Impact of the COVID-19 Pandemic on the Mental Health of Adolescent Students in Daegu, Korea
- Affiliations
-
- 1Department of Psychiatry, School of Medicine, Keimyung University, Daegu, Korea
- 2Department of Psychiatry, Keimyung University Dongsan Medical Center, Daegu, Korea
- 3Daegu Student Suicide Prevention Center, Kyungpook National University Chilgok Hospital, Daegu, Korea
- 4Wee Center in Kyungpook National University Hospital, Kyungpook National University Chilgok Hospital, Daegu, Korea
- 5Department of Physical Education and Health, Daegu Metropolitan Office of Education, Daegu, Korea
- 6Department of Psychiatry, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2522890
- DOI: http://doi.org/10.3346/jkms.2021.36.e321
Abstract
- Background
In February 2020, as coronavirus disease 2019 (COVID-19) spread rapidly in Daegu, South Korea, students in that region experienced many emotional difficulties. In this study, we analyzed the stress and emotional crisis experienced by students during the COVID-19 pandemic, its causative factors, and the factors that affect negative emotions.
Methods
We identified the demographic information related to the experiences of unbearable stress and emotional crisis and their causal factors at three points in time: before the pandemic, during its peak, and at the time of the survey (2–3 months after the peak). In addition, we analyzed the factors related to depression and anxiety experienced by students during the COVID-19 pandemic. The Korean version of the Patient Health Questionnaire 9 and the Korean version of the Generalized Anxiety Disorder 7 was used to assess for depressive and anxiety symptoms in the subject students, respectively.
Results
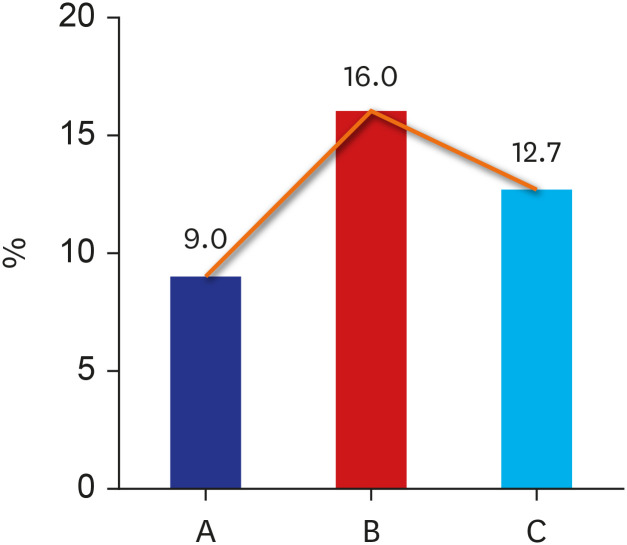
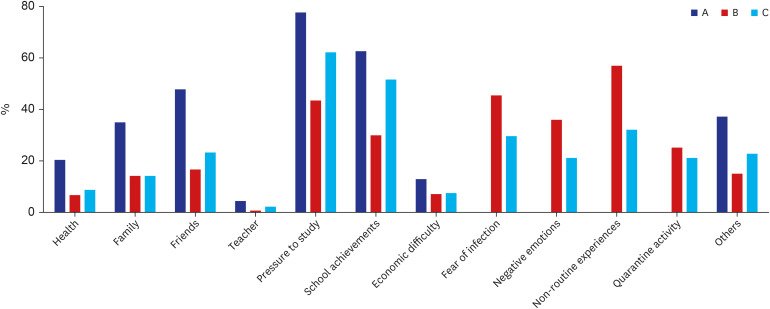
A total of 8,177 students participated in the analysis, with 4,072 boys (49.8%), 4,105 girls (50.2%), and 4,463 middle school students (54.6%) and 3,177 high school students (45.4%). The percentage of students who experienced unbearable stress was 9% before the COVID-19 pandemic, increased to 16% at the peak of the COVID-19 pandemic, then decreased to 12.7% at the time of the survey. Stress was experienced more by girls (18.1% versus 13.8% in boys; χ2 = 28.159, P < 0.001) and high school students (19.0% versus 13.5% in middle school students; χ2 = 45.437, P < 0.001). Overall, 7.6% experienced emotional crises during the COVID-19 pandemic, which was more prevalent in girls (10.1% versus 5.2% in boys; χ2 = 71.025, P < 0.001) and in high school students (8.8% versus 6.7% in middle school students; χ2 = 12.996, P < 0.001). Depression and anxiety was seen in 19.8% and 12.3% of students during the COVID-19 pandemic, respectively. The risk factors for depression and anxiety included unbearable stress before the COVID-19 pandemic (P < 0.001), mental health (P = 0.044), and age (P = 0.040), whereas resilience was identified as a protective factor for depression and anxiety (P = 0.001).
