Anat Cell Biol.
2021 Dec;54(4):479-488. 10.5115/acb.21.107.
Association between masticatory muscle activity and oral conditions in young female college students
- Affiliations
-
- 1Gimhae Jeil Dental Clinic, Gimhae, Korea
- 2Department of Occupational Therapy, Division of Health Sciences, Dongseo University, Busan, Korea
- 3Department of Dental Hygiene, Division of Health Sciences, Dongseo University, Busan, Korea
- KMID: 2523578
- DOI: http://doi.org/10.5115/acb.21.107
Abstract
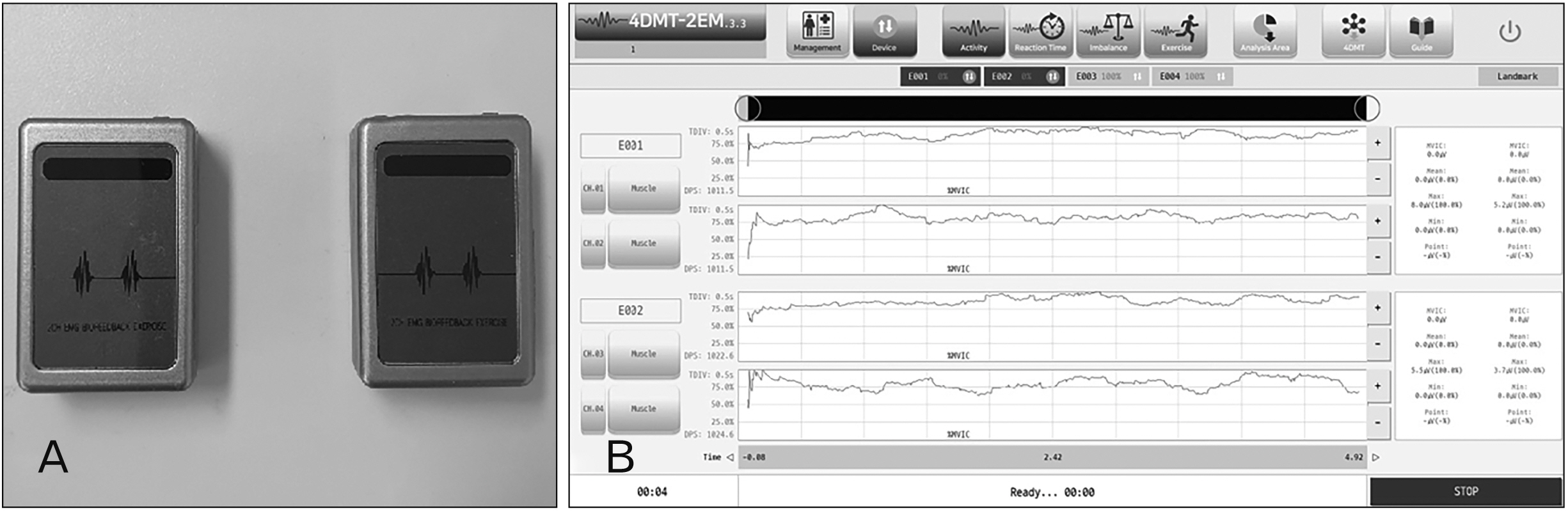
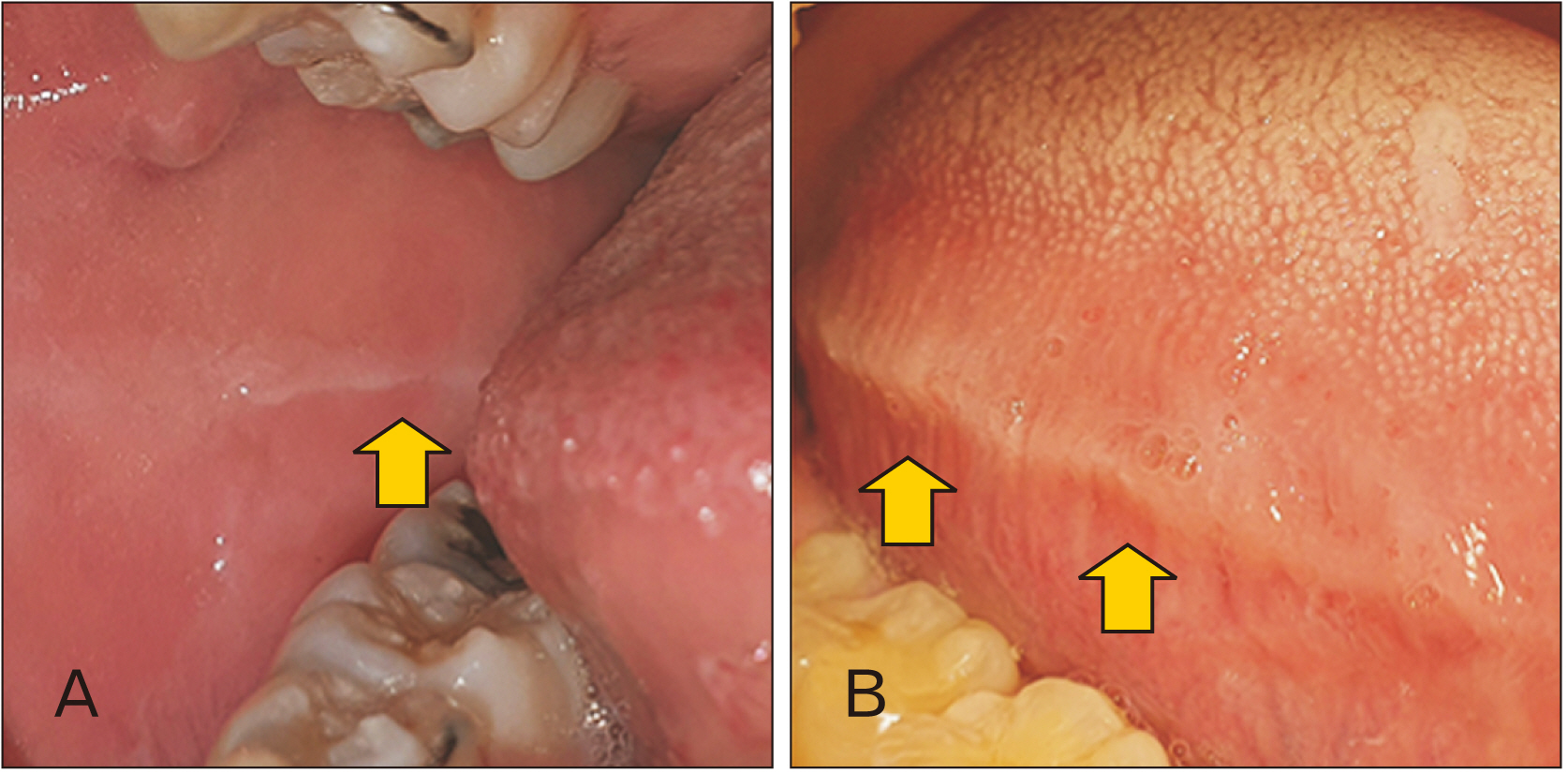
- The purpose of this study was to determine the characteristics of masticatory muscle activity and various oral condition factors, and to analyze their associations in order to improve the prevention and diagnosis of masticatory musclerelated diseases. This study included 30 Korean females (mean age of 20 years, age range of 19–21 years). Participants were instructed to complete a self-written questionnaire on factors that may affect their muscle activity. Surface electromyography was used to measure the activity of the masseter and temporalis muscles. We also observed the buccal mucosa ridge, tongue indentation, tooth cracks and fractures, and mandibular tori in the oral cavity. Spearman correlation analysis and the nonparametric Mann–Whitney U test were applied to the data. When subjects had temporomandibular disorder, the right temporalis muscle exhibited significantly lower activity (P<0.05). Those who had received orthodontic treatment within the previous 2 years showed significantly lower activity of the left masseter muscle (P<0.05). Those who had a left buccal mucosa ridge exhibited lower activity of the left masseter muscle and higher activity of the right temporalis muscle compared with those without such a ridge (P<0.05). Participants with no tongue indentation showed significantly higher activity in the left masseter muscle (P<0.05). These results indicate that there are relationships between masticatory muscle activity and various factors related to the oral condition.
