Clin Endosc.
2021 Nov;54(6):833-842. 10.5946/ce.2021.052.
Stent versus Balloon Dilation for the Treatment of Dominant Strictures in Primary Sclerosing Cholangitis: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Gastrointestinal Endoscopy Unity, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo – HC/FMUSP, São Paulo, SP, Brazil
- 2Division of Gasteoenterology, Hepatology and Endoscopy – Brigham and Women’s Hospital – Harvard Medical School, Boston, MA, USA
- KMID: 2522703
- DOI: http://doi.org/10.5946/ce.2021.052
Abstract
- Background/Aims
The endoscopic management of primary sclerosing cholangitis (PSC)-associated dominant strictures remains challenging. This systematic review and meta-analysis aimed to compare balloon dilation and stent placement in the treatment of dominant strictures among PSC patients.
Methods
Literature searches on MEDLINE, EMBASE, Cochrane CENTRAL and Lilacs/Bireme were performed for studies published until December 2020. Measured outcomes included clinical efficacy, stricture recurrence, cumulative recurrencefree rate, transplant rate, 5-year survival rate, and adverse events (i.e., pancreatitis, cholangitis, bleeding, perforation and death).
Results
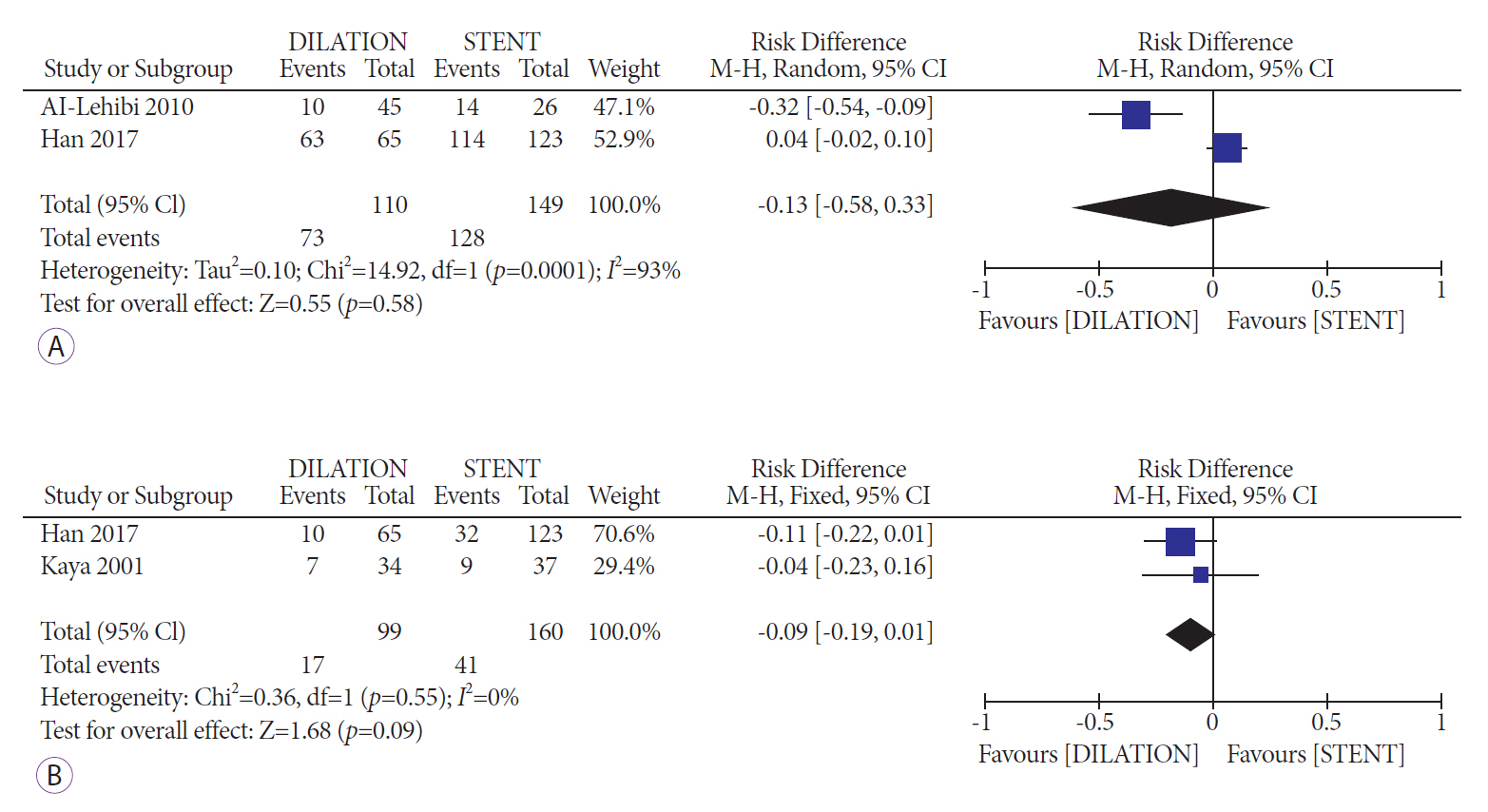
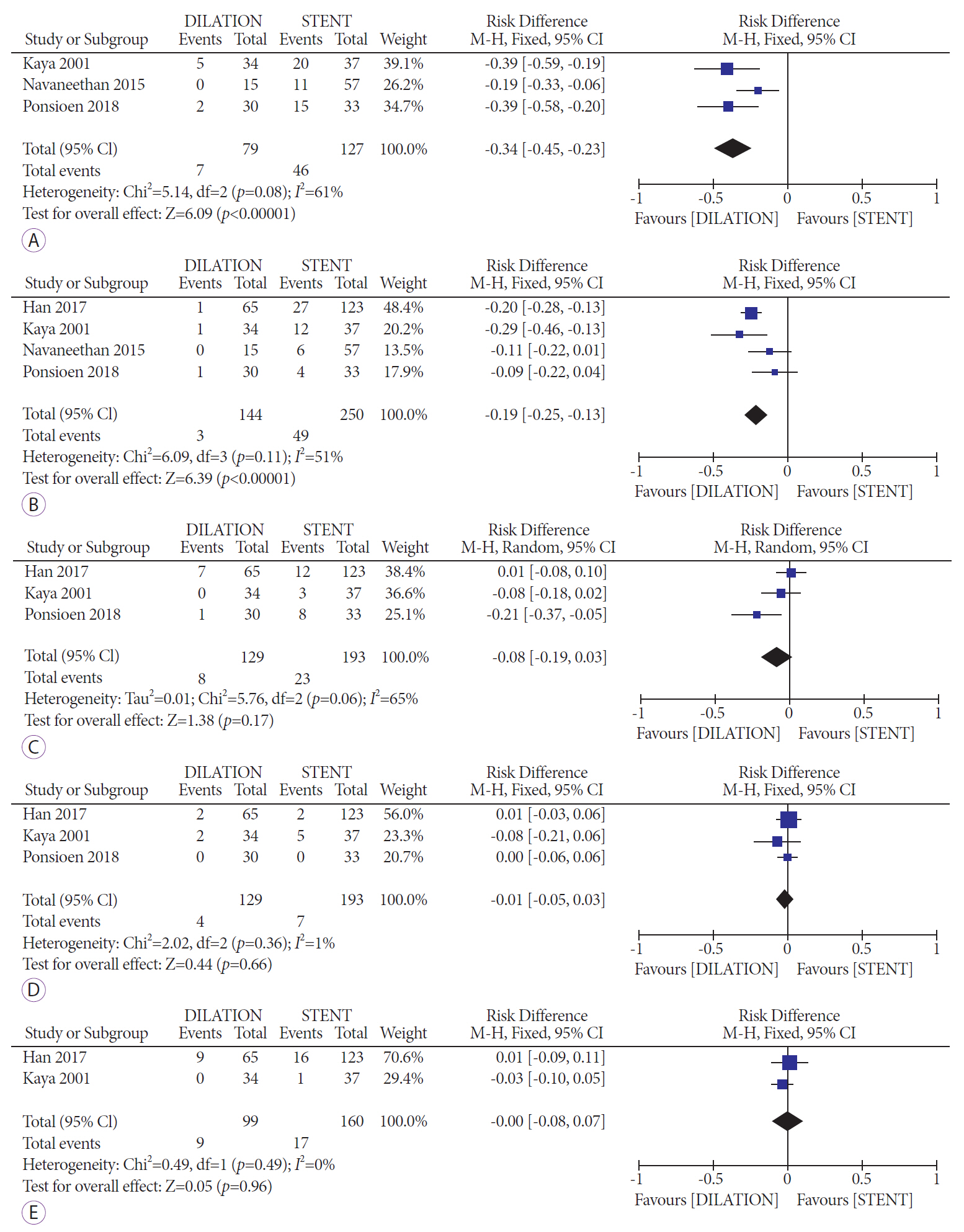
A total of 5 studies (n=467) were included. Based on pooled analyses, there were no differences in clinical efficacy (risk difference [RD], -0.13; 95% confidence interval [CI], -0.58 to 0.33; I2=93%) or transplant rates (RD, -0.09; 95% CI, -0.19 to 0.01; I2=0%); however, the risk of occurrence of adverse events was lower with balloon dilatation than with stent placement (RD,-0.34; 95% CI, -0.45 to -0.23; I2=61%). Among the types of adverse events reported, only the rates of cholangitis/bacteremia were significantly lower in balloon dilation patients (RD, -0.19; 95% CI, -0.25 to -0.13; I2=51%).
