Prog Med Phys.
2021 Dec;32(4):122-129. 10.14316/pmp.2021.32.4.122.
Design of Multipurpose Phantom for External Audit on Radiotherapy
- Affiliations
-
- 1Department of Radiation Oncology, Kosin University College of Medicine, Busan, Korea
- KMID: 2524158
- DOI: http://doi.org/10.14316/pmp.2021.32.4.122
Abstract
- Purpose
This study aimed to design a multipurpose dose verification phantom for external audits to secure safe and optimal radiation therapy.
Methods
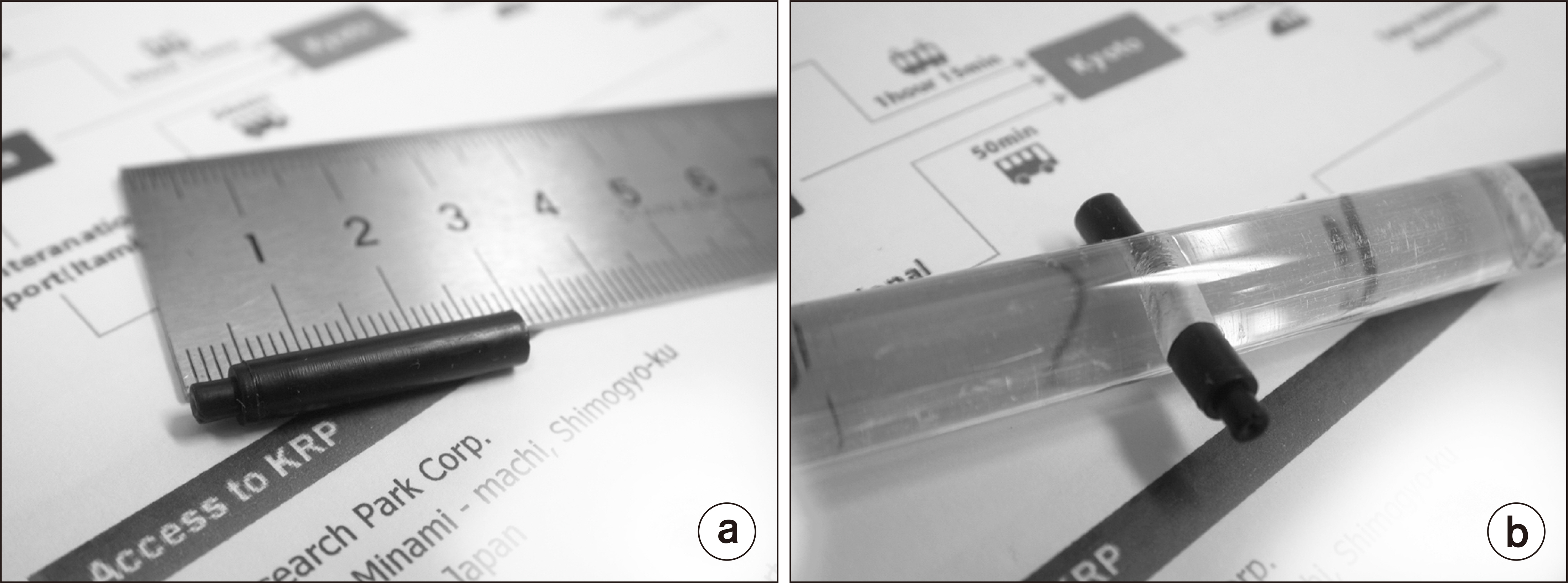
