.38.e398.
Reference
-
1. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382(18):1708–1720. PMID: 32109013.
Article2. Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY). 2020; 12(7):6049–6057. PMID: 32267833.
Article3. Lee YR, Kang MK, Song JE, Kim HJ, Kweon YO, Tak WY, et al. Clinical outcomes of coronavirus disease 2019 in patients with pre-existing liver diseases: a multicenter study in South Korea. Clin Mol Hepatol. 2020; 26(4):562–576. PMID: 33053932.
Article4. Moon AM, Webb GJ, Aloman C, Armstrong MJ, Cargill T, Dhanasekaran R, et al. High mortality rates for SARS-CoV-2 infection in patients with pre-existing chronic liver disease and cirrhosis: preliminary results from an international registry. J Hepatol. 2020; 73(3):705–708. PMID: 32446714.5. Xiao Y, Pan H, She Q, Wang F, Chen M. Prevention of SARS-CoV-2 infection in patients with decompensated cirrhosis. Lancet Gastroenterol Hepatol. 2020; 5(6):528–529. PMID: 32197093.
Article6. Cai Q, Huang D, Yu H, Zhu Z, Xia Z, Su Y, et al. COVID-19: abnormal liver function tests. J Hepatol. 2020; 73(3):566–574. PMID: 32298767.
Article7. Piano S, Dalbeni A, Vettore E, Benfaremo D, Mattioli M, Gambino CG, et al. Abnormal liver function tests predict transfer to intensive care unit and death in COVID-19. Liver Int. 2020; 40(10):2394–2406. PMID: 32526083.
Article8. Marjot T, Buescher G, Sebode M, Barnes E, Barritt AS 4th, Armstrong MJ, et al. SARS-CoV-2 infection in patients with autoimmune hepatitis. J Hepatol. 2021; 74(6):1335–1343. PMID: 33508378.
Article9. Kim D, Adeniji N, Latt N, Kumar S, Bloom PP, Aby ES, et al. Predictors of outcomes of COVID-19 in patients with chronic liver disease: US multi-center study. Clin Gastroenterol Hepatol. 2021; 19(7):1469–1479.e19. PMID: 32950749.
Article10. Butt AA, Yan P, Chotani RA, Shaikh OS. Mortality is not increased in SARS-CoV-2 infected persons with hepatitis C virus infection. Liver Int. 2021; 41(8):1824–1831. PMID: 33534931.
Article11. Kang SH, Cho DH, Choi J, Baik SK, Gwon JG, Kim MY. Association between chronic hepatitis B infection and COVID-19 outcomes: a Korean nationwide cohort study. PLoS One. 2021; 16(10):e0258229. PMID: 34610052.
Article12. Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020; 25(3):2000045.
Article13. Jung SY, Choi JC, You SH, Kim WY. Association of renin-angiotensin-aldosterone system inhibitors with coronavirus disease 2019 (COVID-19)- related outcomes in Korea: a nationwide population-based cohort study. Clin Infect Dis. 2020; 71(16):2121–2128. PMID: 32442285.14. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40(5):373–383. PMID: 3558716.
Article15. Chu H, Chan JF, Yuen TT, Shuai H, Yuan S, Wang Y, et al. Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: an observational study. Lancet Microbe. 2020; 1(1):e14–e23. PMID: 32835326.
Article16. Pirola CJ, Sookoian S. SARS-CoV-2 virus and liver expression of host receptors: putative mechanisms of liver involvement in COVID-19. Liver Int. 2020; 40(8):2038–2040. PMID: 32352224.
Article17. Sonzogni A, Previtali G, Seghezzi M, Grazia Alessio M, Gianatti A, Licini L, et al. Liver histopathology in severe COVID 19 respiratory failure is suggestive of vascular alterations. Liver Int. 2020; 40(9):2110–2116. PMID: 32654359.
Article18. Marjot T, Moon AM, Cook JA, Abd-Elsalam S, Aloman C, Armstrong MJ, et al. Outcomes following SARS-CoV-2 infection in patients with chronic liver disease: an international registry study. J Hepatol. 2021; 74(3):567–577. PMID: 33035628.
Article19. Sarin SK, Choudhury A, Lau GK, Zheng MH, Ji D, Abd-Elsalam S, et al. Pre-existing liver disease is associated with poor outcome in patients with SARS CoV2 infection; The APCOLIS Study (APASL COVID-19 Liver Injury Spectrum Study). Hepatol Int. 2020; 14(5):690–700. PMID: 32623632.
Article20. Ashburn TT, Thor KB. Drug repositioning: identifying and developing new uses for existing drugs. Nat Rev Drug Discov. 2004; 3(8):673–683. PMID: 15286734.
Article21. Malik S, Gupta A, Zhong X, Rasmussen TP, Manautou JE, Bahal R. Emerging therapeutic modalities against COVID-19. Pharmaceuticals (Basel). 2020; 13(8):188.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- COVID-19 International Collaborative Research by the Health Insurance Review and Assessment Service Using Its Nationwide Real-world Data: Database, Outcomes, and Implications
- Incidence and Treatment Pattern of Extremity Soft Tissue Sarcoma in Korea, 2009-2011: A Nationwide Study Based on the Health Insurance Review and Assessment Service Database
- The impact of the COVID-19 pandemic on clinical practices related to colorectal cancer and colonoscopy in South Korea: a nationwide population-based study
- A Nationwide Study on the Impact of COVID-19 Pandemic on Volume of Spine Surgery in South Korea
- Changes in Expenditures of the National Health Insurance of Korea during the COVID-19 Pandemic and the Financial Implications Thereof