Korean J healthc assoc Infect Control Prev.
2021 Dec;26(2):89-95. 10.14192/kjicp.2021.26.2.89.
A Retrospective Descriptive Study on the Status of Active Tuberculosis among Healthcare Workers in a Tertiary Hospital
- Affiliations
-
- 1Yonsei University Shinchon Severance Hospital, Seoul, Korea
- KMID: 2523606
- DOI: http://doi.org/10.14192/kjicp.2021.26.2.89
Abstract
- Background
Healthcare workers are vulnerable to tuberculosis because they are frequently exposed to patients with active tuberculosis. This study aimed to describe the clinical and epidemiological characteristics of active tuberculosis among healthcare workers in a hospital in South Korea.
Methods
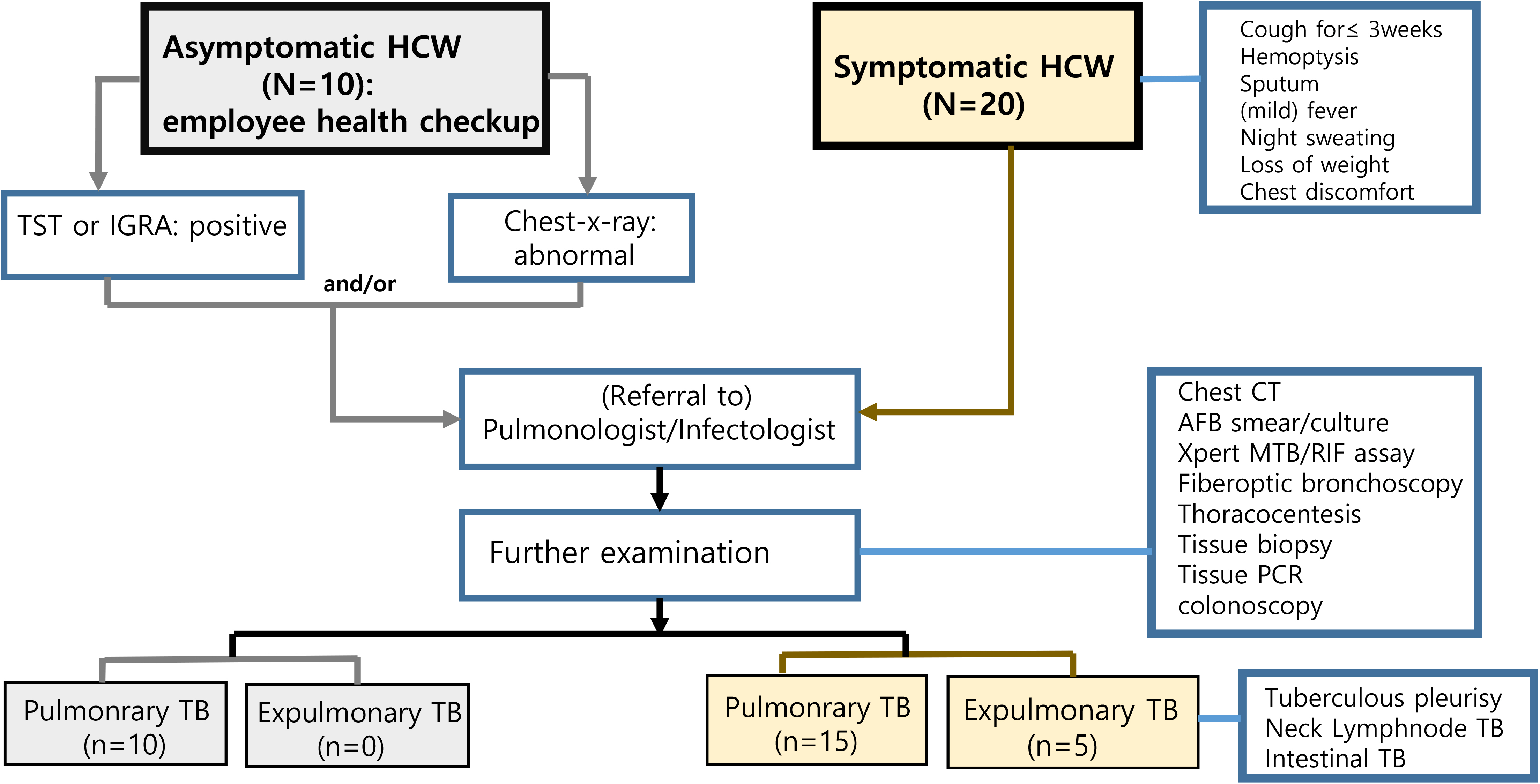
This retrospective descriptive study included 30 healthcare workers diagnosed with active tuberculosis between 2009 and 2019 in a tertiary hospital in South Korea. We reviewed the medical records for clinical findings and treatment processes. Their baseline characteristics were analyzed based on the presence or absence of symptoms. The risk of developing active tuberculosis by not only occupational groups in the medical field but also high-risk groups with possibility of contact with patients with tuberculosis was evaluated.