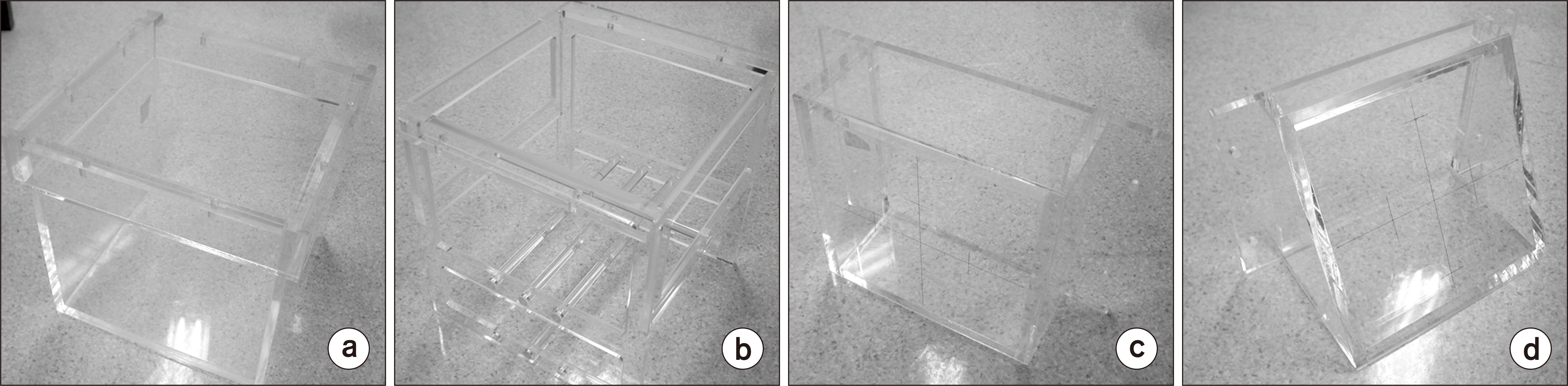
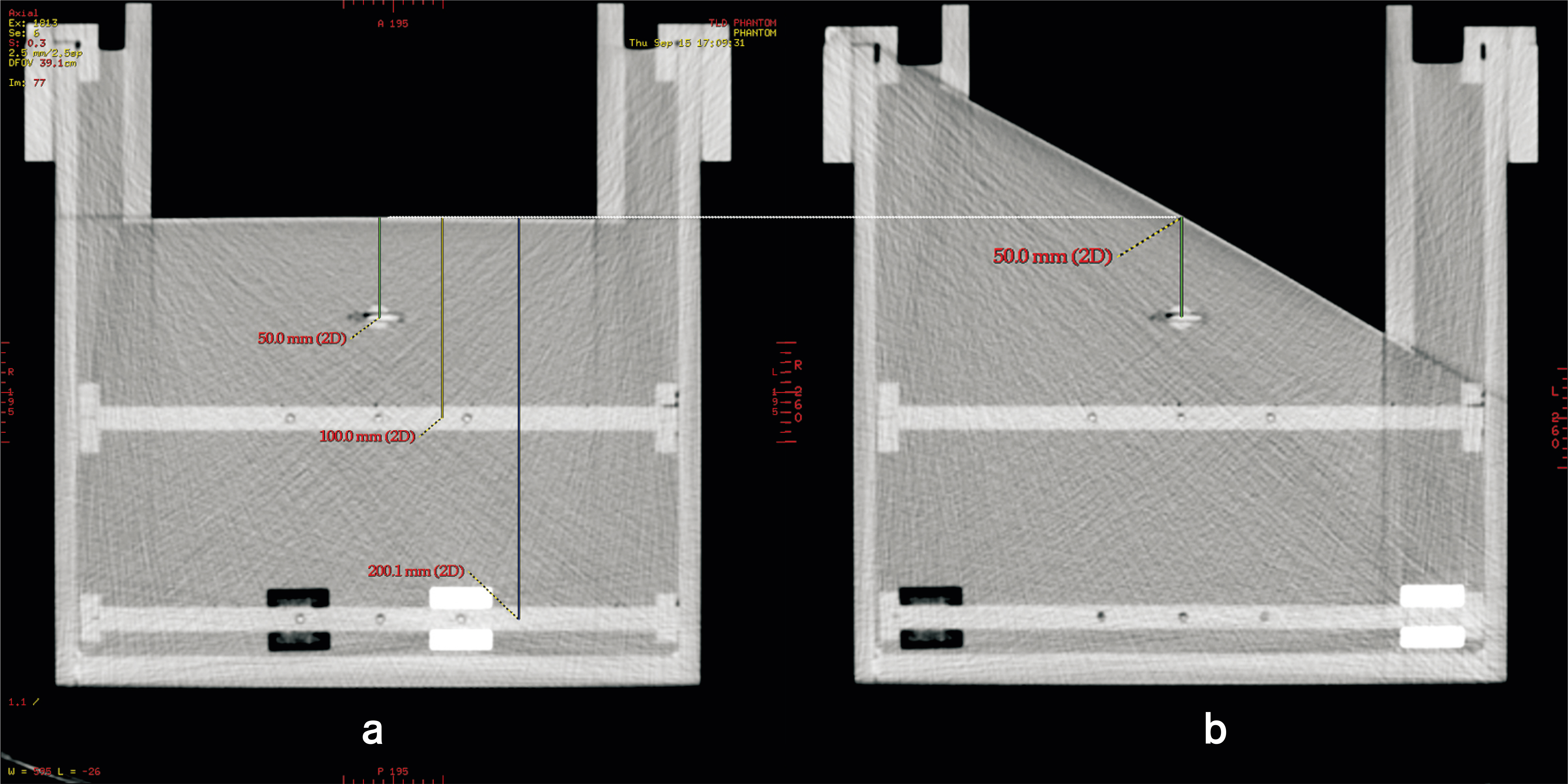
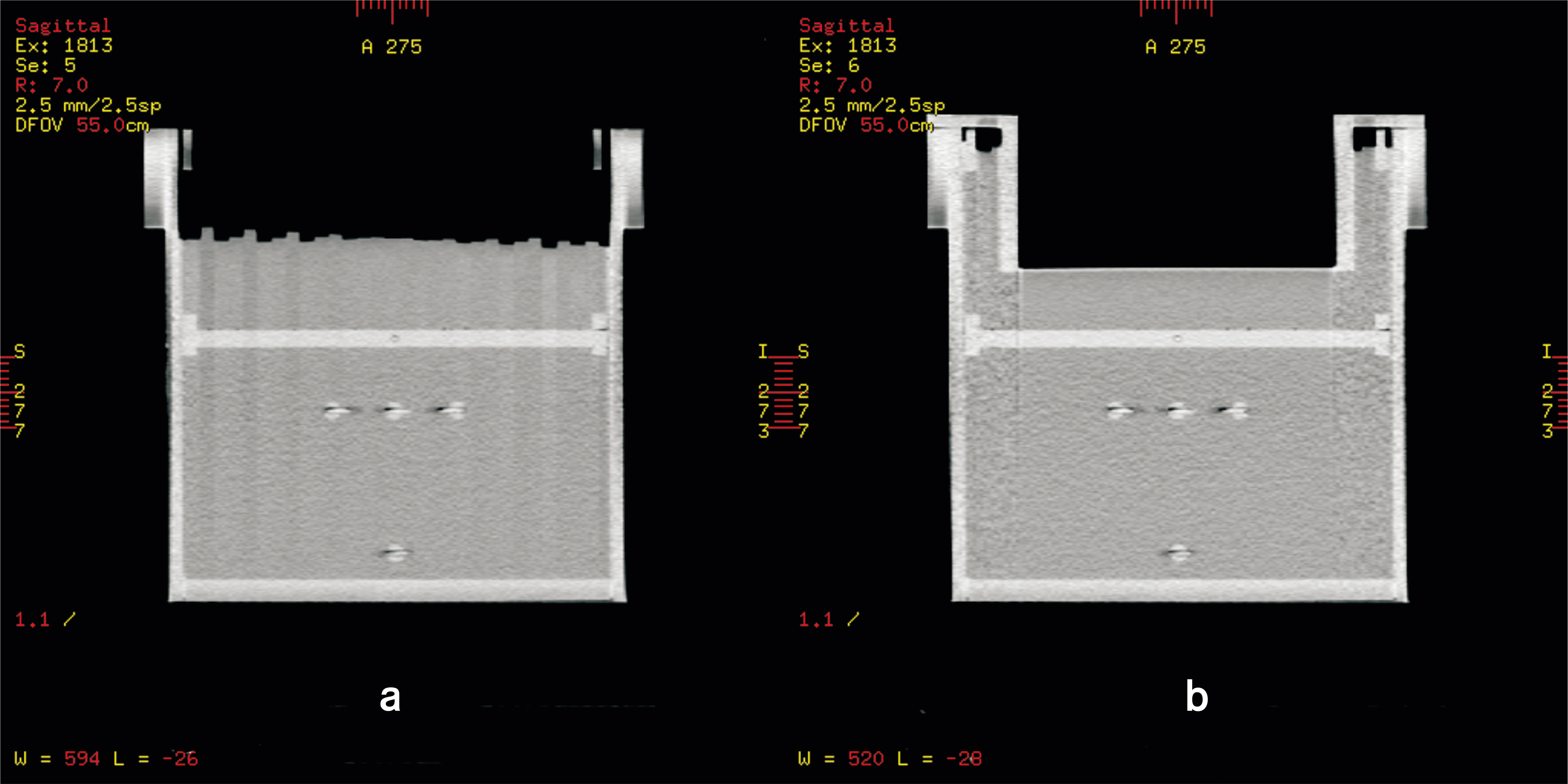
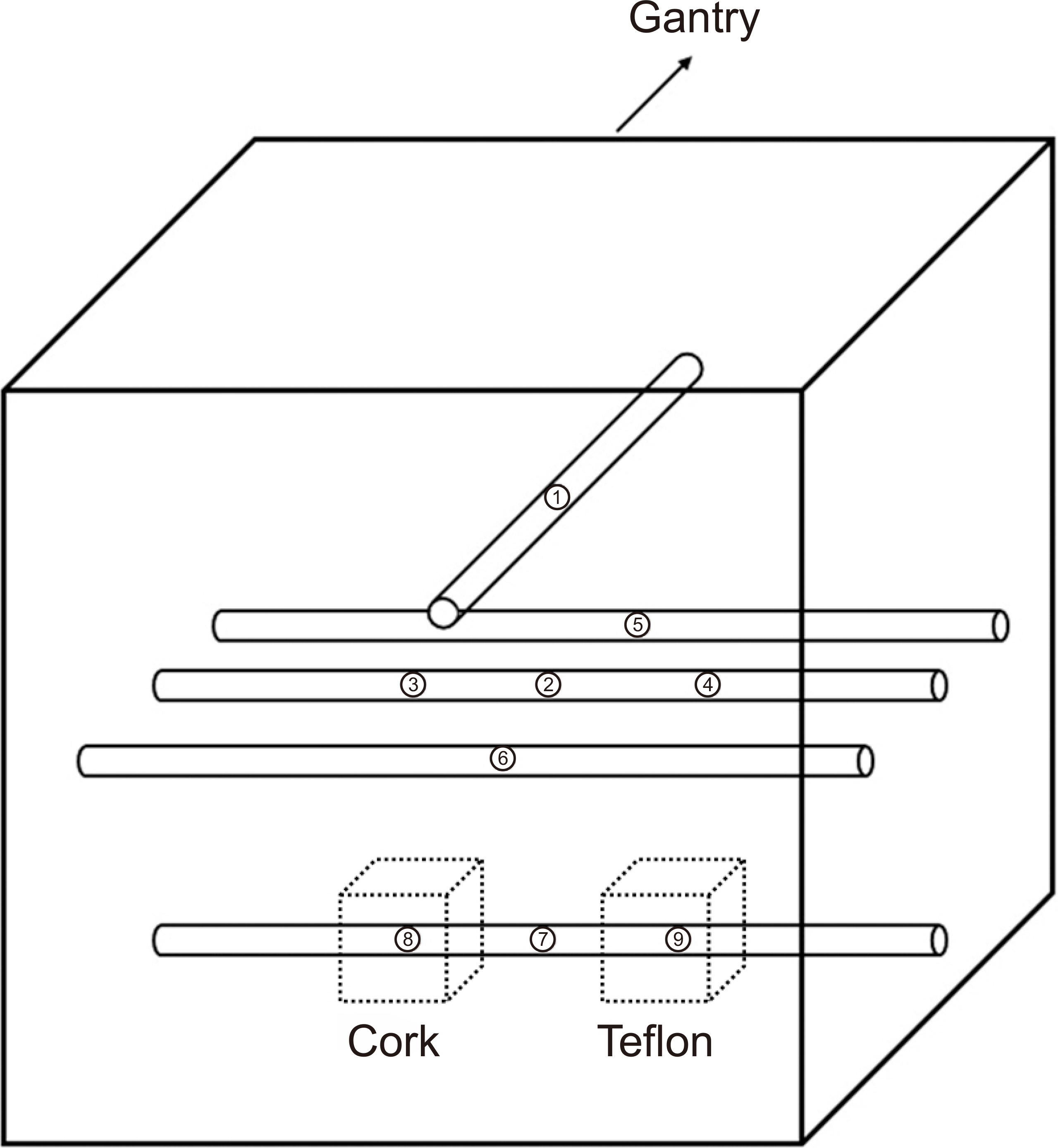
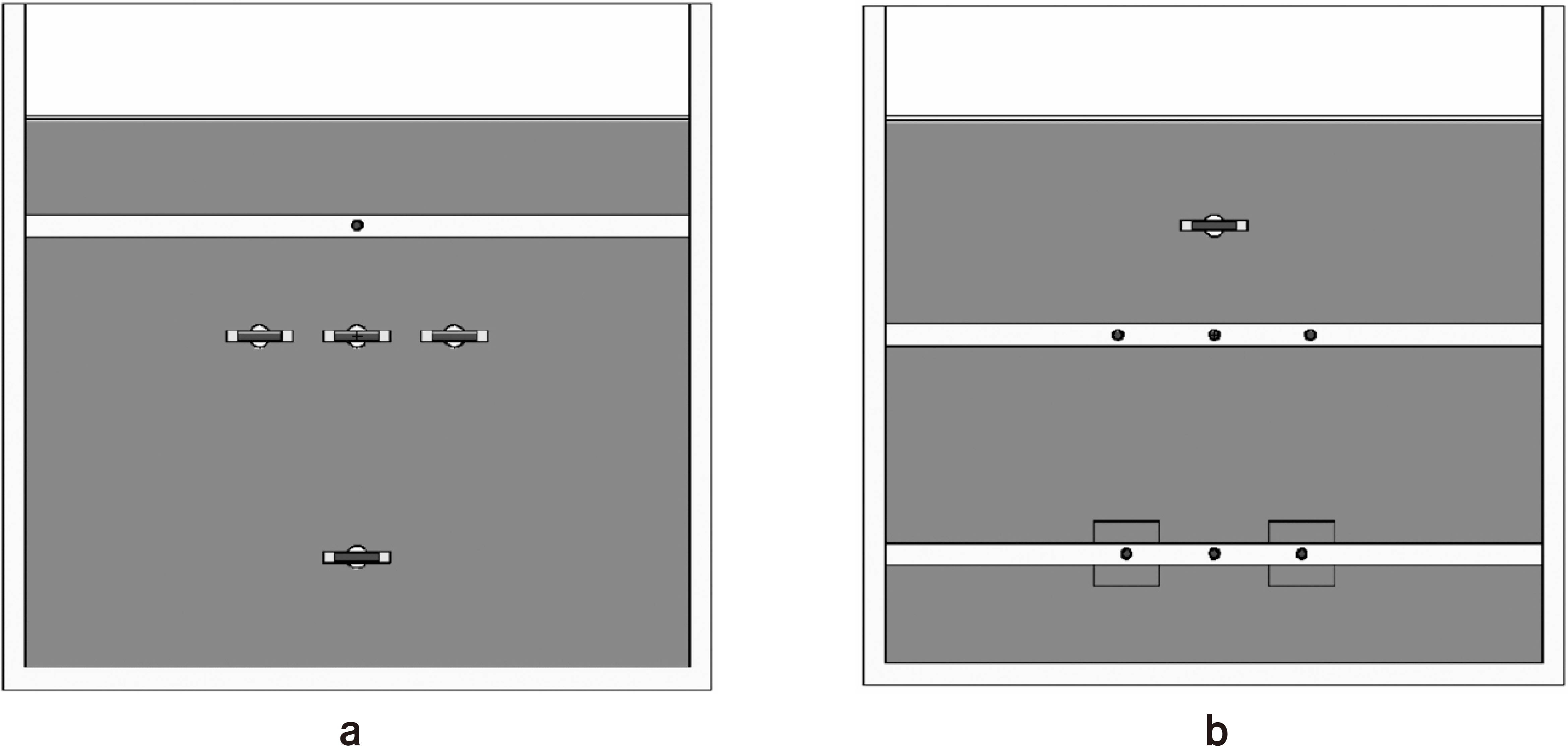
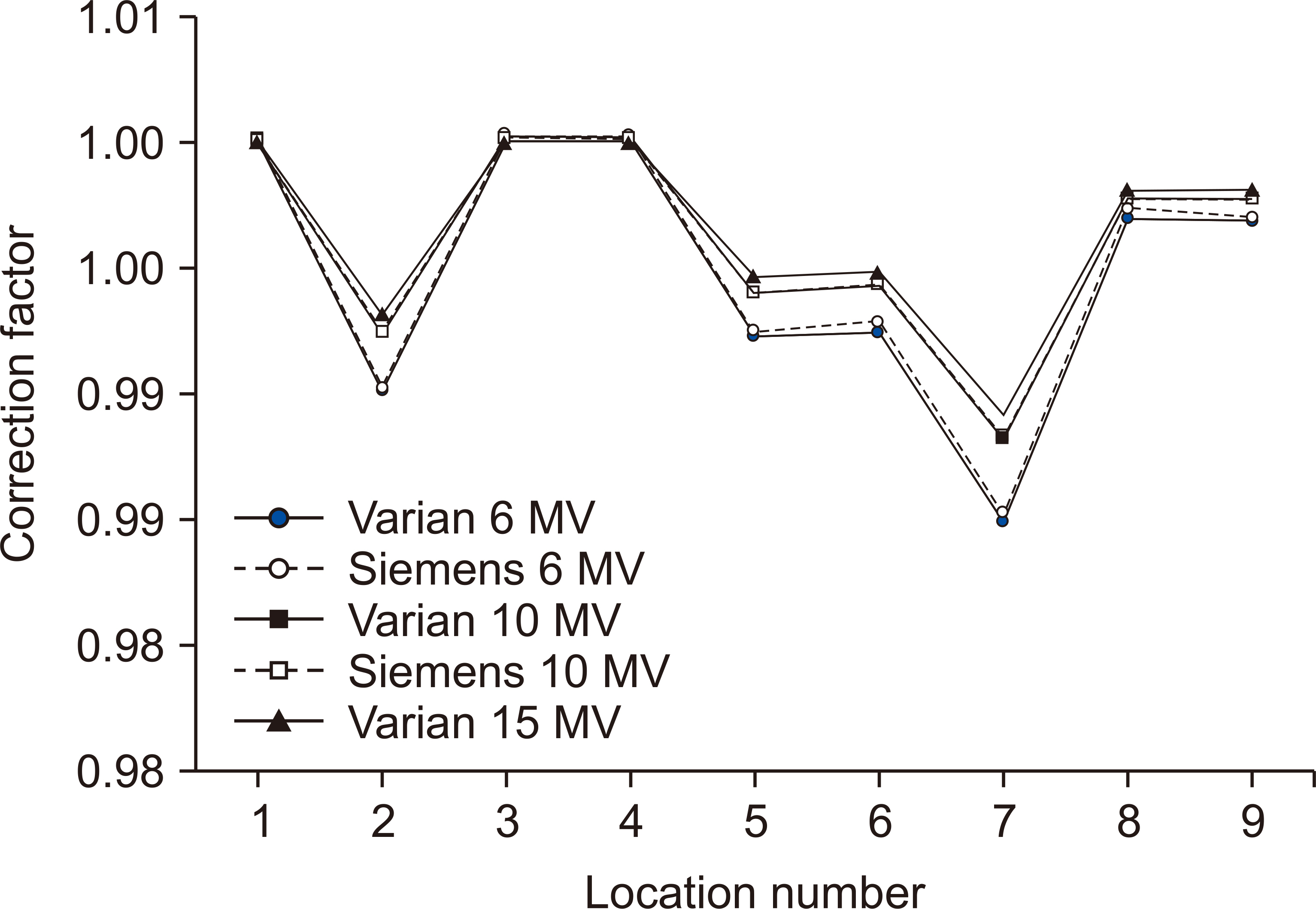
In this study, we used International Atomic Energy Agency (IAEA) LiF powder thermoluminescence dosimeter (TLD), which is generally used in the therapeutic radiation dose assurance project. The newly designed multipurpose phantom (MPP) consists of a container