Acute Crit Care.
2021 Nov;36(4):380-387. 10.4266/acc.2020.01193.
Prognostic factors of pediatric hematopoietic stem cell transplantation recipients admitted to the pediatric intensive care unit
- Affiliations
-
- 1Department of Pediatrics, Asan Medical Center Children’s Hospital, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2524322
- DOI: http://doi.org/10.4266/acc.2020.01193
Abstract
- Background
Pediatric patients who received hematopoietic stem cell transplantation (HSCT) tend to have high morbidity and mortality. While, the prognostic factors of adult patients received bone marrow transplantation were already known, there is little known in pediatric pateints. This study aimed to identify the prognostic factor for pediatric intensive care unit (PICU) mortality of critically ill pediatric patients with HSCT. Method: Retrospectively reviewed that the medical records of patients who received HSCT and admitted to PICU between January 2010 and December 2019. Mortality was defined a patient who expired within 28 days.
Results
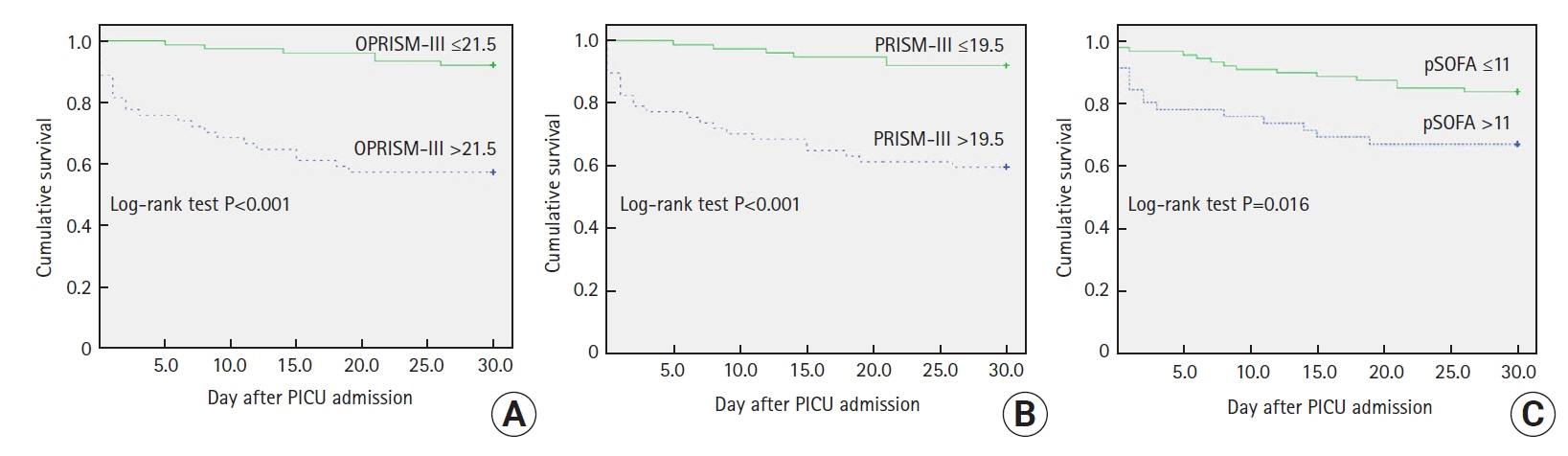
A total of 131 patients were included. There were 63 boys (48.1%) and median age was 11 years (interquartile range, 0–20 years). The most common HSCT type was haploidentical (38.9%) and respiratory failure (44.3%) was the most common reason for PICU admission. Twenty-eight–day mortality was 22.1% (29/131). In comparison between survivors and non-survivors, the number of HSCT received, sepsis, oncological pediatric risk of mortality-III (OPRISM-III), PRISM-III, pediatric sequential organ failure assessment (pSOFA), serum lactate, B-type natriuretic peptide (BNP) and use of mechanical ventilator (MV) and vasoactive inotropics were significant predictors (p<0.05 for all variables). In multivariate logistic regression, number of HSCT received, use of MV, OPRISM-III, PRISM-III and pSOFA were independent risk factors of PICU mortality. Moreover, three scoring systems were significant prognostic factors of 28-day mortality.
Conclusions
The number of HSCT received and use of MV were more accurate predictors in pediatric patients received HSCT.
Keyword
Figure
Reference
-
1. Savaşan S, Abella EM. Current issues in pediatric stem cell transplantation. Clin Lab Med. 2005; 25:519–40.
Article2. Gratwohl A, Baldomero H, Aljurf M, Pasquini MC, Bouzas LF, Yoshimi A, et al. Hematopoietic stem cell transplantation: a global perspective. JAMA. 2010; 303:1617–24.3. Appelbaum FR. Hematopoietic-cell transplantation at 50. N Engl J Med. 2007; 357:1472–5.
