Clin Endosc.
2021 Nov;54(6):864-871. 10.5946/ce.2021.004.
The Additive Effect of Platelet-Rich Plasma in the Treatment of Actively Bleeding Peptic Ulcer
- Affiliations
-
- 1Division of Hepatogastroenterology and Endoscopy, Zagazig University, Zagazig, Egypt
- KMID: 2522707
- DOI: http://doi.org/10.5946/ce.2021.004
Abstract
- Background/Aims
Peptic ulcer bleeding is the most common cause of upper gastrointestinal tract bleeding. Platelet-rich plasma (PRP) enhances tissue repair, and is therefore used in various medical treatments. A combination of mechanical or electrothermal hemostasis has been recommended for upper gastrointestinal tract bleeding treatment. This study evaluated the additive efficacy of PRP in bleeding peptic ulcer hemostasis and recovery.
Methods
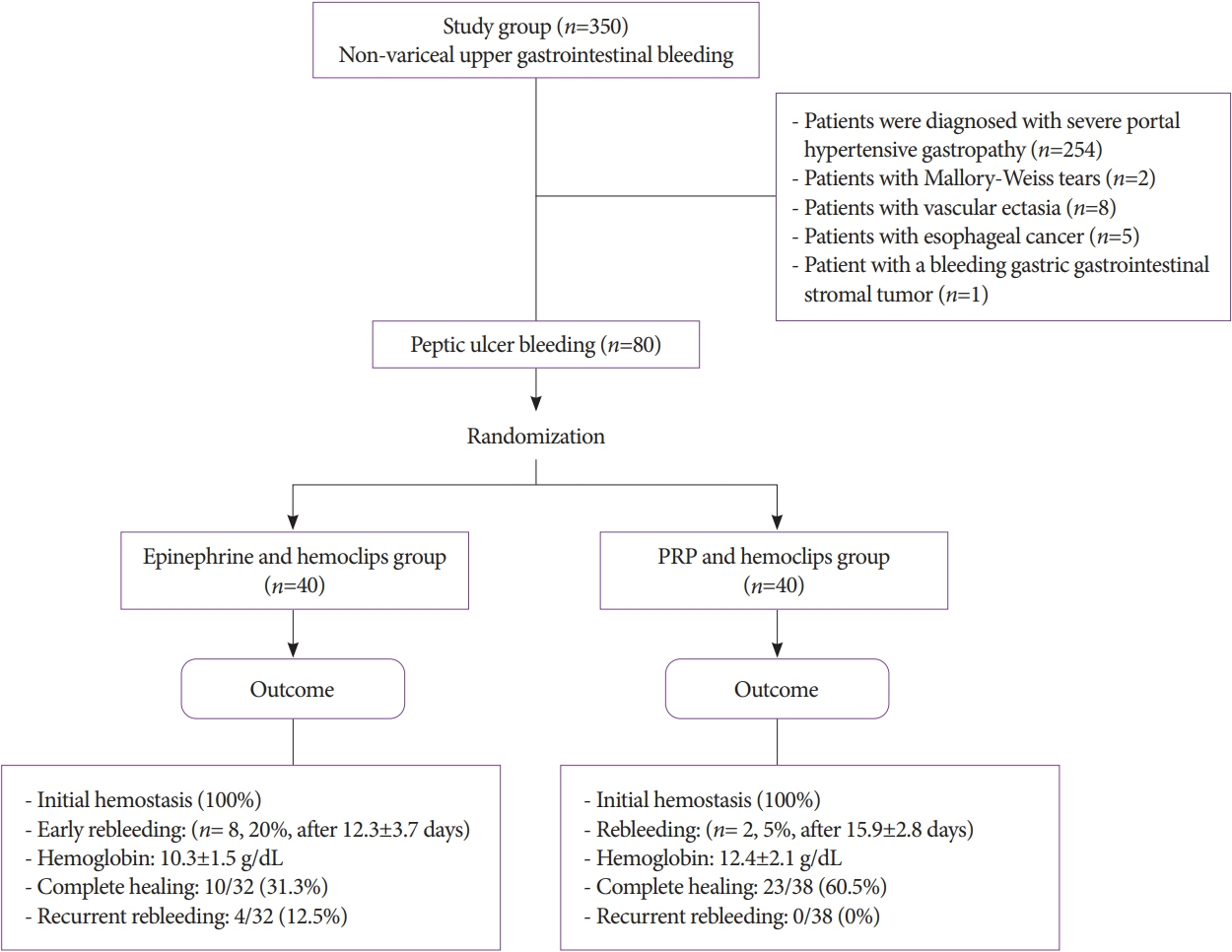
Eighty patients with peptic ulcer bleeding were initially treated by hemoclipping, and were randomly chosen for either additional PRP (n=40) or additional epinephrine (n=40) injections. Both groups were compared with regard to achieving hemostasis and the frequency of complications.
