Prog Med Phys.
2021 Dec;32(4):172-178. 10.14316/pmp.2021.32.4.172.
Synthetic Computed Tomography Generation while Preserving Metallic Markers for Three-Dimensional Intracavitary Radiotherapy: Preliminary Study
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea
- 2Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea
- KMID: 2524165
- DOI: http://doi.org/10.14316/pmp.2021.32.4.172
Abstract
- Purpose
This study aimed to develop a deep learning architecture combining two task models to generate synthetic computed tomography (sCT) images from low-tesla magnetic resonance (MR) images to improve metallic marker visibility.
Methods
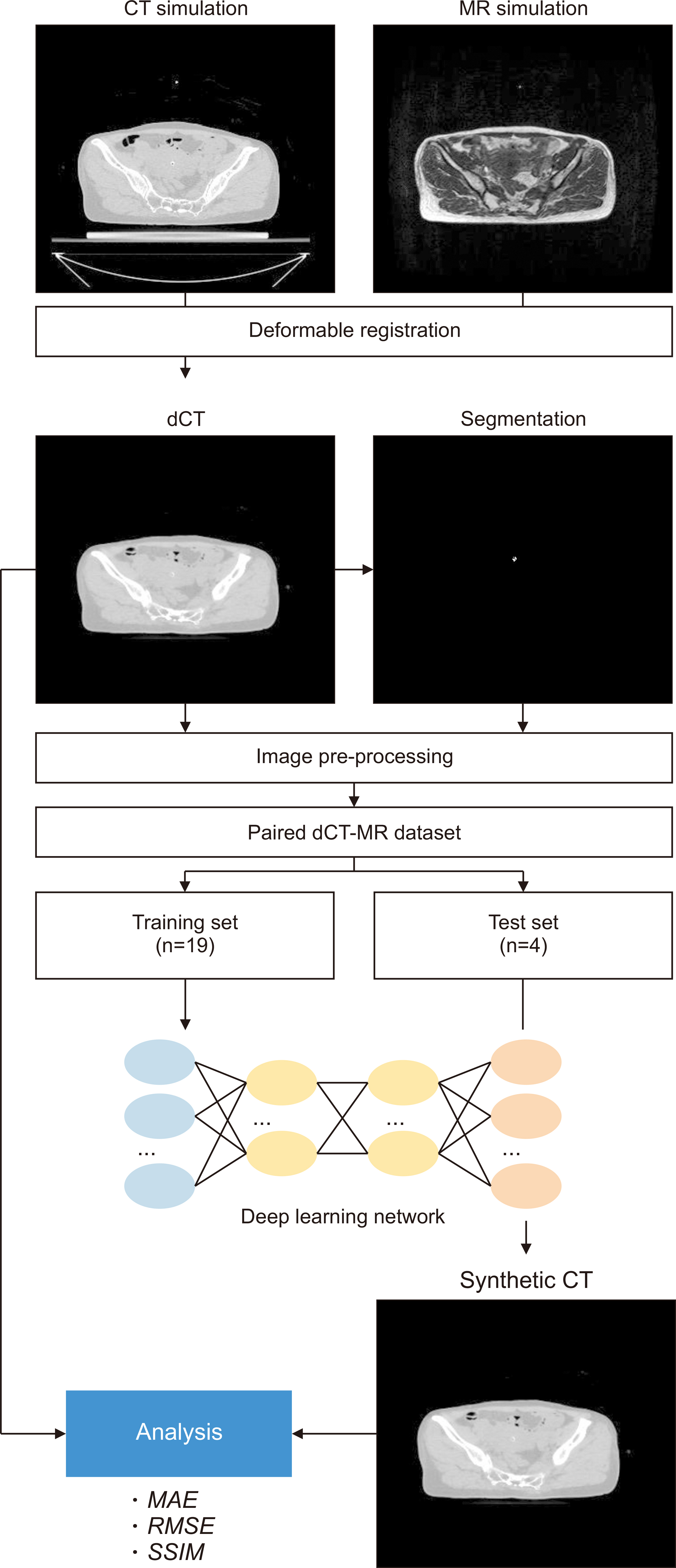
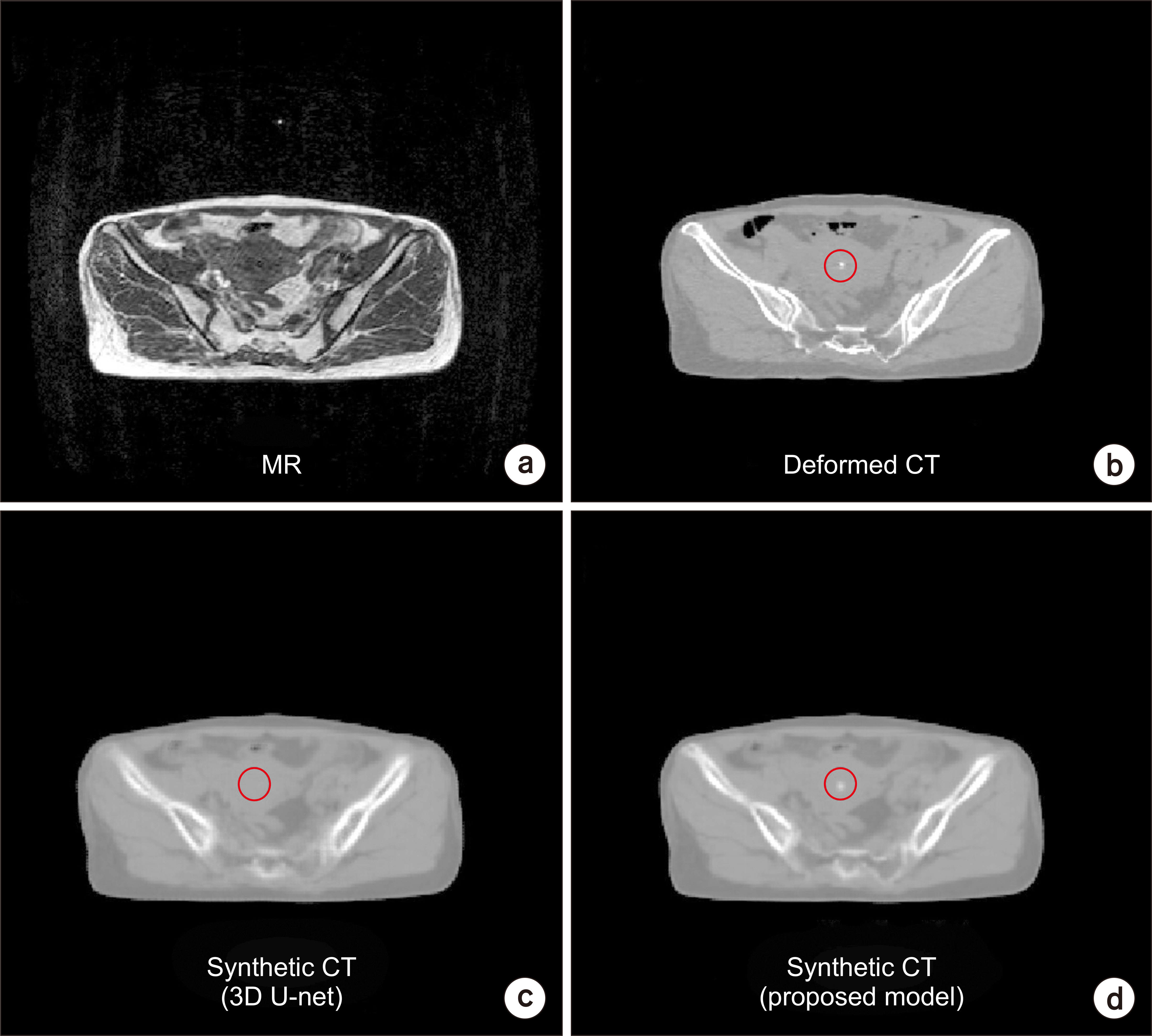
Twenty-three patients with cervical cancer treated with intracavitary radiotherapy (ICR) were retrospectively enrolled, and images were acquired using both a computed tomography (CT) scanner and a low-tesla MR machine. The CT images were aligned to the corresponding MR images using a deformable registration, and the metallic dummy source markers were delineated using threshold-based segmentation followed by manual modification. The deformed CT (dCT), MR, and segmentation mask pairs were used for training and testing. The sCT generation model has a cascaded three-dimensional (3D) U-Net-based architecture that converts MR images to CT images and segments the metallic marker. The performance of the model was evaluated with intensity-based comparison metrics.