Keyword
Figure
Reference
-
References
1. Carlsson GE, Droukas B. 1984; Dental occlusion and the health of the masticatory system. J Craniomandib Pract. 2:141–7. DOI: 10.1080/07345410.1984.11677859.
Article2. Romero-Reyes M, Uyanik JM. 2014; Orofacial pain management: current perspectives. J Pain Res. 7:99–115. DOI: 10.2147/JPR.S37593. PMID: 24591846. PMCID: PMC3937250.
Article3. Korean Oral Anatomy Research Group. 2017. Oral anatomy. Komoonsa;Seoul:4. Kim TH, Kim DH. 2019; The effects of head rotation and tilt on oral pressure and muscle activity. Anat Cell Biol. 52:378–84. DOI: 10.5115/acb.19.191. PMID: 31949975. PMCID: PMC6952685.
Article5. Aidsman IK. 1977; Glossary of prosthodontic terms. J Prosthet Dent. 38:66–109. DOI: 10.1016/0022-3913(77)90268-2. PMID: 28418832.6. Yoon HR, Choi YJ, Kim KH, Chung CR. 2010; Comparisons of occlusal force according to occlusal relationship, skeletal pattern, age and gender in Koreans. Korean J Orthod. 40:304–13. DOI: 10.4041/kjod.2010.40.5.304.
Article7. Kim HB, Bae SS. 1998; Clinical application of electromyography and nerve conduction study. J Korean Phys Ther Sci. 5:603–16.8. Takeuchi-Sato T, Arima T, Mew M, Svensson P. 2019; Relationships between craniofacial morphology and masticatory muscle activity during isometric contraction at different interocclusal distances. Arch Oral Biol. 98:52–60. DOI: 10.1016/j.archoralbio.2018.10.030. PMID: 30448395.
Article9. Custodio W, Gomes SG, Faot F, Garcia RC, Del Bel Cury AA. 2011; Occlusal force, electromyographic activity of masticatory muscles and mandibular flexure of subjects with different facial types. J Appl Oral Sci. 19:343–9. DOI: 10.1590/S1678-77572011005000008. PMID: 21655772. PMCID: PMC4223785.
Article10. Langlais RP, Miller CS, Gehrig JS. 2017. Color atlas of common oral diseases. 5th ed. Jones & Bartlett Learning;Burlington:11. Mizutani S, Ekuni D, Tomofuji T, Azuma T, Irie K, Machida T, Yoneda T, Iwasaki Y, Morita M. 2014; Factors related to the formation of buccal mucosa ridging in university students. Acta Odontol Scand. 72:58–63. DOI: 10.3109/00016357.2013.797102. PMID: 23692316. PMCID: PMC3878356.
Article12. Piquero K, Ando T, Sakurai K. 1999; Buccal mucosa ridging and tongue indentation: incidence and associated factors. Bull Tokyo Dent Coll. 40:71–8. DOI: 10.2209/tdcpublication.40.71. PMID: 10825817.
Article13. Miyaura K, Matsuka Y, Morita M, Yamashita A, Watanabe T. 1999; Comparison of biting forces in different age and sex groups: a study of biting efficiency with mobile and non-mobile teeth. J Oral Rehabil. 26:223–7. DOI: 10.1046/j.1365-2842.1999.00364.x. PMID: 10194731.
Article14. Al Quran FA, Al-Dwairi ZN. 2006; Torus palatinus and torus mandibularis in edentulous patients. J Contemp Dent Pract. 7:112–9. DOI: 10.5005/jcdp-7-2-112. PMID: 16685302.
