J Korean Foot Ankle Soc.
2021 Dec;25(4):190-194. 10.14193/jkfas.2021.25.4.190.
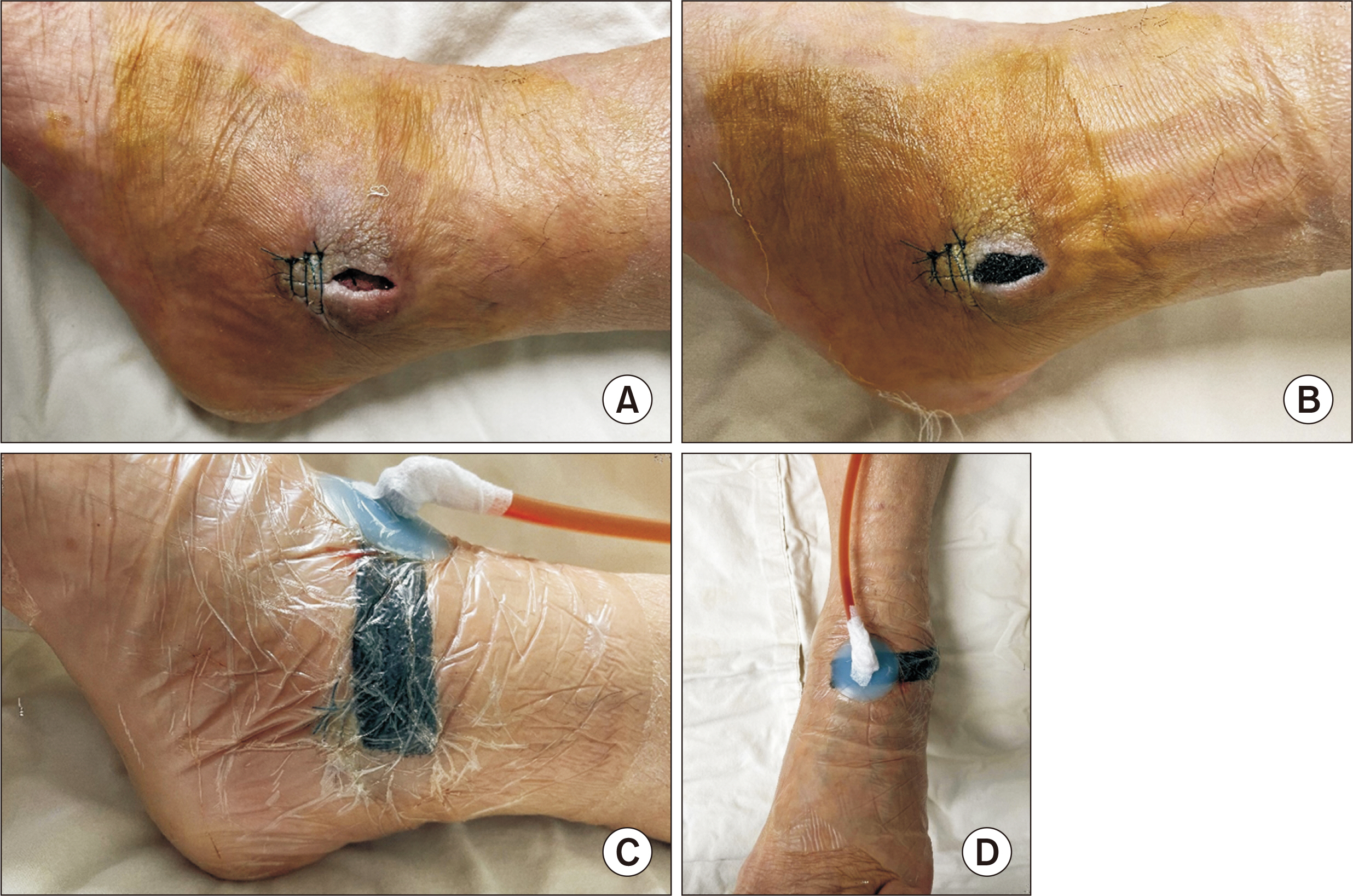
Negative-Pressure Wound Therapy for Septic Ankle Arthritis Following Intractable Lateral Malleolar Bursitis: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Kosin University College of Medicine, Busan, Korea
- KMID: 2523302
- DOI: http://doi.org/10.14193/jkfas.2021.25.4.190
Abstract
- A bursa is an obstructive sac filled with synovial fluid and usually occurs in any area of the body exposed to friction. The bursa of the ankle is not a normal anatomical structure and is caused by repetitive trauma, constant friction, or inflammatory disease of the ankle. Bursitis can occur in any bursa in the human body; however it rarely progresses to septic arthritis. We report a rare case of septic ankle arthritis following intractable lateral malleolar bursitis successfully treated with negative-pressure wound therapy.