Results
The proposed model with segmentation loss outperformed the 3D U-Net in terms of errors between the sCT and dCT. The structural similarity score difference was not significant.
Conclusions
Our study shows the two-task-based deep learning models for generating the sCT images using low-tesla MR images for 3D ICR. This approach will be useful to the MR-only workflow in high-dose-rate brachytherapy.
Keyword
Figure
Reference
-
References
1. Chargari C, Magné N, Dumas I, Messai T, Vicenzi L, Gillion N, et al. 2009; Physics contributions and clinical outcome with 3D-MRI-based pulsed-dose-rate intracavitary brachytherapy in cervical cancer patients. Int J Radiat Oncol Biol Phys. 74:133–139. DOI: 10.1016/j.ijrobp.2008.06.1912. PMID: 18774656.
Article2. Tanderup K, Eifel PJ, Yashar CM, Pötter R, Grigsby PW. 2014; Curative radiation therapy for locally advanced cervical cancer: brachytherapy is NOT optional. Int J Radiat Oncol Biol Phys. 88:537–539. DOI: 10.1016/j.ijrobp.2013.11.011. PMID: 24411631.
Article3. Chassagne D, Dutreix A, Almond P, Burgers J, Busch M, Joslin C. 1985; International Commission on Radiological Units and Measurements Report No. 38: dose and volume specification for reporting intracavitary therapy in gynecology. J ICRU. 20:DOI: 10.1093/jicru/os20.1.Report38.4. Kang HC, Shin KH, Park SY, Kim JY. 2010; 3D CT-based high-dose-rate brachytherapy for cervical cancer: clinical impact on late rectal bleeding and local control. Radiother Oncol. 97:507–513. DOI: 10.1016/j.radonc.2010.10.002. PMID: 21074881.
Article5. Pötter R, Haie-Meder C, Van Limbergen E, Barillot I, De Brabandere M, Dimopoulos J, et al. 2006; Recommendations from gynaecological (GYN) GEC ESTRO working group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother Oncol. 78:67–77. DOI: 10.1016/j.radonc.2005.11.014. PMID: 16403584.
Article6. Haie-Meder C, Pötter R, Van Limbergen E, Briot E, De Brabandere M, Dimopoulos J, et al. 2005; Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 74:235–245. DOI: 10.1016/j.radonc.2004.12.015. PMID: 15763303.
Article7. Tanderup K, Viswanathan AN, Kirisits C, Frank SJ. 2014; Magnetic resonance image guided brachytherapy. Semin Radiat Oncol. 24:181–191. DOI: 10.1016/j.semradonc.2014.02.007. PMID: 24931089. PMCID: PMC4147854.
Article8. Owrangi AM, Prisciandaro JI, Soliman A, Ravi A, Song WY. 2015; Magnetic resonance imaging-guided brachytherapy for cervical cancer: initiating a program. J Contemp Brachytherapy. 7:417–422. DOI: 10.5114/jcb.2015.55541. PMID: 26622249. PMCID: PMC4663219.9. Hellebust TP, Kirisits C, Berger D, Pérez-Calatayud J, De Brabandere M, De Leeuw A, et al. 2010; Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group: considerations and pitfalls in commissioning and applicator reconstruction in 3D image-based treatment planning of cervix cancer brachytherapy. Radiother Oncol. 96:153–160. DOI: 10.1016/j.radonc.2010.06.004. PMID: 20663578.