Article4. Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006; 354:1813–26.
Article5. Oudin C, Chevallier P, Furst S, Guillaume T, El Cheikh J, Delaunay J, et al. Reduced-toxicity conditioning prior to allogeneic stem cell transplantation improves outcome in patients with myeloid malignancies. Haematologica. 2014; 99:1762–8.
Article6. Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009; 15:1628–33.
Article7. Passweg JR, Baldomero H, Peters C, Gaspar HB, Cesaro S, Dreger P, et al. Hematopoietic SCT in Europe: data and trends in 2012 with special consideration of pediatric transplantation. Bone Marrow Transplant. 2014; 49:744–50.
Article8. Gooley TA, Chien JW, Pergam SA, Hingorani S, Sorror ML, Boeckh M, et al. Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med. 2010; 363:2091–101.
Article9. Azoulay E, Afessa B. The intensive care support of patients with malignancy: do everything that can be done. Intensive Care Med. 2006; 32:3–5.
Article10. Pène F, Aubron C, Azoulay E, Blot F, Thiéry G, Raynard B, et al. Outcome of critically ill allogeneic hematopoietic stem-cell transplantation recipients: a reappraisal of indications for organ failure supports. J Clin Oncol. 2006; 24:643–9.
Article11. Platon L, Amigues L, Ceballos P, Fegueux N, Daubin D, Besnard N, et al. A reappraisal of ICU and long-term outcome of allogeneic hematopoietic stem cell transplantation patients and reassessment of prognosis factors: results of a 5-year cohort study (2009-2013). Bone Marrow Transplant. 2016; 51:256–61.
Article12. Benz R, Schanz U, Maggiorini M, Seebach JD, Stussi G. Risk factors for ICU admission and ICU survival after allogeneic hematopoietic SCT. Bone Marrow Transplant. 2014; 49:62–5.
Article13. Saillard C, Blaise D, Mokart D. Critically ill allogeneic hematopoietic stem cell transplantation patients in the intensive care unit: reappraisal of actual prognosis. Bone Marrow Transplant. 2016; 51:1050–61.
Article14. Saillard C, Darmon M, Bisbal M, Sannini A, Chow-Chine L, Faucher M, et al. Critically ill allogenic HSCT patients in the intensive care unit: a systematic review and meta-analysis of prognostic factors of mortality. Bone Marrow Transplant. 2018; 53:1233–41.
Article15. Pollack MM, Patel KM, Ruttimann UE. PRISM III: an updated pediatric risk of mortality score. Crit Care Med. 1996; 24:743–52.16. Matics TJ, Sanchez-Pinto LN. Adaptation and validation of a pediatric sequential organ failure assessment score and evaluation of the sepsis-3 definitions in critically ill children. JAMA Pediatr. 2017; 171:e172352.
Article17. Schneider DT, Lemburg P, Sprock I, Heying R, Göbel U, Nürnberger W. Introduction of the oncological pediatric risk of mortality score (O-PRISM) for ICU support following stem cell transplantation in children. Bone Marrow Transplant. 2000; 25:1079–86.
Article18. Soubani AO, Kseibi E, Bander JJ, Klein JL, Khanchandani G, Ahmed HP, et al. Outcome and prognostic factors of hematopoietic stem cell transplantation recipients admitted to a medical ICU. Chest. 2004; 126:1604–11.
Article19. Jacobe SJ, Hassan A, Veys P, Mok Q. Outcome of children requiring admission to an intensive care unit after bone marrow transplantation. Crit Care Med. 2003; 31:1299–305.
Article20. Keenan HT, Bratton SL, Martin LD, Crawford SW, Weiss NS. Outcome of children who require mechanical ventilatory support after bone marrow transplantation. Crit Care Med. 2000; 28:830–5.
Article21. Mokart D, Granata A, Crocchiolo R, Sannini A, Chow-Chine L, Brun JP, et al. Allogeneic hematopoietic stem cell transplantation after reduced intensity conditioning regimen: outcomes of patients admitted to intensive care unit. J Crit Care. 2015; 30:1107–13.
Article22. Choi HS, Lee EJ, Lee JW, Jang PS, Chung NG, Cho B, et al. Prediction of Prognosis for children cared in intensive care unit (ICU) after hematopoietic stem cell transplantation (HSCT). Korean J Crit Care Med. 2011; 26:226–31.
Article23. González-Vicent M, Marín C, Madero L, Sevilla J, Díaz MA. Risk score for pediatric intensive care unit admission in children undergoing hematopoietic stem cell transplantation and analysis of predictive factors for survival. J Pediatr Hematol Oncol. 2005; 27:526–31.
