Clin Endosc.
2021 Nov;54(6):920-923. 10.5946/ce.2020.228.
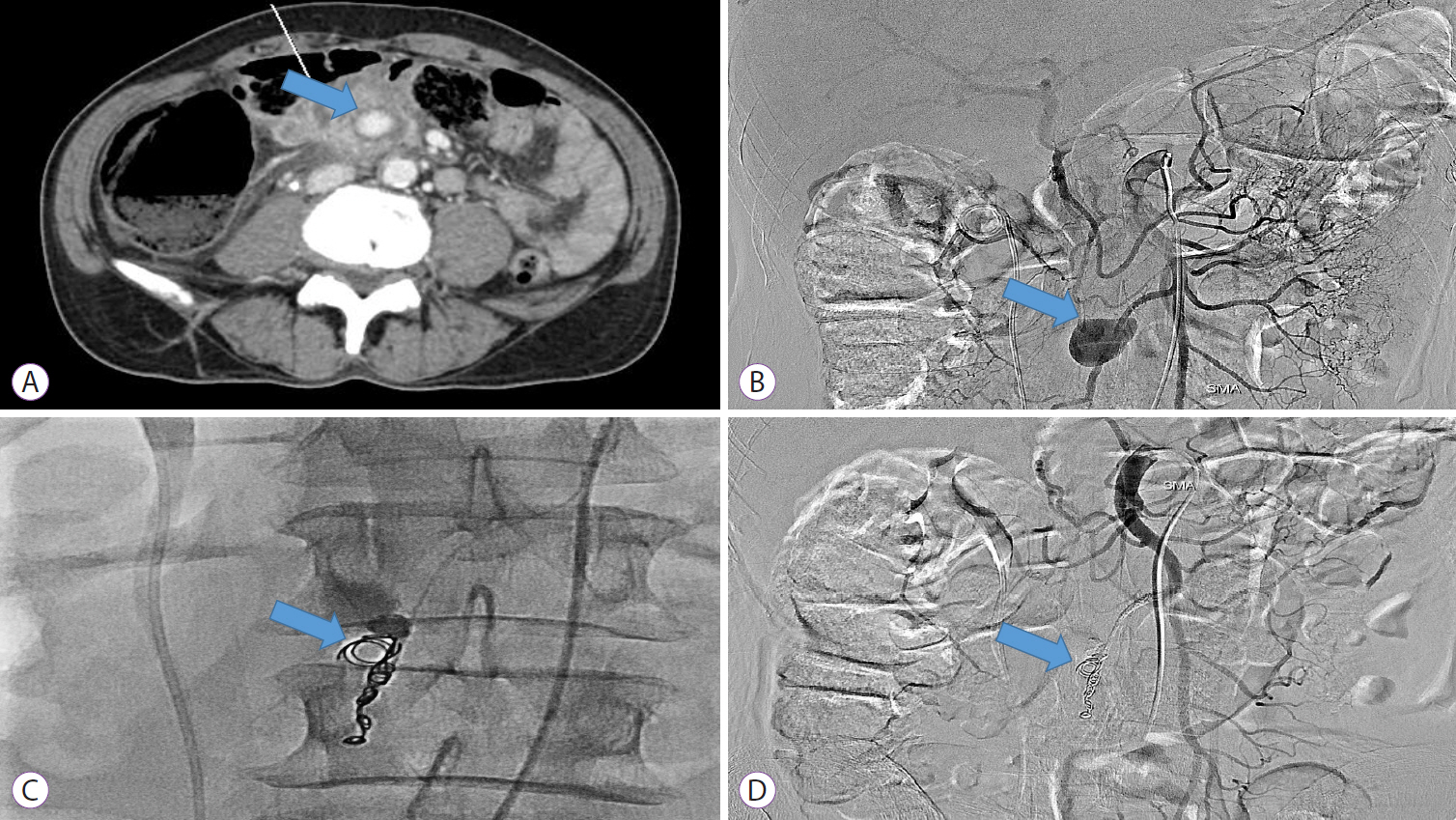
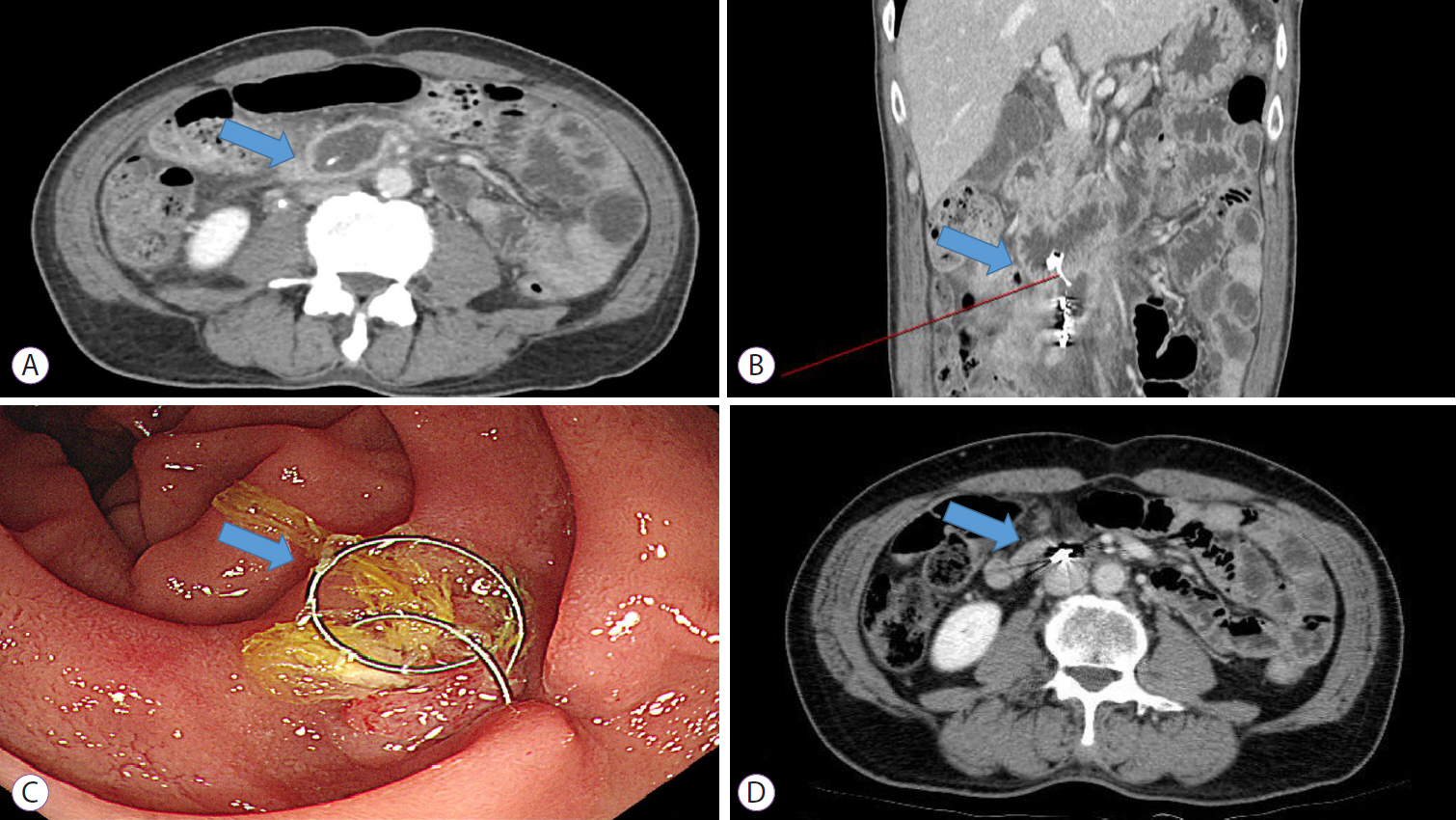
A Rare Case of Coil Migration into the Duodenum after Embolization of a Right Colic Artery Pseudoaneurysm
- Affiliations
-
- 1Department of Internal Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea
- KMID: 2522715
- DOI: http://doi.org/10.5946/ce.2020.228
Abstract
- Transcatheter arterial embolization is a safe and effective treatment for visceral artery aneurysms; nevertheless, some complications can occur. Coil migration to other organs after embolization is extremely rare, and only 16 cases have been reported previously. We report a rare case of coil migration to the duodenal lumen after embolization of a right colic artery pseudoaneurysm. To the best of our knowledge, this is the first case of coil migration after a right colic artery embolization. The patient exhibited no symptoms and was treated conservatively without any intervention. Some previous reports have demonstrated spontaneous coil passage and successful conservative management. Our case supports conservative treatment as the primary treatment for asymptomatic patients. Clinicians should assess the risks and benefits of coil removal in asymptomatic patients before performing any intervention.
Keyword
Figure
Reference
-
1. Pitton MB, Dappa E, Jungmann F, et al. Visceral artery aneurysms: incidence, management, and outcome analysis in a tertiary care center over one decade. Eur Radiol. 2015; 25:2004–2014.
Article2. Barrionuevo P, Malas MB, Nejim B, et al. A systematic review and meta-analysis of the management of visceral artery aneurysms. J Vasc Surg. 2019; 70:1694–1699.