Results
Female healthcare workers accounted for 83.3% of the participants. The average age was 31.7 years, and the average duration from employment to diagnosis was 52.69 months. Of the subjects, 6.7% had a body mass index of <18.5 kg/m2 . Moreover, 86.7% were in the normal weight range. The most frequent symptom was cough for >3 weeks. The acid-fast bacillus (AFB) smear test and AFB culture were performed for all participants. Furthermore, 70% of the samples showed positive culture results. Regarding occupational distribution, the number of nurses was highest at 56%. The majority of healthcare workers worked in high-risk areas, being in contact with patients with tuberculosis. Pulmonary tuberculosis was noted in 25 patients. The other five patients had extrapulmonary tuberculosis. All subjects were treated with primary anti-tuberculosis medications. The average treatment duration was 6 months (66.7%).
Conclusion
Healthcare workers who work in areas with possibility of contact with patients with tuberculosis are at high risk of active tuberculosis infection. Therefore, continuous screening and comprehensive tests are required.
Keyword
Figure
Reference
-
1. Korean National Tuberculosis Association. Domestic current tuberculosis status report 2019. https://www.knta.or.kr/tbInfo/tbCondition/tbCondition.asp . Updated on 12 November 2021.2. Jo KW, Woo JH, Hong Y, Choi CM, Oh YM, Lee SD, et al. 2008; Incidence of tuberculosis among health care workers at a private university hospital in South Korea. Int J Tuberc Lung Dis. 12:436–40. PMID: 18371271.3. Cho KS, Park WS, Jeong HR, Kim MJ, Park SJ, Park AY, et al. 2018; Prevalence of latent tuberculosis infection at congregated settings in the Republic of Korea, 2017. Public Health Wkly Rep. 11:348–54.4. Yeon JH, Seong H, Hur H, Park Y, Kim YA, Park YS, et al. 2018; Prevalence and risk factors of latent tuberculosis among Korean healthcare workers using whole-blood interferon-γ release assay. Sci Rep. 8:10113. DOI: 10.1038/s41598-018-28430-w. PMID: 29973678. PMCID: PMC6031657.
Article5. Korea Centers for Disease Control. Announcement of latent tuberculosis infection screening project results in group facilities (2017-2018). https://www.kdca.go.kr/board.es?mid=a20501000000&bid=0015&act=view&list_no=366971 . Updated on 23 April 2020.6. Korea Centers for Disease Control. 2016. Guidance of TB in health care institutions. 2nd rev. ed. Korea Centers for Disease Control and Prevention;Cheongju: p. 14–9.7. Mirtskhulava V, Kempker R, Shields KL, Leonard MK, Tsertsvadze T, del Rio C, et al. 2008; Prevalence and risk factors for latent tuberculosis infection among health care workers in Georgia. Int J Tuberc Lung Dis. 12:513–9. PMID: 18419886. PMCID: PMC2742226.8. Rafiza S, Rampal KG, Tahir A. 2011; Prevalence and risk factors of latent tuberculosis infection among health care workers in Malaysia. BMC Infect Dis. 11:19. DOI: 10.1186/1471-2334-11-19. PMID: 21244645. PMCID: PMC3033828.
Article9. Prado TND, Riley LW, Sanchez M, Fregona G, Nóbrega RLP, Possuelo LG, et al. 2017; Prevalence and risk factors for latent tuberculosis infection among primary health care workers in Brazil. Cad Saude Publica. 33:e00154916. DOI: 10.1590/0102-311X00154916. PMID: 29267691.
Article10. Park JS. 2018; The prevalence and risk factors of latent tuberculosis infection among health care workers working in a tertiary hospital in South Korea. Tuberc Respir Dis (Seoul). 81:274–80. DOI: 10.4046/trd.2018.0020. PMID: 30238715. PMCID: PMC6148103.
Article11. Ngo CQ, Manabe T, Vu GV, Chu HT, Vu TTT, Tran TT, et al. 2019; Difficulties in tuberculosis infection control in a general hospital of Vietnam: a knowledge, attitude, and practice survey and screening for latent tuberculosis infection among health professionals. BMC Infect Dis. 19:951. DOI: 10.1186/s12879-019-4593-z. PMID: 31703561. PMCID: PMC6842132.
Article12. Graves SK, Augusto O, Viegas SO, Lederer P, David C, Lee K, et al. 2019; Tuberculosis infection risk, preventive therapy care cascade and incidence of tuberculosis disease in healthcare workers at Maputo Central Hospital. BMC Infect Dis. 19:346. DOI: 10.1186/s12879-019-3966-7. PMID: 31023260. PMCID: PMC6485058.