Article24. Cheuk DK, Ha SY, Lee SL, Chan GC, Tsoi NS, Lau YL. Prognostic factors in children requiring admission to an intensive care unit after hematopoietic stem cell transplant. Hematol Oncol. 2004; 22:1–9.
Article25. Tomaske M, Bosk A, Eyrich M, Bader P, Niethammer D. Risks of mortality in children admitted to the paediatric intensive care unit after haematopoietic stem cell transplantation. Br J Haematol. 2003; 121:886–91.
Article26. Zinter MS, Logan BR, Fretham C, Sapru A, Abraham A, Aljurf MD, et al. Comprehensive prognostication in critically ill pediatric hematopoietic cell transplant patients: results from merging the center for international blood and marrow transplant research (CIBMTR) and virtual pediatric systems (VPS) registries. Biol Blood Marrow Transplant. 2020; 26:333–42.
Article27. Lamas A, Otheo E, Ros P, Vázquez JL, Maldonado MS, Muñoz A, et al. Prognosis of child recipients of hematopoietic stem cell transplantation requiring intensive care. Intensive Care Med. 2003; 29:91–6.
Article28. Kwon R, Koutsogiannaki S, Staffa SJ, Yuki K. The outcomes of pediatric hematopoietic stem cell transplantation recipients requiring intensive care unit admission: a single center experience. Transl Perioper Pain Med. 2019; 6:75–80.
Article29. Kumar G, Ahmad S, Taneja A, Patel J, Guddati AK, Nanchal R. Milwaukee initiative in critical care outcomes research group of investigators: severe sepsis in hematopoietic stem cell transplant recipients. Transl Perioper Pain Med. 2019; 6:75–80.30. Fernández-García M, Gonzalez-Vicent M, Mastro-Martinez I, Serrano A, Diaz MA. Intensive care unit admissions among children after hematopoietic stem cell transplantation: incidence, outcome, and prognostic factors. J Pediatr Hematol Oncol. 2015; 37:529–35.31. Schneider DT, Cho J, Laws HJ, Dilloo D, Göbel U, Nürnberger W. Serial evaluation of the oncological pediatric risk of mortality (O-PRISM) score following allogeneic bone marrow transplantation in children. Bone Marrow Transplant. 2002; 29:383–9.
Article32. Torrecilla C, Cortés JL, Chamorro C, Rubio JJ, Galdos P, Dominguez de Villota E. Prognostic assessment of the acute complications of bone marrow transplantation requiring intensive therapy. Intensive Care Med. 1988; 14:393–8.
Article33. Staudinger T, Stoiser B, Müllner M, Locker GJ, Laczika K, Knapp S, et al. Outcome and prognostic factors in critically ill cancer patients admitted to the intensive care unit. Crit Care Med. 2000; 28:1322–8.
Article34. Pène F, Percheron S, Lemiale V, Viallon V, Claessens YE, Marqué S, et al. Temporal changes in management and outcome of septic shock in patients with malignancies in the intensive care unit. Crit Care Med. 2008; 36:690–6.
Article35. Zuber B, Tran TC, Aegerter P, Grimaldi D, Charpentier J, Guidet B, et al. Impact of case volume on survival of septic shock in patients with malignancies. Crit Care Med. 2012; 40:55–62.
Article36. McGowan JV, Chung R, Maulik A, Piotrowska I, Walker JM, Yellon DM. Anthracycline chemotherapy and cardiotoxicity. Cardiovasc Drugs Ther. 2017; 31:63–75.
Article37. Dhesi S, Chu MP, Blevins G, Paterson I, Larratt L, Oudit GY, et al. Cyclophosphamide-induced cardiomyopathy: a case report, review, and recommendations for management. J Investig Med High Impact Case Rep. 2013; 1:2324709613480346.38. Snowden JA, Hill GR, Hunt P, Carnoutsos S, Spearing RL, Espiner E, et al. Assessment of cardiotoxicity during haemopoietic stem cell transplantation with plasma brain natriuretic peptide. Bone Marrow Transplant. 2000; 26:309–13.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcome and risk factors of pediatric hemato-oncology patients admitted in pediatric intensive care unit
- Comparison of Quality of Life of Autologous and Allogeneic Hematopoietic Stem Cell Transplantation Recipients
- Hematopoietic Stem Cell Transplantation in Inborn Error of Metabolism
- Prediction of Prognosis for Children Cared in Intensive Care Unit (ICU) after Hematopoietic Stem Cell Transplantation (HSCT)
- Gastrointestinal Complications Following Hematopoietic Stem Cell Transplantation in Children