filled with water, a TLD holder, and two water-pressing covers. The size of the phantom was designed to be sufficient (30×30×30 cm3 ). The water container was filled with water and pressed with the cover for normal incidence to be fixed. The surface of the MPP was devised to maintain the same distance from the source at all times, even in the case of oblique incidence regardless of the water level. The MPP was irradiated with 6, 10, and 15 MV photon beams from Varian Linear Accelerator and measured by a 1.25 cm3 ionization chamber to get the correction factors. Monte Carlo (MC) simulation was also used to compare the measurements.
Results
The result obtained by MC had a relatively high uncertainty of 1% at the dosimetry point, but it showed a correction factor value of 1.3% at the 5 cm point. The energy dependence was large at 6 MV and small at 15 MV. Various dosimetric parameters for external audits can be performed within an hour.
Conclusions
The results allow an objective comparison of the quality assurance (QA) of individual hospitals. Therefore, this can be employed for external audits or QA systems in radiation therapy institutions.
Figure
Reference
-
References
1. Hoornaert MT, Van Dam J, Vynckier S, Bouiller A. 1993; A dosimetric quality audit of photon beams by the Belgian Hospital Physicist Association. Radiother Oncol. 28:37–43. DOI: 10.1016/0167-8140(93)90183-9.
Article2. Nisbet A, Thwaites DI, Sheridan ME. 1998; A dosimetric intercomparison of kilovoltage X-rays, megavoltage photons and electrons in the Republic of Ireland. Radiother Oncol. 48:95–101. DOI: 10.1016/S0167-8140(98)00041-3.
Article3. Nisbet A, Thwaites DI. 1997; A dosimetric intercomparison of electron beams in UK radiotherapy centres. Phys Med Biol. 42:2393–2409. DOI: 10.1088/0031-9155/42/12/007. PMID: 9434296.
Article4. Choi CH, Kim JI, Park JM, Park YK, Cho KW, Cho WK, et al. 2010; External auditing on absorbed dose using a solid water phantom for domestic radiotherapy facilities. J Korean Soc Ther Radiol Oncol. 28:50–56. DOI: 10.3857/jkstro.2010.28.1.50.
Article5. Davis B, Faessler P. 1993; Quality audit of megavoltage radiotherapy units: intercomparison of dose at a reference point using a mailed TL-dosimetry system. Radiother Oncol. 28:79–81. DOI: 10.1016/0167-8140(93)90191-A.
Article6. Derreumaux S, Chavaudra J, Bridier A, Rossetti V, Dutreix A. 1995; A European quality assurance network for radiotherapy: dose measurement procedure. Phys Med Biol. 40:1191–1208. DOI: 10.1088/0031-9155/40/7/004. PMID: 7568377.