Results
Hemostasis was immediately achieved in both groups. Two patients (5%) in the PRP group and 8 (20%) patients in the epinephrine group experienced rebleeding after 15.9±2.8 and 12.3±3.7 days, respectively. They were managed by PRP injection in addition to proton pump inhibitor infusion. Hemoglobin was substantially increased in the PRP-treated group with full recovery occurring in 60.5% compared to 31.3% of patients in the epinephrine group (p=0.001). There was no recurrent bleeding in the PRP group, but 4/32 (12.5%) patients in the epinephrine group exhibited rebleeding.
Conclusions
PRP showed additional benefit in reducing peptic ulcer bleeding with no reported significant complications. Clinical trial (NCT03733171).
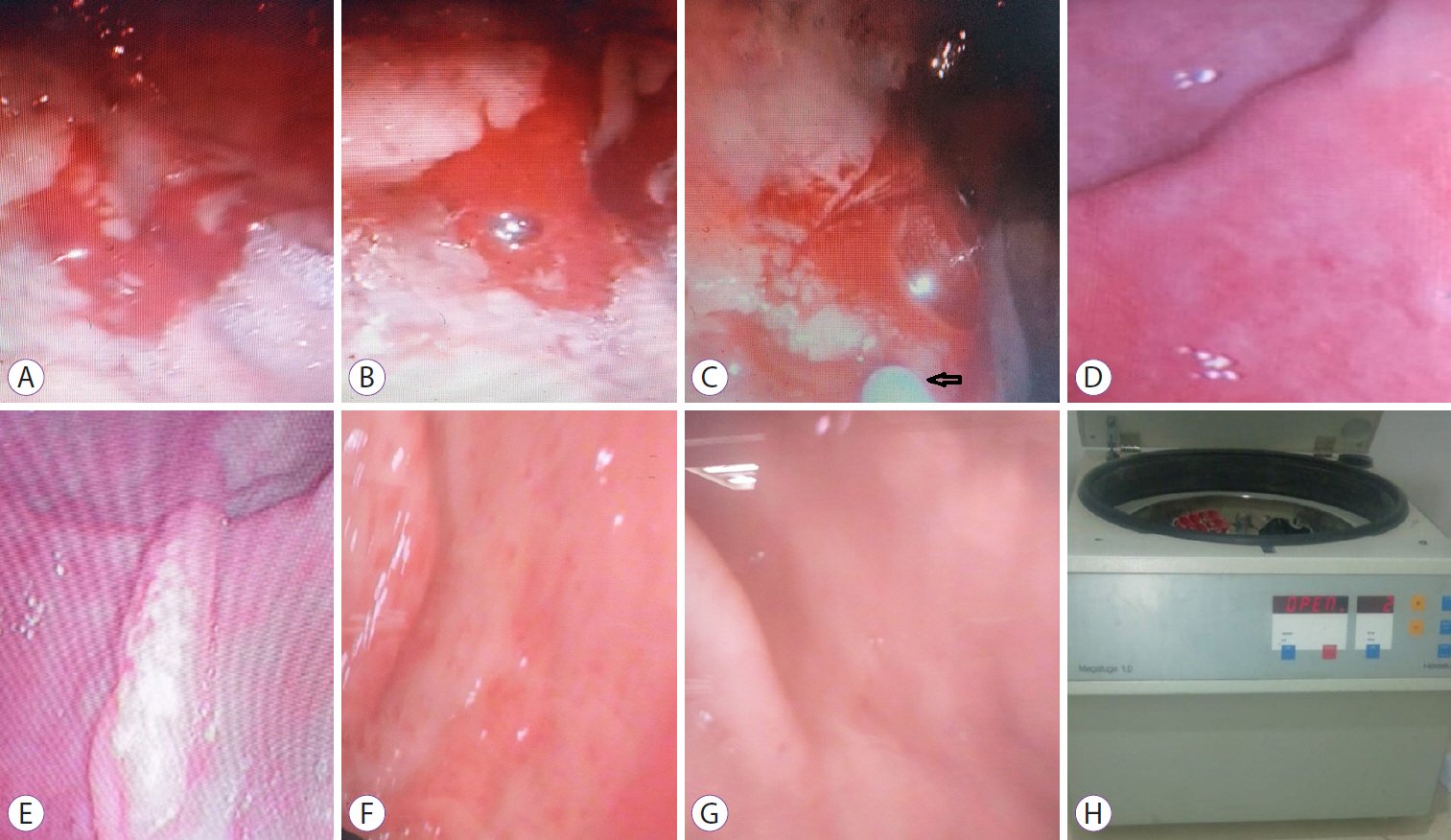
Figure
Reference
-
1. Jacques J, Legros R, Chaussade S, Sautereau D. Endoscopic haemostasis: an overview of procedures and clinical scenarios. Dig Liver Dis. 2014; 46:766–776.
Article2. Everts PA, Knape JT, Weibrich G, et al. Platelet-rich plasma and platelet gel: a review. J Extra Corpor Technol. 2006; 38:174–187.3. Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004; 62:489–496.
Article4. Valeri CR, Saleem B, Ragno G. Release of platelet-derived growth factors and proliferation of fibroblasts in the releasates from platelets stored in the liquid state at 22 degrees C after stimulation with agonists. Transfusion. 2006; 46:225–229.5. Sunitha Raja V, Munirathnam Naidu E. Platelet-rich fibrin: evolution of a second-generation platelet concentrate. Indian J Dent Res. 2008; 19:42–46.
