Anesth Pain Med.
2021 Oct;16(4):344-352. 10.17085/apm.21028.
Preoperative 2D-echocardiographic assessment of pulmonary arterial pressure in subgroups of liver transplantation recipients
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Medicine, Dongtan Sacred Heart Hospital, Hallym University School of Medicine, Hwaseong, Korea
- 3Department of Medicine, Heart, Stroke, and Vascular Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 5Department of Anesthesiology, School of Dentistry, Dankook University, Cheonan, Korea
- KMID: 2524446
- DOI: http://doi.org/10.17085/apm.21028
Abstract
- Background
The clinical efficacy of preoperative 2D-echocardiographic assessment of pulmonary arterial pressure (PAP) has not been evaluated fully in liver transplantation (LT) recipients.
Methods
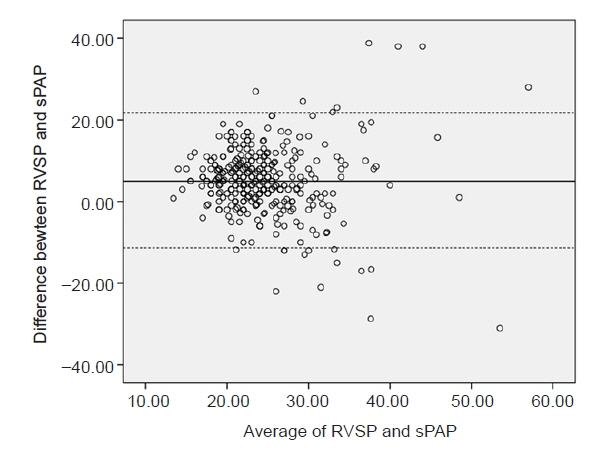
From October 2010 to February 2017, a total of 344 LT recipients who underwent preoperative 2D-echocardiography and intraoperative right heart catheterization (RHC) was enrolled and stratified according to etiology, disease progression, and clinical setting. The correlation of right ventricular systolic pressure (RVSP) on preoperative 2D-echocardiography with mean and systolic PAP on intraoperative RHC was evaluated, and the predictive value of RVSP > 50 mmHg to identify mean PAP > 35 mmHg was estimated.
Results
In the overall population, significant but weak correlations were observed (R = 0.27; P < 0.001 for systolic PAP, R = 0.24; P < 0.001 for mean PAP). The positive and negative predictive values of RVSP > 50 mmHg identifying mean PAP > 35 mmHg were 37.5% and 49.9%, respectively. In the subgroup analyses, correlations were not significant in recipients of deceased donor type LT (R = 0.129; P = 0.224 for systolic PAP, R = 0.163; P = 0.126 for mean PAP) or in recipients with poorly controlled ascites (R = 0.215; P = 0.072 for systolic PAP, R = 0.21; P = 0.079 for mean PAP).
Conclusion
In LT recipients, the correlation between RVSP on preoperative 2D-echocardiography and PAP on intraoperative RHC was weak; thus, preoperative 2D-echocardiography might not be the optimal tool for predicting intraoperative PAP. In LT candidates at risk of pulmonary hypertension, RHC should be considered.
Figure
Reference
-
1. Salgia RJ, Goodrich NP, Simpson H, Merion RM, Sharma P. Outcomes of liver transplantation for porto-pulmonary hypertension in model for end-stage liver disease era. Dig Dis Sci. 2014; 59:1976–82.2. Houlihan DD, Holt A, Elliot C, Ferguson JW. Review article: liver transplantation for the pulmonary disorders of portal hypertension. Aliment Pharmacol Ther. 2013; 37:183–94.3. Krowka MJ, Fallon MB, Kawut SM, Fuhrmann V, Heimbach JK, Ramsay MA, et al. International Liver Transplant Society Practice Guidelines: diagnosis and management of Hepatopulmonary syndrome and Portopulmonary hypertension. Transplantation. 2016; 100:1440–52.4. Krowka MJ, Plevak DJ, Findlay JY, Rosen CB, Wiesner RH, Krom RA. Pulmonary hemodynamics and perioperative cardiopulmonary-related mortality in patients with portopulmonary hypertension undergoing liver transplantation. Liver Transpl. 2000; 6:443–50.5. Gwak MS, Kim JA, Kim GS, Choi SJ, Ahn H, Lee JJ, et al. Incidence of severe ventricular arrhythmias during pulmonary artery catheterization in liver allograft recipients. Liver Transpl. 2007; 13:1451–4.6. Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J. 2015; 46:903–75.7. Janda S, Shahidi N, Gin K, Swiston J. Diagnostic accuracy of echocardiography for pulmonary hypertension: a systematic review and meta-analysis. Heart. 2011; 97:612–22.8. Kim WR, Krowka MJ, Plevak DJ, Lee J, Rettke SR, Frantz RP, et al. Accuracy of Doppler echocardiography in the assessment of pulmonary hypertension in liver transplant candidates. Liver Transpl. 2000; 6:453–8.9. Cotton CL, Gandhi S, Vaitkus PT, Massad MG, Benedetti E, Mrtek RG, et al. Role of echocardiography in detecting portopulmonary hypertension in liver transplant candidates. Liver Transpl. 