Article10. Haack S, Nielsen SK, Lindegaard JC, Gelineck J, Tanderup K. 2009; Applicator reconstruction in MRI 3D image-based dose planning of brachytherapy for cervical cancer. Radiother Oncol. 91:187–193. DOI: 10.1016/j.radonc.2008.09.002. PMID: 18977049.
Article11. Shaaer A, Paudel M, Smith M, Tonolete F, Nicolae A, Leung E, et al. 2020; Evaluation of an MR-only interstitial gynecologic brachytherapy workflow using MR-line marker for catheter reconstruction. Brachytherapy. 19:642–650. DOI: 10.1016/j.brachy.2020.06.007. PMID: 32712027.
Article12. Ning MS, Vedam S, Ma J, Stafford RJ, Bruno TL, Cunningham M, et al. 2020; Clinical utility and value contribution of an MRI-positive line marker for image-guided brachytherapy in gynecologic malignancies. Brachytherapy. 19:305–315. DOI: 10.1016/j.brachy.2019.12.005. PMID: 32265119.
Article13. Kim JH, Jung S, Kim JI. 2019; Low magnetic field MRI visibility of rubber-based markers. Prog Med Phys. 30:89–93. DOI: 10.14316/pmp.2019.30.4.89.
Article14. Fu J, Yang Y, Singhrao K, Ruan D, Chu FI, Low DA, et al. 2019; Deep learning approaches using 2D and 3D convolutional neural networks for generating male pelvic synthetic computed tomography from magnetic resonance imaging. Med Phys. 46:3788–3798. DOI: 10.1002/mp.13672. PMID: 31220353.
Article15. Han X. 2017; MR-based synthetic CT generation using a deep convolutional neural network method. Med Phys. 44:1408–1419. DOI: 10.1002/mp.12155. PMID: 28192624.
Article16. Kang SK, An HJ, Jin H, Kim JI, Chie EK, Park JM, et al. 2021; Synthetic CT generation from weakly paired MR images using cycle-consistent GAN for MR-guided radiotherapy. Biomed Eng Lett. 11:263–271. DOI: 10.1007/s13534-021-00195-8. PMID: 34350052.
Article17. Kazemifar S, Nguyen D, Mcguire S, Timmerman R, Nedzi L, Wardak Z, et al. 2018; Synthetic CT generation for MRI-only radiation therapy using deep learning. Med Phys. 45:E700.18. Lei Y, Harms J, Wang T, Liu Y, Shu HK, Jani AB, et al. 2019; MRI-only based synthetic CT generation using dense cycle consistent generative adversarial networks. Med Phys. 46:3565–3581. DOI: 10.1002/mp.13617. PMID: 31112304. PMCID: PMC6692192.
Article19. Rivard MJ, Coursey BM, DeWerd LA, Hanson WF, Huq MS, Ibbott GS, et al. 2004; Update of AAPM Task Group No. 43 report: a revised AAPM protocol for brachytherapy dose calculations. Med Phys. 31:633–674. DOI: 10.1118/1.1646040. PMID: 15070264.
Article20. Beaulieu L, Carlsson Tedgren A, Carrier JF, Davis SD, Mourtada F, Rivard MJ, et al. 2012; Report of the Task Group 186 on model-based dose calculation methods in brachytherapy beyond the TG-43 formalism: current status and recommendations for clinical implementation. Med Phys. 39:6208–6236. DOI: 10.1118/1.4747264. PMID: 23039658.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical outcome after high dose rate intracavitary brachytherapy with traditional point ‘A’ dose prescription in locally advanced carcinoma of uterine cervix: dosimetric analysis from the perspective of computed tomography imaging-based 3-dimensional treatment planning
- Dosimetric Evaluation of Synthetic Computed Tomography Technique on Position Variation of Air Cavity in Magnetic Resonance-Guided Radiotherapy
- Three-dimensional imaging modalities in endodontics
- Assessment of metal artifacts in three-dimensional dental surface models derived by cone-beam computed tomography
- Accuracy of Dose Estimation in High Dose Rate Intracavitary Radiotherapy of Carcinoma of the Uterine Cervix