J Neurocrit Care.
2021 Dec;14(2):113-116. 10.18700/jnc.210025.
Supranuclear oculomotor palsy in cerebral venous sinus thrombosis: a case report
- Affiliations
-
- 1Department of Neurology, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India
- KMID: 2523722
- DOI: http://doi.org/10.18700/jnc.210025
Abstract
- Background
For certain ocular movement abnormalities, the exact neuroanatomical localization of the causative lesion is still not defined. Oculomotor apraxia, apraxia of eye opening and closing, and motor impersistence are rarely reported in acute stroke, particularly following venous stroke.
Case Report
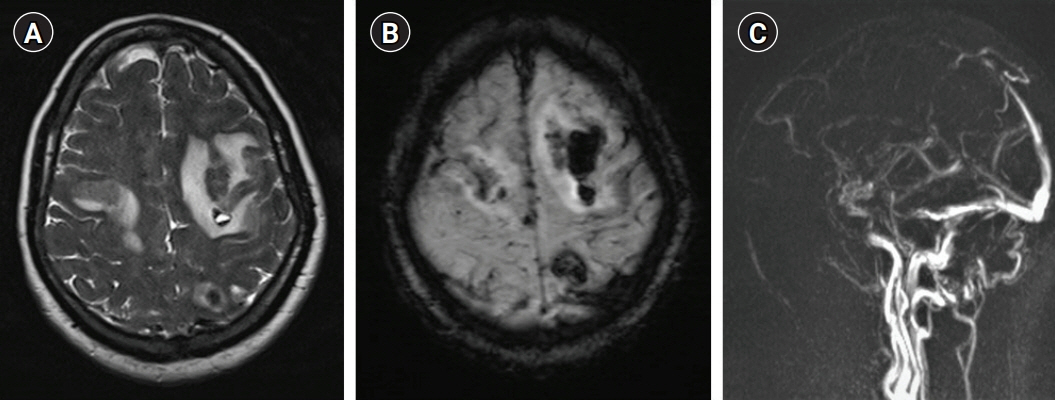
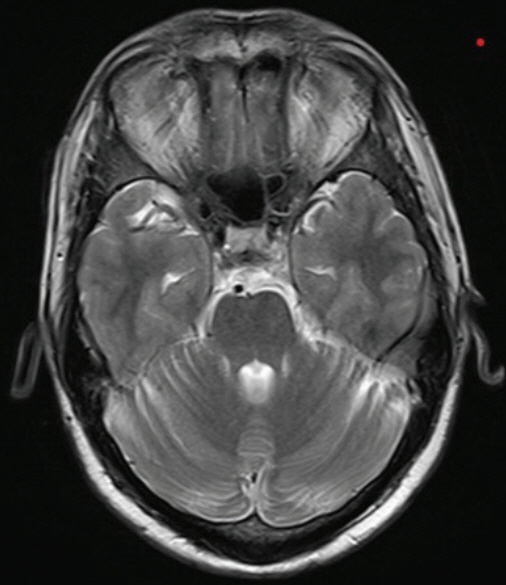
A 34-year-old man presented with headache, vomiting, focal seizures with bilateral tonic-clonic movements, and altered sensorium. Magnetic resonance imaging revealed bilateral frontal and left parietal hemorrhagic infarcts, and contrast venography revealed superior sagittal sinus thrombosis. The patient received anticoagulant treatment with antiepileptics. On re-examination on day 3, the patient had a rare combination of apraxia of eyelid closure, motor impersistence, and oculomotor apraxia. By Day 10 of admission, all oculomotor abnormalities had subsided.
Conclusion
To the best of our knowledge, this is the first report of the combination of oculomotor apraxia and apraxia of eyelid closure with motor impersistence in a patient with cerebral venous sinus thrombosis.
Figure
Reference
-
1. Hamedani AG, Gold DR. Eyelid dysfunction in neurodegenerative, neurogenetic, and neurometabolic disease. Front Neurol. 2017; 8:329.
Article2. Lewandowsky M. Über apraxie des lidschlusses. Berl Klin Wochenschr. 1907; 44:921–3.3. Nicoletti T, Quaranta D, Della Marca G, Tasca G, Gainotti G. Eyelid closing and opening disorders in patients with unilateral brain lesions: a case report with video neuroimage and a systematic review of the literature. J Clin Neurosci. 2021; 87:69–73.
Article4. van Koningsbruggen MG, Peelen MV, Davies E, Rafal RD. Neural control of voluntary eye closure: a case study and an fMRI investigation of blinking and winking. Behav Neurol. 2012; 25:103–9.
Article5. Cogan DG. A type of congenital ocular motor apraxia presenting jerky head movements. Am J Ophthalmol. 1953; 36:433–41.
Article6. Lal V, Truong D. Eye movement abnormalities in movement disorders. Clin Park Relat Disord. 2019; 1:54–63.
Article7. Fisher M. Left hemiplegia and motor impresistence. J Nerv Ment Dis. 1956; 123:201–18.8. Kertesz A, Nicholson I, Cancelliere A, Kassa K, Black SE. Motor impersistence: a right-hemisphere syndrome. Neurology. 1985; 35:662–6.
Article9. Kim EJ, Lee B, Jo MK, Jung K, You H, Lee BH, et al. Directional and spatial motor intentional disorders in patients with right versus left hemisphere strokes. Neuropsychology. 2013; 27:428–37.
Article10. Kim HJ, Kim D, Won DH, Chin J, Lee KH, Seo SW, et al. Callosal motor impersistence: a novel disconnection syndrome. Cogn Behav Neurol. 2017; 30:68–72.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Leptomeningeal Metastasis Associated with Cerebral Venous Thrombosis
- Cerebral Venous Sinus Thrombosis Associated with Antithrombin III Deficiency: A Case Report
- Neuro-Behcet's Disease Presented with Cerebral Venous Sinus Thrombosis: A Case Report
- Development of Subdural Hemorrhage in a Patient With Cerebral Venous Sinus Thrombosis
- Cerebral Venous Sinus Thrombosis: A Case Report