Article6. Antoniades HN, Williams LT. Human platelet-derived growth factor: structure and function. Fed Proc. 1983; 42:2630–2634.7. Lindeboom JA, Mathura KR, Aartman IH, Kroon FH, Milstein DM, Ince C. Influence of the application of platelet-enriched plasma in oral mucosal wound healing. Clin Oral Implants Res. 2007; 18:133–139.
Article8. Ramos-Torrecillas J, De Luna-Bertos E, García-Martínez O, Díaz-Rodríguez L, Ruiz C. Use of platelet-rich plasma to treat pressure ulcers: a case study. J Wound Ostomy Continence Nurs. 2013; 40:198–202.9. Wrotniak M, Bielecki T, Gaździk TS. Current opinion about using the platelet-rich gel in orthopaedics and trauma surgery. Ortop Traumatol Rehabil. 2007; 9:227–238.10. Yol S, Tekin A, Yilmaz H, et al. Effects of platelet rich plasma on colonic anastomosis. J Surg Res. 2008; 146:190–194.
Article11. Pallua N, Wolter T, Markowicz M. Platelet-rich plasma in burns. Burns. 2010; 36:4–8.
Article12. Barkun AN, Bardou M, Kuipers EJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010; 152:101–113.
Article13. Forrest JA, Finlayson ND, Shearman DJ. Endoscopy in gastrointestinal bleeding. Lancet. 1974; 2:394–397.
Article14. Konstantinidis A, Valatas V, Ntelis V, et al. Endoscopic treatment for high-risk bleeding peptic ulcers: a comparison of epinephrine alone with epinephrine plus ethanolamine. Ann Gastroenterol. 2011; 24:101–107.15. Kovacs TO. Management of upper gastrointestinal bleeding. Curr Gastroenterol Rep. 2008; 10:535–542.