2002; 8:1051–4.10. Sussman N, Kaza V, Barshes N, Stribling R, Goss J, O'Mahony C, et al. Successful liver transplantation following medical management of portopulmonary hypertension: a single-center series. Am J Transplant. 2006; 6:2177–82.11. Ashfaq M, Chinnakotla S, Rogers L, Ausloos K, Saadeh S, Klintmalm GB, et al. The impact of treatment of portopulmonary hypertension on survival following liver transplantation. Am J Transplant. 2007; 7:1258–64.12. Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23:685–713; quiz 786-8.13. Krowka MJ, Mandell MS, Ramsay MA, Kawut SM, Fallon MB, Manzarbeitia C, et al. Hepatopulmonary syndrome and portopulmonary hypertension: a report of the multicenter liver transplant database. Liver Transpl. 2004; 10:174–82.14. Kia L, Shah SJ, Wang E, Sharma D, Selvaraj S, Medina C, et al. Role of pretransplant echocardiographic evaluation in predicting outcomes following liver transplantation. Am J Transplant. 2013; 13:2395–401.15. Bushyhead D, Kirkpatrick JN, Goldberg D. Pretransplant echocardiographic parameters as markers of posttransplant outcomes in liver transplant recipients. Liver Transpl. 2016; 22:316–23.16. Raevens S, Colle I, Reyntjens K, Geerts A, Berrevoet F, Rogiers X, et al. Echocardiography for the detection of portopulmonary hypertension in liver transplant candidates: an analysis of cutoff values. Liver Transpl. 2013; 19:602–10.17. Milan A, Magnino C, Veglio F. Echocardiographic indexes for the non-invasive evaluation of pulmonary hemodynamics. J Am Soc Echocardiogr. 2010; 23:225–39; quiz 332-4.18. Hemnes AR, Forfia PR, Champion HC. Assessment of pulmonary vasculature and right heart by invasive haemodynamics and echocardiography. Int J Clin Pract Suppl. 2009; (162):4–19.19. Posteraro A, Salustri A, Trambaiolo P, Amici E, Gambelli G. Echocardiographic estimation of pulmonary pressures. J Cardiovasc Med (Hagerstown). 2006; 7:545–54.20. Jeon DS, Luo H, Iwami T, Miyamoto T, Brasch AV, Mirocha J, et al. The usefulness of a 10% air-10% blood-80% saline mixture for contrast echocardiography: Doppler measurement of pulmonary artery systolic pressure. J Am Coll Cardiol. 2002; 39:124–9.21. Waggoner AD, Barzilai B, Pérez JE. Saline contrast enhancement of tricuspid regurgitant jets detected by Doppler color flow imaging. Am J Cardiol. 1990; 65:1368–71.22. Fischer LG, Aken HV, Bu Combining Diaeresis Rkle H. Management of pulmonary hypertension: physiological and pharmacological considerations for anesthesiologists. Anesth Analg. 2003; 96:1603–16.23. Goodkin GM, Spevack DM, Tunick PA, Kronzon I. How useful is hand-carried bedside echocardiography in critically ill patients? J Am Coll Cardiol. 2001; 37:2019–22.24. Ling LF, Obuchowski NA, Rodriguez L, Popovic Z, Kwon D, Marwick TH. Accuracy and interobserver concordance of echocardiographic assessment of right ventricular size and systolic function: a quality control exercise. J Am Soc Echocardiogr. 2012; 25:709–13.25. Dagar G, Taneja A, Nanchal RS. Abdominal circulatory interactions. Crit Care Clin. 2016; 32:265–77.26. Wexler L, Bergel DH, Gabe IT, Makin GS, Mills CJ. Velocity of blood flow in normal human venae cavae. Circ Res. 1968; 23:349–59.27. Takata M, Wise RA, Robotham JL. Effects of abdominal pressure on venous return: abdominal vascular zone conditions. J Appl Physiol (1985). 1990; 69:1961–72.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship of preoperative echocardiography and circulation in living donor liver transplantation
- A Study on the Echocardiographic Right Ventricular Systolic Time Intervals in Adults
- Comparatives Study of Pulmonary Artery and Pulmonary Venous Wedge Pressure in Congenital Heart Disease
- Noninvasive estimation of raised intracranial pressure using ocular ultrasonography in liver transplant recipients with acute liver failure: A report of two cases
- Prediction of Pulmonary Arterial Pressure by Pulsed Doppler Echocardiography