Conclusion
Students in Daegu experienced lots of mental difficulties since the COVID-19 pandemic. It will be necessary to improve stress management and resilience to improve students' mental health in disasters such as the COVID-19 pandemic.
Keyword
Figure
Cited by 3 articles
-
Factors Related to Anxiety and Depression Among Adolescents During COVID-19: A Web-Based Cross-Sectional Survey
Kyung-Shin Lee, Ho Kyung Sung, So Hee Lee, Jinhee Hyun, Heeguk Kim, Jong-Sun Lee, Jong-Woo Paik, Seok-Joo Kim, Sunju Sohn, Yun-Kyeung Choi
J Korean Med Sci. 2022;37(25):e199. doi: 10.3346/jkms.2022.37.e199.Mental Health of Adolescents and Subjective Economic Deterioration Caused by COVID-19 in Korea
JaeHyuck Lee, Seung Wan Hong, Keonyeop Kim
J Korean Med Sci. 2022;37(35):e268. doi: 10.3346/jkms.2022.37.e268.Impact of the COVID-19 Pandemic on Gender Differences in Depression Based on National Representative Data
Hyunsuk Jeong, Hyeon Woo Yim, Seung-Yup Lee, Da Young Jung
J Korean Med Sci. 2023;38(6):e36. doi: 10.3346/jkms.2023.38.e36.
Reference
-
1. World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. Updated 2020. Accessed April 15, 2017. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 .2. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395(10223):497–506. PMID: 31986264.
Article3. Kim JY, Choe PG, Oh Y, Oh KJ, Kim J, Park SJ, et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci. 2020; 35(5):e61. PMID: 32030925.
Article4. Lee JY, Hong SW, Hyun M, Park JS, Lee JH, Suh YS, et al. Epidemiological and clinical characteristics of coronavirus disease 2019 in Daegu, South Korea. Int J Infect Dis. 2020; 98:462–466. PMID: 32702415.
Article5. Ministry of Health and Welfare. Confirmed patient status of coronavirus disease 2019 in South Korea. Updated 2021. Accessed April 15, 2017. http://ncov.mohw.go.kr/ .6. Kim SW, Kim SM, Kim YK, Kim JY, Lee YM, Kim BO, et al. Clinical characteristics and outcomes of COVID-19 cohort patients in Daegu metropolitan city outbreak in 2020. J Korean Med Sci. 2021; 36(1):e12. PMID: 33398946.
Article7. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020; 323(13):1239–1242. PMID: 32091533.8. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, Evaluation, and Treatment of Coronavirus (COVID-19). StatPearls. Treasure Island, FL, USA: StatPearls Publishing Copyright;2021.9. Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020; 78:185–193. PMID: 32305533.
Article10. Goodell JW. COVID-19 and finance: agendas for future research. Finance Res Lett. 2020; 35:101512.
Article11. Bruns DP, Kraguljac NV, Bruns TR. COVID-19: Facts, cultural considerations, and risk of stigmatization. J Transcult Nurs. 2020; 31(4):326–332. PMID: 32316872.
Article12. Viner RM, Russell SJ, Croker H, Packer J, Ward J, Stansfield C, et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020; 4(5):397–404. PMID: 32272089.
Article13. Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr. 2020; 14(5):779–788. PMID: 32526627.
Article14. Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2021; 281:91–98. PMID: 33310451.
Article15. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020; 395(10227):912–920. PMID: 32112714.
Article16. Ghosh R, Dubey MJ, Chatterjee S, Dubey S. Impact of COVID -19 on children: special focus on the psychosocial aspect. Minerva Pediatr. 2020; 72(3):226–235. PMID: 32613821.
Article17. Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. 2020; 14(1):20. PMID: 32419840.
Article18. Guessoum SB, Lachal J, Radjack R, Carretier E, Minassian S, Benoit L, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020; 291:113264. PMID: 32622172.