Conclusions
Compared to balloon dilation, stent placement for dominant strictures in PSC appeared to have higher complication rates without significant differences in efficacy.
Figure
Cited by 1 articles
-
Treatment of primary sclerosing cholangitis combined with inflammatory bowel disease
You Sun Kim, Edward H. Hurley, Yoojeong Park, Sungjin Ko
Intest Res. 2023;21(4):420-432. doi: 10.5217/ir.2023.00039.
Reference
-
1. Lee YM, Kaplan MM. Primary sclerosing cholangitis. N Engl J Med. 1995; 332:924–933.
Article2. Angulo P, Lindor KD. Primary sclerosing cholangitis. Hepatology. 1999; 30:325–332.
Article3. Njei B, McCarty TR, Varadarajulu S, Navaneethan U. Systematic review with meta-analysis: endoscopic retrograde cholangiopancreatography-based modalities for the diagnosis of cholangiocarcinoma in primary sclerosing cholangitis. Aliment Pharmacol Ther. 2016; 44:1139–1151.
Article4. Tabibian JH, Baron TH. Endoscopic management of primary sclerosing cholangitis. Expert Rev Gastroenterol Hepatol. 2018; 12:693–703.
Article5. Broomé U, Olsson R, Lööf L, et al. Natural history and prognostic factors in 305 Swedish patients with primary sclerosing cholangitis. Gut. 1996; 38:610–615.
Article6. Sclair SN, Little E, Levy C. Current concepts in primary biliary cirrhosis and primary sclerosing cholangitis. Clin Transl Gastroenterol. 2015; 6:e109.
Article7. Sedki M, Levy C. Update in the care and management of patients with primary sclerosing cholangitis. Curr Gastroenterol Rep. 2018; 20:29.
Article8. Karlsen TH, Folseraas T, Thorburn D, Vesterhus M. Primary sclerosing cholangitis-a comprehensive review. J Hepatol. 2017; 67:1298–1323.9. Weismüller TJ, Trivedi PJ, Bergquist A, et al. Patient age, sex, and inflammatory bowel disease phenotype associate with course of primary sclerosing cholangitis. Gastroenterology. 2017; 152:1975–1984.e8.10. de Moura DTH, Ryou M, de Moura EGH, Ribeiro IB, Bernardo WM, Thompson CC. Endoscopic ultrasound-guided fine needle aspiration and endoscopic retrograde cholangiopancreatography-based tissue sampling in suspected malignant biliary strictures: a meta-analysis of same-session procedures. Clin Endosc. 2020; 53:417–428.
Article11. Abu-Wasel B, Keough V, Renfrew PD, Molinari M. Biliary stent therapy for dominant strictures in patients affected by primary sclerosing cholangitis. Pathobiology. 2013; 80:182–193.
Article12. Moura DTH, de Moura EGH, Matuguma SE, et al. EUS-FNA versus ERCP for tissue diagnosis of suspect malignant biliary strictures: a prospective comparative study. Endosc Int Open. 2018; 6:E769–E777.
Article13. de Oliveira PVAG, de Moura DTH, Ribeiro IB, et al. Efficacy of digital single-operator cholangioscopy in the visual interpretation of indeterminate biliary strictures: a systematic review and meta-analysis. Surg Endosc. 2020; 34:3321–3329.
Article14. Delgado AA de A, de Moura DTH, Ribeiro IB, et al. Propofol vs traditional sedatives for sedation in endoscopy: a systematic review and meta-analysis. World J Gastrointest Endosc. 2019; 11:573–588.15. Matsubayashi CO, Ribeiro IB, de Moura DTH, et al. Is endoscopic balloon dilation still associated with higher rates of pancreatitis?: a systematic review and meta-analysis. Pancreas. 2020; 49:158–174.16. Funari MP, Ribeiro IB, de Moura DTH, et al. Adverse events after biliary sphincterotomy: does the electric current mode make a difference? a systematic review and meta-analysis of randomized controlled trials. Clin Res Hepatol Gastroenterol. 2020; 44:739–752.
Article17. Passos ML, Ribeiro IB, de Moura DTH, et al. Efficacy and safety of carbon dioxide insufflation versus air insufflation during endoscopic retrograde cholangiopancreatography in randomized controlled trials: a systematic review and meta-analysis. Endosc Int Open. 2019; 7:E487–E497.
Article18. Serrano JPR, de Moura DTH, Bernardo WM, et al. Nonsteroidal anti-inflammatory drugs versus placebo for post-endoscopic retrograde cholangiopancreatography pancreatitis: a systematic review and meta-analysis. Endosc Int Open. 2019; 7:E477–E486.