Article15. De Luca Canto G, Torres de Freitas S, Schuldt Filho G, de Sousa Vieira R. 2013; Association between mandibular torus and parafunctional activity. J Stomat Occ Med. 6:43–9. DOI: 10.1007/s12548-012-0064-5.
Article16. Pechenkina EA, Benfer RA Jr. 2002; The role of occlusal stress and gingival infection in the formation of exostoses on mandible and maxilla from Neolithic China. Homo. 53:112–30. DOI: 10.1078/0018-442X-00040. PMID: 12489411.
Article17. Reddy MS, Geurs NC, Wang IC, Liu PR, Hsu YT, Jeffcoat RL, Jeffcoat MK. 2002; Mandibular growth following implant restoration: does Wolff's law apply to residual ridge resorption? Int J Periodontics Restorative Dent. 22:315–21.18. Shimomoto Y, Chung CJ, Iwasaki-Hayashi Y, Muramoto T, Soma K. 2007; Effects of occlusal stimuli on alveolar/jaw bone formation. J Dent Res. 86:47–51. DOI: 10.1177/154405910708600107. PMID: 17189462.
Article19. Fricton J. 2014; Temporomandibular disorders: a human systems approach. J Calif Dent Assoc. 42:523–33. discussion 531533–5. PMID: 25174211.20. Alkhalifah S, Alkandari H, Sharma PN, Moule AJ. 2017; Treatment of cracked teeth. J Endod. 43:1579–86. DOI: 10.1016/j.joen.2017.03.029. PMID: 28734650.
Article21. Cameron CE. 1976; The cracked tooth syndrome: additional findings. J Am Dent Assoc. 93:971–5. DOI: 10.14219/jada.archive.1976.0034. PMID: 61220.
Article22. Okeson JP. Okeson JP, editor. 2013. Etiology of functional disturbances in the masticatory system. Management of Temporomandibular Disorders and Occlusion. Elsevier;St. Louis: p. 130–63.23. Speciali JG, Dach F. 2015; Temporomandibular dysfunction and headache disorder. Headache. 55(Suppl 1):72–83. DOI: 10.1111/head.12515. PMID: 25644695.
Article24. Rani S, Pawah S, Gola S, Bakshi M. 2017; Analysis of Helkimo index for temporomandibular disorder diagnosis in the dental students of Faridabad city: a cross-sectional study. J Indian Prosthodont Soc. 17:48–52. DOI: 10.4103/0972-4052.194941. PMID: 28216845. PMCID: PMC5308067.
Article25. Kim HS. 2013. The relationship between oral tori and temporomandibular joint symptoms and oral parafunctions [MS dissertation]. Yonsei University;Seoul:26. Vitti M, Basmajian JV. 1975; Muscles of mastication in small children: an electromyographic analysis. Am J Orthod. 68:412–9. DOI: 10.1016/0002-9416(75)90182-7. PMID: 1058639.
Article27. Ahlgren J, Sonesson B, Blitz M. 1985; An electromyographic analysis of the temporalis function of normal occlusion. Am J Orthod. 87:230–9. DOI: 10.1016/0002-9416(85)90044-2. PMID: 3856396.
Article28. Lee HJ, Lee YW. 2019; Correlation between cyclists' quadriceps femoris thickness and isokinetic strength. Korean J Sport. 17:1617–24.29. Takagi I, Sakurai K. 2003; Investigation of the factors related to the formation of the buccal mucosa ridging. J Oral Rehabil. 30:565–72. DOI: 10.1046/j.1365-2842.2003.01144.x. PMID: 12787452.
Article30. Gould MS, Picton DC. 1968; A study of pressures exerted by the lips and cheeks on the teeth of subjects with angle's class II division 1, clss II division 2 and class 3 malocclusions compared with those of subjects with normal occlusions. Arch Oral Biol. 13:527–41. DOI: 10.1016/0003-9969(68)90113-1.31. Tallgren A, Melsen B, Hansen MA. 1979; An electromyographic and roentgen cephalometric study of occlusal morphofunctional disharmony in children. Am J Orthod. 76:394–409. DOI: 10.1016/0002-9416(79)90225-2. PMID: 291342.