Article16. Aabakken L. Current endoscopic and pharmacological therapy of peptic ulcer bleeding. Best Pract Res Clin Gastroenterol. 2008; 22:243–259.
Article17. Chau CH, Siu WT, Law BK, et al. Randomized controlled trial comparing epinephrine injection plus heat probe coagulation versus epinephrine injection plus argon plasma coagulation for bleeding peptic ulcers. Gastrointest Endosc. 2003; 57:455–461.
Article18. van Leerdam ME. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008; 22:209–224.
Article19. Hearnshaw SA, Logan RF, Lowe D, Travis SP, Murphy MF, Palmer KR. Acute upper gastrointestinal bleeding in the UK: patient characteristics, diagnoses and outcomes in the 2007 UK audit. Gut. 2011; 60:1327–1335.
Article20. Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012; 107:345–360. quiz 361.
Article21. Szura M, Pasternak A. Upper non-variceal gastrointestinal bleeding - review the effectiveness of endoscopic hemostasis methods. World J Gastrointest Endosc. 2015; 7:1088–1095.
Article22. Gralnek IM, Dumonceau JM, Kuipers EJ, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2015; 47:a1–a46.
Article23. Schmidt A, Gölder S, Goetz M, et al. Over-the-scope clips are more effective than standard endoscopic therapy for patients with recurrent bleeding of peptic ulcers. Gastroenterology. 2018; 155:674–686.e6.
Article24. Barkun A. Hemostatic powder TC-325. Gastroenterol Hepatol (NY). 2015; 11:489–491.25. Prei JC, Barmeyer C, Bürgel N, et al. EndoClot polysaccharide hemostatic system in nonvariceal gastrointestinal bleeding: results of a prospective multicenter observational pilot study. J Clin Gastroenterol. 2016; 50:e95–e100.26. Kurt M, Onal I, Akdogan M, et al. Ankaferd blood stopper for controlling gastrointestinal bleeding due to distinct benign lesions refractory to conventional antihemorrhagic measures. Can J Gastroenterol. 2010; 24:380–384.
Article27. Smith PA. Intra-articular autologous conditioned plasma injections provide safe and efficacious treatment for knee osteoarthritis: an FDA-sanctioned, randomized, double-blind, placebo-controlled clinical trial. Am J Sports Med. 2016; 44:884–891.28. de la Portilla F, Segura-Sampedro JJ, Reyes-Díaz ML, et al. Treatment of transsphincteric fistula-in-ano with growth factors from autologous platelets: results of a phase II clinical trial. Int J Colorectal Dis. 2017; 32:1545–1550.
Article29. Long DW, Johnson NR, Jeffries EM, Hara H, Wang Y. Controlled delivery of platelet-derived proteins enhances porcine wound healing. J Control Release. 2017; 253:73–81.
Article30. Dijkstra-Tiekstra MJ, van der Schoot CE, Pietersz RN, Reesink HW. White blood cell fragments in platelet concentrates prepared by the platelet-rich plasma or buffy-coat methods. Vox Sang. 2005; 88:275–277.
Article31. Adler SC, Kent KJ. Enhancing wound healing with growth factors. Facial Plast Surg Clin North Am. 2002; 10:129–146.
Article32. Jeong E, Yoo IK, Cakir OO, et al. Effectiveness of autologous platelet-rich plasma for the healing of ulcers after endoscopic submucosal dissection. Clin Endosc. 2019; 52:472–478.
Article33. Jensen DM, Eklund S, Persson T, et al. Reassessment of rebleeding risk of Forrest IB (Oozing) peptic ulcer bleeding in a large international randomized trial. Am J Gastroenterol. 2017; 112:441–446.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Management of Peptic Ulcer Bleeding
- The Effect of Helicobacter pylori Infection on Peptic Ulcer Bleeding
- The Effects of Endoscopic Sodium Alginate Powder (Alto Shooter(TM)) in Peptic Ulcer Bleeding
- Management of Peptic Ulcer Bleeding in Patients Taking Aspirin or Anticoagulant
- Effect of Platelet-rich Plasma on Burn Wounds according to Time of Application: An Experimental Study on Rats