Article19. Wilson N, Turner-Halliday F, Minnis H. Escaping the inescapable: Risk of mental health disorder, somatic symptoms and resilience in Palestinian refugee children. Transcult Psychiatry. 2021; 58(2):307–320. PMID: 33522455.
Article20. Zhao Y, Guo Y, Xiao Y, Zhu R, Sun W, Huang W, et al. The effects of online homeschooling on children, parents, and teachers of grades 1-9 during the COVID-19 pandemic. Med Sci Monit. 2020; 26:e925591. PMID: 32917849.
Article21. Lin MP. Prevalence of internet addiction during the COVID-19 outbreak and its risk factors among junior high school students in Taiwan. Int J Environ Res Public Health. 2020; 17(22):8547.
Article22. Cost KT, Crosbie J, Anagnostou E, Birken CS, Charach A, Monga S, et al. Mostly worse, occasionally better: impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. Eur Child Adolesc Psychiatry. Forthcoming. 2021; DOI: 10.1007/s00787-021-01744-3.
Article23. O'Donohue K, Berger E, McLean L, Carroll M. Psychological outcomes for young adults after disastrous events: a mixed-methods scoping review. Soc Sci Med. 2021; 276:113851. PMID: 33812159.24. Makwana N. Disaster and its impact on mental health: a narrative review. J Family Med Prim Care. 2019; 8(10):3090–3095. PMID: 31742125.
Article25. Newnham EA, Dzidic PL, Mergelsberg EL, Guragain B, Chan EY, Kim Y, et al. The Asia Pacific Disaster Mental Health Network: setting a mental health agenda for the region. Int J Environ Res Public Health. 2020; 17(17):6144.
Article26. Daegu Metropolitan Office of Education. A Report of COVID- 19 Related Student and Teacher Disaster Mental Health Assessment (Publication No. 2020-157). Daegu, Korea: Daegu Metropolitan Office of Education;2021.27. Spitzer RL, Kroenke K, Williams JB, Group PH, Group PH. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999; 282(18):1737–1744. PMID: 10568646.28. Park SJ, Choi HR, Choi JH, Kim KW, Hong JP. Reliability and validity of the Korean version of the Patient Health Questionnaire-9 (PHQ-9). Anxiety Mood. 2010; 6(2):119–124.29. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006; 166(10):1092–1097. PMID: 16717171.30. Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007; 146(5):317–325. PMID: 17339617.
Article31. Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016; 39:24–31. PMID: 26719105.
Article32. Lee SH, Shin C, Kim H, Jeon SW, Yoon HK, Ko YH, et al. Validation of the Korean version of the Generalized Anxiety Disorder 7 self-rating scale. Asia-Pac Psychiatry. Forthcoming. 2020; DOI: 10.1111/appy.12421.
Article33. Shin WY, Kim MG, Kim JH. Developing measures of resilience for Korean adolescents and testing cross, convergent, and discriminant validity. Stud Korean Youth. 2009; 20(4):105–131.34. Bell C, Beaglehole B, Bell R, Tanveer S, Sulaiman-Hill R, Boden J, et al. Learning from previous disasters: potential pitfalls of epidemiological psychosocial research in the COVID-19 environment. Aust N Z J Psychiatry. 2021; 55(7):646–649. PMID: 33645256.
Article35. Alnazly E, Khraisat OM, Al-Bashaireh AM, Bryant CL. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One. 2021; 16(3):e0247679. PMID: 33711026.
Article36. He X, Zhang D, Zhang L, Zheng X, Zhang G, Pan K, et al. Neurological and psychiatric presentations associated with COVID-19. Eur Arch Psychiatry Clin Neurosci. Forthcoming. 2021; DOI: 10.1007/s00406-021-01244-0.
Article37. Fiest KM, Parsons Leigh J, Krewulak KD, Plotnikoff KM, Kemp LG, Ng-Kamstra J, et al. Experiences and management of physician psychological symptoms during infectious disease outbreaks: a rapid review. BMC Psychiatry. 2021; 21(1):91. PMID: 33568141.
Article38. Strudwick G, Sockalingam S, Kassam I, Sequeira L, Bonato S, Youssef A, et al. Digital interventions to support population mental health in Canada during the COVID-19 pandemic: rapid review. JMIR Ment Health. 2021; 8(3):e26550. PMID: 33650985.
Article39. Park C, Hwang JM, Jo S, Bae SJ, Sakong J. COVID-19 outbreak and its association with healthcare workers' emotional stress: a cross-sectional study. J Korean Med Sci. 2020; 35(41):e372. PMID: 33107230.