Article19. European Society of Gastrointestinal Endoscopy; European Association for the Study of the Liver. Role of endoscopy in primary sclerosing cholangitis: european society of gastrointestinal endoscopy (ESGE) and european association for the study of the liver (EASL) clinical guideline. J Hepatol. 2017; 66:1265–1281.20. Chapman MH, Thorburn D, Hirschfield GM, et al. British society of gastroenterology and UK-PSC guidelines for the diagnosis and management of primary sclerosing cholangitis. Gut. 2019; 68:1356–1378.
Article21. Logiudice FP, Bernardo WM, Galetti F, et al. Endoscopic ultrasound-guided vs endoscopic retrograde cholangiopancreatography biliary drainage for obstructed distal malignant biliary strictures: a systematic review and meta-analysis. World J Gastrointest Endosc. 2019; 11:281–291.
Article22. Parsi MA. Common controversies in management of biliary strictures. World J Gastroenterol. 2017; 23:1119–1124.
Article23. Modha K, Navaneethan U. Diagnosis and management of primary sclerosing cholangitis-perspectives from a therapeutic endoscopist. World J Hepatol. 2015; 7:799–805.
Article24. Ponsioen CY, Arnelo U, Bergquist A, et al. No superiority of stents vs balloon dilatation for dominant strictures in patients with primary sclerosing cholangitis. Gastroenterology. 2018; 155:752–759.e5.
Article25. Costamagna G, Boškoski I. Current treatment of benign biliary strictures. Ann Gastroenterol. 2013; 26:37–40.26. De Moura DTH, Moura EGHD, Bernardo WM, et al. Endoscopic retrograde cholangiopancreatography versus endoscopic ultrasound for tissue diagnosis of malignant biliary stricture: systematic review and meta-analysis. Endosc Ultrasound. 2018; 7:10–19.
Article27. Visconti TA de C, Bernardo WM, Moura DTH, et al. Metallic vs plastic stents to treat biliary stricture after liver transplantation: a systematic review and meta-analysis based on randomized trials. Endosc Int Open. 2018; 6:E914–E923.
Article28. Ferreira R, Loureiro R, Nunes N, et al. Role of endoscopic retrograde cholangiopancreatography in the management of benign biliary strictures: what’s new? World J Gastrointest Endosc. 2016; 8:220–231.
Article29. Kaya M, Petersen BT, Angulo P, et al. Balloon dilation compared to stenting of dominant strictures in primary sclerosing cholangitis. Am J Gastroenterol. 2001; 96:1059–1066.
Article30. Baron TH, Davee T. Endoscopic management of benign bile duct strictures. Gastrointest Endosc Clin N Am. 2013; 23:295–311.
Article31. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015; 4:1.
Article32. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019; 366:l4898.
Article33. Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016; 355:i4919.
Article34. Morgan RL, Florez I, Falavigna M, et al. Development of rapid guidelines: 3. GIN-Mcmaster guideline development checklist extension for rapid recommendations. Health Res Policy Syst. 2018; 16:63.
Article35. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005; 5:13.
Article36. Navaneethan U, Jegadeesan R, Hammel J, Sanaka MR, Vargo JJ, Parsi MA. Su1646 endoscopic treatment of dominant biliary strictures in primary sclerosing cholangitis patients: comparison of adverse events associated with balloon dilation with and without stenting. Gastrointestinal Endoscopy. 2015; 81:AB364.
Article37. Al-Lehibi AH, Kumar N, Ammar T, et al. T1572: experience with endoscopic therapy in patients with primary sclerosing cholangitis. Gastrointestinal Endoscopy. 2010; 71:AB312.
Article38. Han S, Xu A, Shah RJ. Tu1435 ERCP with balloon dilation alone or balloon dilation with stenting for dominant strictures in patients with primary sclerosing cholangitis. Gastrointestinal Endoscopy. 2017; 85:AB625–AB626.
Article39. Njei B, McCarty TR, Varadarajulu S, Navaneethan U. Cost utility of ERCP-based modalities for the diagnosis of cholangiocarcinoma in primary sclerosing cholangitis. Gastrointestinal Endoscopy. 2017; 85:773–781.e10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A novel clinical trial for primary sclerosing cholangitis from Asia: All regional endeavors should improve global management of primary sclerosing cholangitis: Editorial on “Safety and efficacy of HK-660S in patients with primary sclerosing cholangitis: A randomized double-blind phase 2a trial”
- Biliary Tract & Pancreas; A Case of Cholangiocarcinoma Suggested as Developing in the Patient with Primary Sclerosing Cholangitis
- Endoscopic Diagnosis and Treatment of Benign Biliary Strictures
- Use of a Cutting Balloon Dilation as a Rescue Therapy in Patients with Benign Bilioenteric Anastomotic Strictures Refractory to Conventional Balloon Dilation
- Role of Endoscopy in Primary Sclerosing Cholangitis