Article7. Dutreix A, Derreumaux S, Chavaudra J, van der Schueren E. 1994; Quality control of radiotherapy centres in Europe: beam calibration. Radiother Oncol. 32:256–264. DOI: 10.1016/0167-8140(94)90025-6.
Article8. Dutreix A, van der Schueren E, Derreumaux S, Chavaudra J. 1993; Preliminary results of a quality assurance network for radiotherapy centres in Europe. Radiother Oncol. 29:97–101. DOI: 10.1016/0167-8140(93)90232-W.
Article9. Hansson U, Johansson KA. 1991; Quality audit of radiotherapy with EORTC mailed in water TL-dosimetry. Radiother Oncol. 20:191–196. DOI: 10.1016/0167-8140(91)90096-Y.
Article10. Huntley R, Izewska J. 2000; The 1998 Australian external beam radiotherapy survey and IAEA/WHO TLD postal dose quality audit. Australas Phys Eng Sci Med. 23:21–29.11. Izewska J, Novotny J, Gwiazdowska B, Kindlova A, Kontra G, van Dam J, et al. 1995; External audit on output calibration for photon beams. Acta Oncol. 34:829–838. DOI: 10.3109/02841869509127193. PMID: 7576752.12. Ferreira IH, Dutreix A, Bridier A, Chavaudra J, Svensson H. 2000; The ESTRO-QUALity assurance network (EQUAL). Radiother Oncol. 55:273–284. DOI: 10.1016/S0167-8140(99)00101-2.
Article13. Izewska J, Andreo P. 2000; The IAEA/WHO TLD postal programme for radiotherapy hospitals. Radiother Oncol. 54:65–72. DOI: 10.1016/S0167-8140(99)00164-4.
Article14. Svensson H, Hanson GP, Zsdanszky K. 1989. SSDL newsletter. No. 28. The IAEA/WHO TL dosimetry service for radiotherapy centres. 1969-1987. International Atomic Energy Agency (IAEA);Vienna: p. 3–23. DOI: 10.3109/02841869009090030. PMID: 2390272.15. Swinnen A, Verstraete J, Huyskens D. 2002; The use of a multipurpose phantom for mailed dosimetry checks of therapeutic photon beams: 'OPERA' (operational phantom for external radiotherapy audit). Radiother Oncol. 64:317–326. DOI: 10.1016/S0167-8140(02)00186-X.
Article16. Bridier A, Nyström H, Ferreira I, Gomola I, Huyskens D. 2000; A comparative description of three multipurpose phantoms (MPP) for external audits of photon beams in radiotherapy: the water MPP, the Umeå MPP and the EC MPP. Radiother Oncol. 55:285–293. DOI: 10.1016/S0167-8140(99)00169-3.
Article17. Almond PR, Biggs PJ, Coursey BM, Hanson WF, Huq MS, Nath R, et al. 1999; AAPM's TG-51 protocol for clinical reference dosimetry of high-energy photon and electron beams. Med Phys. 26:1847–1870. DOI: 10.1118/1.598691. PMID: 10505874.
Article18. Mobit PN, Mayles P, Nahum AE. 1996; The quality dependence of LiF TLD in megavoltage photon beams: Monte Carlo simulation and experiments. Phys Med Biol. 41:387–398. DOI: 10.1088/0031-9155/41/3/004. PMID: 8778821.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- External Auditing on Absorbed Dose Using a Solid Water Phantom for Domestic Radiotherapy Facilities
- Development of Dose Verification Method for In vivo Dosimetry in External Radiotherapy
- Analysis for Internal Audit and External Audit of the Sanitation/Safety Management Performance for the School Foodservice in Gyeongbuk Area
- Application of IAEA TRS-398 Protocol to Gamma Knife Model C
- Study of Respiration Simulating Phantom using Thermocouple-based Respiration Monitoring Mask