Article40. Elmer T, Mepham K, Stadtfeld C. Students under lockdown: comparisons of students' social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS One. 2020; 15(7):e0236337. PMID: 32702065.
Article41. Rothe J, Buse J, Uhlmann A, Bluschke A, Roessner V. Changes in emotions and worries during the Covid-19 pandemic: an online-survey with children and adults with and without mental health conditions. Child Adolesc Psychiatry Ment Health. 2021; 15(1):11. PMID: 33612122.
Article42. Gobinath AR, Mahmoud R, Galea LA. Influence of sex and stress exposure across the lifespan on endophenotypes of depression: focus on behavior, glucocorticoids, and hippocampus. Front Neurosci. 2015; 8:420. PMID: 25610363.
Article43. Donner NC, Lowry CA. Sex differences in anxiety and emotional behavior. Pflugers Arch. 2013; 465(5):601–626. PMID: 23588380.
Article44. Esposito S, Giannitto N, Squarcia A, Neglia C, Argentiero A, Minichetti P, et al. Development of psychological problems among adolescents during school closures because of the COVID-19 lockdown phase in Italy: a cross-sectional survey. Front Pediatr. 2021; 8:628072. PMID: 33553079.
Article45. Zhou SJ, Zhang LG, Wang LL, Guo ZC, Wang JQ, Chen JC, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020; 29(6):749–758. PMID: 32363492.
Article46. Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021; 51(2):201–211. PMID: 33436130.
Article47. Lorenzo NE, Zeytinoglu S, Morales S, Listokin J, Almas AN, Degnan KA, et al. Transactional associations between parent and late adolescent internalizing symptoms during the COVID-19 pandemic: the moderating role of avoidant coping. J Youth Adolesc. 2021; 50(3):459–469. PMID: 33495969.
Article48. Chi X, Liang K, Chen ST, Huang Q, Huang L, Yu Q, et al. Mental health problems among Chinese adolescents during the COVID-19: the importance of nutrition and physical activity. Int J Clin Health Psychol. 2021; 21(3):100218. PMID: 33391373.
Article49. Zhou SJ, Wang LL, Yang R, Yang XJ, Zhang LG, Guo ZC, et al. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020; 74:39–47. PMID: 32836185.
Article50. Soest TV, Bakken A, Pedersen W, Sletten MA. Life satisfaction among adolescents before and during the COVID-19 pandemic. Tidsskr Nor Laegeforen. 2020; 140(10):51. Lee YR, Lee JY, Park IH, Kim M, Jhon M, Kim JW, et al. The relationships among media usage regarding COVID-19, knowledge about infection, and anxiety: structural model analysis. J Korean Med Sci. 2020; 35(48):e426. PMID: 33316862.
Article52. Tang S, Xiang M, Cheung T, Xiang YT. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J Affect Disord. 2021; 279:353–360. PMID: 33099049.
Article53. Fountoulakis KN, Apostolidou MK, Atsiova MB, Filippidou AK, Florou AK, Gousiou DS, et al. Self-reported changes in anxiety, depression and suicidality during the COVID-19 lockdown in Greece. J Affect Disord. 2021; 279:624–629. PMID: 33190113.
Article54. Zhang C, Ye M, Fu Y, Yang M, Luo F, Yuan J, et al. The psychological impact of the COVID-19 pandemic on teenagers in China. J Adolesc Health. 2020; 67(6):747–755. PMID: 33041204.
Article55. Zhang X, Zhu W, Kang S, Qiu L, Lu Z, Sun Y. Association between physical activity and mood states of children and adolescents in social isolation during the CoViD-19 epidemic. Int J Environ Res Public Health. 2020; 17(20):7666.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of COVID-19 Pandemic on the Mental Health of the General Public and Children and Adolescents and Supporting Measures
- Impact of the Coronavirus Disease Pandemic on Mental Health Among School Students in Korea During the COVID-19 Pandemic
- Medical students’ professionalism attributes, knowledge, practices, and attitudes toward COVID-19 and attitudes toward care provision during pandemic amidst the COVID-19 outbreak according to their demographics and mental health
- Association of Sociodemographic and Psychosocial Factors With COVID-19–Related Post-Traumatic Stress Disorder Risk Group Among Medical Students
- COVID-19 Pandemic and Pilot Mental Health Care