Figure
Reference
-
References
1. Brown TD, Varney TE, Micheli LJ. 2000; Malleolar bursitis in figure skaters. Indications for operative and nonoperative treatment. Am J Sports Med. 28:109–11. doi: 10.1177/03635465000280010301. DOI: 10.1177/03635465000280010301. PMID: 10653553.2. Larsson LG, Baum J. 1986; The syndromes of bursitis. Bull Rheum Dis. 36:1–8. PMID: 3790856.3. Boutin FJ BR, Boutin FJ Jr. Chapman MW, Madison M, editors. 1993. Bursitis. Operative orthopaedics. 2nd ed. JB Lippincott Co;Philadelphia: p. 3419–32.4. Hernandez PA, Hernandez WA, Hernandez A. 1991; Clinical aspects of bursae and tendon sheaths of the foot. J Am Podiatr Med Assoc. 81:366–72. doi: 10.7547/87507315-81-7-366. DOI: 10.7547/87507315-81-7-366. PMID: 1941580.
Article5. Woo SH, Kim JS, Son SM, Shin WC. 2019; Triamcinolone acetonide injections for lateral malleolar bursitis of the ankle. J Korean Foot Ankle Soc. 23:12–7. doi: 10.14193/jkfas.2019.23.1.12. DOI: 10.14193/jkfas.2019.23.1.12.
Article6. Weston V, Coakley G. 2006; Guideline for the management of the hot swollen joint in adults with a particular focus on septic arthritis. J Antimicrob Chemother. 58:492–3. doi: 10.1093/jac/dkl295. DOI: 10.1093/jac/dkl295. PMID: 16857687.
Article7. Vispo Seara JL, Barthel T, Schmitz H, Eulert J. 2002; Arthroscopic treatment of septic joints: prognostic factors. Arch Orthop Trauma Surg. 122:204–11. doi: 10.1007/s00402-001-0386-z. DOI: 10.1007/s00402-001-0386-z. PMID: 12029509.8. Argenta LC, Morykwas MJ. 1997; Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 38:563–76. discussion 577doi: 10.1097/00000637-199706000-00002. DOI: 10.1097/00000637-199706000-00002. PMID: 9188971.9. Kim BS, Choi WJ, Baek MK, Kim YS, Lee JW. 2011; Limb salvage in severe diabetic foot infection. Foot Ankle Int. 32:31–7. doi: 10.3113/FAI.2011.0031. DOI: 10.3113/FAI.2011.0031. PMID: 21288432.
Article10. Birke-Sorensen H, Malmsjo M, Rome P, Hudson D, Krug E, Berg L, et al. Evidence-based recommendations for negative pressure wound therapy: treatment variables (pressure levels, wound filler and contact layer)--steps towards an international consensus. J Plast Reconstr Aesthet Surg. 2011; 64 Suppl:S1–16. doi: 10.1016/j.bjps.2011.06.001. DOI: 10.1016/j.bjps.2011.06.001. PMID: 21868296.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Secondary Septic Arthritis Due to Lateral Malleolar Bursitis: A Case Report
- Surgery for Synovial Fistula after Excision of the Lateral Malleolar Bursitis of the Ankle: A Case Report
- Outcomes of Lateral Malleolar Saving versus Sacrificing Procedure in Transfibular Ankle Arthrodesis
- Endoscopy versus Open Bursectomy of Lateral Malleolar Bursitis; Comparative Study
- The Effect of Indwelling Silk Suture Following Aspiration in the Treatment of Chronic Lateral Malleolar Bursitis