Article3. Matsubara Y, Lim LA, Hijikata Y, Hirata Y, Yotsuyanagi H. Embolization coil migration in the stomach and spontaneous excretion: a case report and review of the literature. Radiol Case Rep. 2020; 15:1018–1022.
Article4. Hewgley WP, Webb DL, Garrett HE Jr. Migrated embolization coil causes intestinal obstruction. J Vasc Surg Cases Innov Tech. 2018; 4:8–11.
Article5. Pratap A, Pokala B, Vargas LM, Oleynikov D, Kothari V. Laparoscopic endoscopic combined surgery for removal of migrated coil after embolization of ruptured splenic artery aneurysm. J Surg Case Rep. 2018; 2018:rjx242.
Article6. Nomura Y, Gotake Y, Okada T, Yamaguchi M, Sugimoto K, Okita Y. Coil migration to the duodenum 1 year following embolisation of a ruptured giant common hepatic artery aneurysm. EJVES Short Rep. 2018; 39:33–36.
Article7. Zaafouri H, Hasnaoui A, Essghaeir S, et al. Ascending cholangitis secondary to migrated embolization coil of gastroduodenal artery pseudo-aneurysm a case report. BMC Surg. 2017; 17:30.
Article8. Han YM, Lee JY, Choi IJ, et al. Endoscopic removal of a migrated coil after embolization of a splenic pseudoaneurysm: a case report. Clin Endosc. 2014; 47:183–187.
Article9. Tekola BD, Arner DM, Behm BW. Coil migration after transarterial coil embolization of a splenic artery pseudoaneurysm. Case Rep Gastroenterol. 2013; 7:487–491.
Article10. Skipworth JR, Morkane C, Raptis DA, et al. Coil migration--a rare complication of endovascular exclusion of visceral artery pseudoaneurysms and aneurysms. Ann R Coll Surg Engl. 2011; 93:e19–e23.11. Kao WY, Chiou YY, Chen TS. Coil migration into the common bile duct after embolization of a hepatic artery pseudoaneurysm. Endoscopy. 2011; 43(Suppl 2):E364–E365.
Article12. Reed A, Suri R, Marcovich R. Passage of embolization coil through urinary collecting system one year after embolization. Urology. 2007; 70:1222.e17–e18.
Article13. Shah NA, Akingboye A, Haldipur N, Mackinlay JY, Jacob G. Embolization coils migrating and being passed per rectum after embolization of a splenic artery pseudoaneurysm, “the migrating coil”: a case report. Cardiovasc Intervent Radiol. 2007; 30:1259–1262.
Article14. Dinter DJ, Rexin M, Kaehler G, Neff W. Fatal coil migration into the stomach 10 years after endovascular celiac aneurysm repair. J Vasc Interv Radiol. 2007; 18(1 Pt 1):117–120.
Article15. Van Steenbergen W, Lecluyse K, Maleux G, Pirenne J. Successful percutaneous cholangioscopic extraction of vascular coils that had eroded into the bile duct after liver transplantation. Endoscopy. 2007; 39(Suppl 1):E210–E211.
Article16. Turaga KK, Amirlak B, Davis RE, Yousef K, Richards A, Fitzgibbons RJ Jr. Cholangitis after coil embolization of an iatrogenic hepatic artery pseudoaneurysm: an unusual case report. Surg Laparosc Endosc Percutan Tech. 2006; 16:36–38.17. Ozkan OS, Walser EM, Akinci D, Nealon W, Goodacre B. Guglielmi detachable coil erosion into the common bile duct after embolization of iatrogenic hepatic artery pseudoaneurysm. J Vasc Interv Radiol. 2002; 13(9 Pt 1):935–938.
Article18. Takahashi T, Shimada K, Kobayashi N, Kakita A. Migration of steelwire coils into the stomach after transcatheter arterial embolization for a bleeding splenic artery pseudoaneurysm: report of a case. Surg Today. 2001; 31:458–462.
Article19. Xu H, Jing C, Zhou J, et al. Clinical efficacy of coil embolization in treating pseudoaneurysm post-whipple operation. Exp Ther Med. 2020; 20:37.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Removal of a Migrated Coil after Embolization of a Splenic Pseudoaneurysm: A Case Report
- Endovascular Thrombin Injection for a Pulmonary Artery Pseudoaneurysm: Case Report
- Coil Embolization of a Pseudoaneurysm of the Anterior Tibial Artery: A Case Report
- Jejunal Migration of the Stent-Graft Used for Common Hepatic Artery Pseudoaneurysm
- Successfully treated isolated renal artery pseudoaneurysm in a patient with Behçet's disease