Article13. Baussano I, Nunn P, Williams B, Pivetta E, Bugiani M, Scano F. 2011; Tuberculosis among health care workers. Emerg Infect Dis. 17:488–94. DOI: 10.3201/eid1703.100947. PMID: 21392441. PMCID: PMC3298382.
Article14. Jo KW, Hong Y, Park JS, Bae IG, Eom JS, Lee SR, et al. 2013; Prevalence of latent tuberculosis infection among health care workers in South Korea: a multicenter study. Tuberc Respir Dis (Seoul). 75:18–24. DOI: 10.4046/trd.2013.75.1.18. PMID: 23946754. PMCID: PMC3741469.
Article15. Kim SY, Park MS, Kim YS, Kim SK, Chang J, Kang YA. 2013; Conversion rates of an interferon-γ release assay and the tuberculin skin test in the serial monitoring of healthcare workers. Infection. 41:511–6. DOI: 10.1007/s15010-012-0356-0. PMID: 23104257.
Article16. Yoon CG, Oh SY, Lee JB, Kim MH, Seo Y, Yang J, et al. 2017; Occupational risk of latent tuberculosis infection in health workers of 14 military hospitals. J Korean Med Sci. 32:1251–7. DOI: 10.3346/jkms.2017.32.8.1251. PMID: 28665059. PMCID: PMC5494322.
Article17. Herzmann C, Sotgiu G, Bellinger O, Diel R, Gerdes S, Goetsch U, et al. 2017; Risk for latent and active tuberculosis in Germany. Infection. 45:283–90. DOI: 10.1007/s15010-016-0963-2. PMID: 27866367. PMCID: PMC5488071.
Article18. Alonso-Echanove J, Granich RM, Laszlo A, Chu G, Borja N, Blas R, et al. 2001; Occupational transmission of Mycobacterium tuberculosis to health care workers in a university hospital in Lima, Peru. Clin Infect Dis. 33:589–96. DOI: 10.1086/321892. PMID: 11477527.19. Griffith DE, Hardeman JL, Zhang Y, Wallace RJ, Mazurek GH. 1995; Tuberculosis outbreak among healthcare workers in a community hospital. Am J Respir Crit Care Med. 152:808–11. DOI: 10.1164/ajrccm.152.2.7633747. PMID: 7633747.
Article20. Alele FO, Franklin RC, Emeto TI, Leggat P. 2019; Occupational tuberculosis in healthcare workers in sub-Saharan Africa: a systematic review. Arch Environ Occup Health. 74:95–108. DOI: 10.1080/19338244.2018.1461600. PMID: 29702035.
Article21. Sharma SK, Vashishtha R, Chauhan LS, Sreenivas V, Seth D. 2017; Comparison of TST and IGRA in diagnosis of latent tuberculosis infection in a high TB-burden setting. PLoS One. 12:e0169539. DOI: 10.1371/journal.pone.0169539. PMID: 28060926. PMCID: PMC5218498.
Article22. Nasiri MJ, Pormohammad A, Goudarzi H, Mardani M, Zamani S, Migliori GB, et al. 2019; Latent tuberculosis infection in transplant candidates: a systematic review and meta-analysis on TST and IGRA. Infection. 47:353–61. DOI: 10.1007/s15010-019-01285-7. PMID: 30805899.
Article23. Auguste P, Tsertsvadze A, Pink J, Court R, McCarthy N, Sutcliffe P, et al. 2017; Comparing interferon-gamma release assays with tuberculin skin test for identifying latent tuberculosis infection that progresses to active tuberculosis: systematic review and meta-analysis. BMC Infect Dis. 17:200. DOI: 10.1186/s12879-017-2301-4. PMID: 28274215. PMCID: PMC5343308.
Article24. Abubakar I, Drobniewski F, Southern J, Sitch AJ, Jackson C, Lipman M, et al. 2018; Prognostic value of interferon-γ release assays and tuberculin skin test in predicting the development of active tuberculosis (UK PREDICT TB): a prospective cohort study. Lancet Infect Dis. 18:1077–87. DOI: 10.1016/S1473-3099(18)30355-4. PMID: 30174209. PMCID: PMC6192014.25. Little KM, Pai M, Dowdy DW. 2015; Costs and consequences of using interferon-γ release assays for the diagnosis of active tuberculosis in India. PLoS One. 10:e0124525. DOI: 10.1371/journal.pone.0124525. PMID: 25918999. PMCID: PMC4412573.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Treatment of Latent Tuberculosis Infection in Healthcare Workers
- Comparison of Working Conditions Between Immigrant and Non-immigrant Healthcare Workers in the United States: Evidence From the National Health Interview Survey
- Influences of Working Conditions and Health Status on Absence due to Sickness in Health and Medical related Workers
- Awareness of Hospital Safety Culture and Safety Activities of Workers in a Tertiary Care Hospital
- Current Status of Fluoroquinolone Use for Treatment of Tuberculosis in a Tertiary Care Hospital in Korea