J Neurocrit Care.
2021 Dec;14(2):109-112. 10.18700/jnc.210030.
Which one to do first?: a case report of simultaneous acute ischemic stroke and myocardial infarction
- Affiliations
-
- 1Department of Neurology, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 2Department of Neurology, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Cardiology, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- KMID: 2523721
- DOI: http://doi.org/10.18700/jnc.210030
Abstract
- Background
Although there are common risk factors for acute ischemic stroke and myocardial infarction, simultaneous onset of both diseases is uncommon. Here, we present a case of acute cerebral infarction with concurrent fatal myocardial infarction.
Case Report
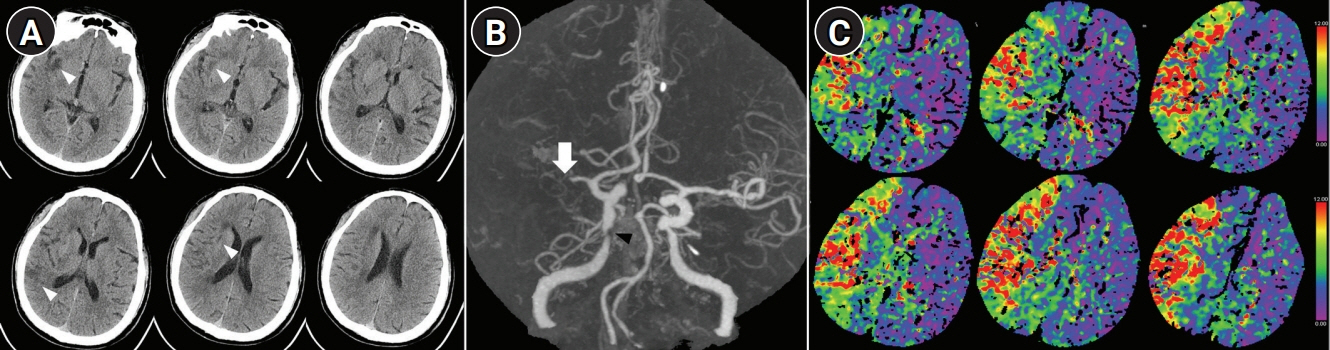
A 54-year-old man presented with left hemiparesis, gaze preponderance to the right side, and visual and tactile extinction. Computed tomography angiography showed occlusion of the right middle cerebral artery. ST-elevation myocardial infarction was suspected on electrocardiography. After the injection of intravenous tissue plasminogen activator, thrombectomy was attempted first, and the coronary angiogram was planned after recanalization of the cerebral artery. However, thrombectomy was discontinued because of cardiac arrest. Despite extracorporeal membrane oxygenation and emergency percutaneous coronary intervention, the patient died of multiorgan failure.
Conclusion
Double primary acute ischemic stroke and myocardial infarction are rare but may be fatal due to the narrow therapeutic time window for both diseases. Careful consideration of the urgency of cardiac status is essential.
Keyword
Figure
Reference
-
1. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020; 141:e139–596.
Article2. Meschia JF, Bushnell C, Boden-Albala B, Braun LT, Bravata DM, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:3754–832.3. Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010; 56:1113–32.4. Yeo LL, Andersson T, Yee KW, Tan BY, Paliwal P, Gopinathan A, et al. Synchronous cardiocerebral infarction in the era of endovascular therapy: which to treat first? J Thromb Thrombolysis. 2017; 44:104–111.
Article5. Omar HR, Fathy A, Rashad R, Helal E. Concomitant acute right ventricular infarction and ischemic cerebrovascular stroke: possible explanations. Int Arch Med. 2010; 3:25.
Article6. Kijpaisalratana N, Chutinet A, Suwanwela NC. Hyperacute simultaneous cardiocerebral infarction: rescuing the brain or the heart first? Front Neurol. 2017; 8:664.
Article7. Akinseye OA, Shahreyar M, Heckle MR, Khouzam RN. Simultaneous acute cardio-cerebral infarction: is there a consensus for management? Ann Transl Med. 2018; 6:7.
Article8. Verma GC, Jain G, Wahid A, Saurabh C, Sharma NK, Pathan AR, et al. Acute ischaemic stroke and acute myocardial infarction occurring together in domestic low-voltage (220-240V) electrical injury: a rare complication. J Assoc Physicians India. 2014; 62:620–3.9. Keskin M, Hayıroğlu Mİ, Keskin Ü, Eren M. Acute myocardial infarction and ischemic stroke coexistence due to marijuana abuse in an adolescent. Anatol J Cardiol. 2016; 16:542–3.
Article10. Muñiz AE. Myocardial infarction and stroke as the presenting symptoms of acute myeloid leukemia. J Emerg Med. 2012; 42:651–4.
Article11. Simpson DL. Simultaneous acute myocardial infarction, stroke and critical limb ischaemia: an unusual presentation requiring multidisciplinary approach. BMJ Case Rep. 2021; 14:e241565.
Article12. Ibekwe E, Kamdar HA, Strohm T. Cardio-cerebral infarction in left MCA strokes: a case series and literature review. Neurol Sci. 2021; Sep. 29. [Epub]. https://doi.org/10.1007/s10072-021-05628-x.
Article13. de Castillo LL, Diestro JD, Tuazon CA, Sy MC, Añonuevo JC, San Jose MC. Cardiocerebral infarction: a single institutional series. J Stroke Cerebrovasc Dis. 2021; 30:105831.
Article14. Ng TP, Wong C, Leong EL, Tan BY, Chan MY, Yeo LL, et al. Simultaneous cardio-cerebral infarction: a meta-analysis. QJM. 2021; May. 29. [Epub]. https://doi.org/10.1093/qjmed/hcab158. Online ahead of print.
Article15. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–418.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Myocardial Infarction with Simultaneous Thrombosis of Multiple Coronary Arteries
- Two patients with acute myocardial infarction presenting with simultaneous acute ischemic stroke
- Simultaneously Presented Acute Ischemic Stroke and Non-ST Elevation Myocardial Infarction in a Patient with Paroxysmal Atrial Fibrillation
- ST-Elevation Myocardial Infarction after Intravenous Thrombolysis Treatment for Acute Ischemic Stroke
- Simultaneous Onset of Ischemic and Hemorrhagic Stroke Due To Intracranial Artery Dissection