Article32. Yanagisawa K, Takagi I, Sakurai K. 2007; Influence of tongue pressure and width on tongue indentation formation. J Oral Rehabil. 34:827–34. DOI: 10.1111/j.1365-2842.2007.01734.x. PMID: 17919249.
Article33. Yang KY, Han KS, Yeo IS. 2003; Masticatory muscle activity and bite force according to head postureand clenching level. J Oral Med Pain. 28:249–59.34. van Boxtel A, Boelhouwer AJ, Bos AR. 1998; Optimal EMG signal bandwidth and interelectrode distance for the recording of acoustic, electrocutaneous, and photic blink reflexes. Psychophysiology. 35:690–7. DOI: 10.1111/1469-8986.3560690. PMID: 9844430.
Article35. Schmid-Schwap M, Bristela M, Kundi M, Piehslinger E. 2013; Sex-specific differences in patients with temporomandibular disorders. J Orofac Pain. 27:42–50. DOI: 10.11607/jop.970. PMID: 23424719.
Article36. Santana-Mora U, Cudeiro J, Mora-Bermúdez MJ, Rilo-Pousa B, Ferreira-Pinho JC, Otero-Cepeda JL, Santana-Penín U. 2009; Changes in EMG activity during clenching in chronic pain patients with unilateral temporomandibular disorders. J Electromyogr Kinesiol. 19:e543–9. DOI: 10.1016/j.jelekin.2008.10.002. PMID: 19041265.
Article37. Raphael KG, Janal MN, Sirois DA, Svensson P. 2013; Effect of contingent electrical stimulation on masticatory muscle activity and pain in patients with a myofascial temporomandibular disorder and sleep bruxism. J Orofac Pain. 27:21–31. DOI: 10.11607/jop.1029. PMID: 23424717.
Article38. Santiago V, Raphael K. 2019; Absence of joint pain identifies high levels of sleep masticatory muscle activity in myofascial temporomandibular disorder. J Oral Rehabil. 46:1161–9. DOI: 10.1111/joor.12853. PMID: 31271666. PMCID: PMC8662550.
Article39. Wei F, Van Horn MH, Coombs MC, She X, Gonzales TS, Gonzalez YM, Scott JM, Iwasaki LR, Nickel JC, Yao H. 2017; A pilot study of nocturnal temporalis muscle activity in TMD diagnostic groups of women. J Oral Rehabil. 44:517–25. DOI: 10.1111/joor.12517. PMID: 28449265. PMCID: PMC5499232.
Article40. Valentino R, Cioffi I, Vollaro S, Cimino R, Baiano R, Michelotti A. 2021; Jaw muscle activity patterns in women with chronic TMD myalgia during standardized clenching and chewing tasks. Cranio. 39:157–63. DOI: 10.1080/08869634.2019.1589703. PMID: 30896353.
Article41. Han DH, Park DY, Kim BI, Koh MY, Ahn YW, Kim JB. 2011; Global self-rating of oral health, concerns about oral health, and history of jaw injury related to temporomandibular joint symptoms in Korean adults. J Orofac Pain. 25:308–16. PMID: 22247926.42. Choi Y, Park H, Lee JS, Park JC, Kim CS, Choi SH, Cho KS, Chai JK, Jung UW. 2012; Prevalence and anatomic topography of mandibular tori: computed tomographic analysis. J Oral Maxillofac Surg. 70:1286–91. DOI: 10.1016/j.joms.2011.12.009. PMID: 22310453.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Masticatory muscle tenderness in burning mouth syndrome: A case control study
- Correlation between mandibular morphology and masticatory muscle thickness in normal occlusion and mandibular prognathism
- Association between Temporomandibular Disorder and Masticatory Muscle Weakness: A Case report
- Tetanus and masticatory muscle spasm
- Trismus casued by inverse activity of masticatory muscles