Healthc Inform Res.
2021 Oct;27(4):315-324. 10.4258/hir.2021.27.4.315.
Stakeholders’ Perceptions of the Implementation of a Patient-Centric Digital Health Application for Primary Healthcare in India
- Affiliations
-
- 1Department of Community Medicine and School of Public Health, Postgraduate Institute of Medical Education and Research, Chandigarh, India
- 2Department of Informatics, University of Oslo, Oslo, Norway
- KMID: 2522213
- DOI: http://doi.org/10.4258/hir.2021.27.4.315
Abstract
Objectives
Health systems are shifting from traditional methods of healthcare delivery to delivery using digital applications. This change was introduced at a primary care centre in Chandigarh, India that served a marginalised population. After establishing the digital health system, we explored stakeholders’ perceptions regarding its implementation.
Methods
Ethnographic methods were used to explore stakeholders’ perceptions regarding the implementation of the Integrated Health Information System for Primary Health Care (IHIS4PHC), which was developed as a patient-centric digital health application. Data were collected using focus group discussions and in-depth interviews. Participatory observations were made of day-to-day activities including outpatient visits, outreach field visits, and methods of health practice. The collected information was analysed using thematic coding.
Results
Healthcare workers highlighted that working with the digital health system was initially arduous, but they later realised its usefulness, as the digital system made it easier to search records and generate reports, rapidly providing evidence to make decisions. Auxiliary nurse midwives reported that recording information on computers saved time when generating reports; however, systematic and mandatory data entry made recording tedious. Staff were apprehensive about the use of computer-based data for monitoring their work performance. Patients appreciated that their previous records were now available on the computer for easy retrieval.
Conclusions
The usefulness of the digital health application was appreciated by various primary healthcare stakeholders. Barriers persisted due to perceived needs for flexibility in delivering healthcare services, and apprehensions continued because of increased transparency, accountability, and dependence on computers and digital technicians.
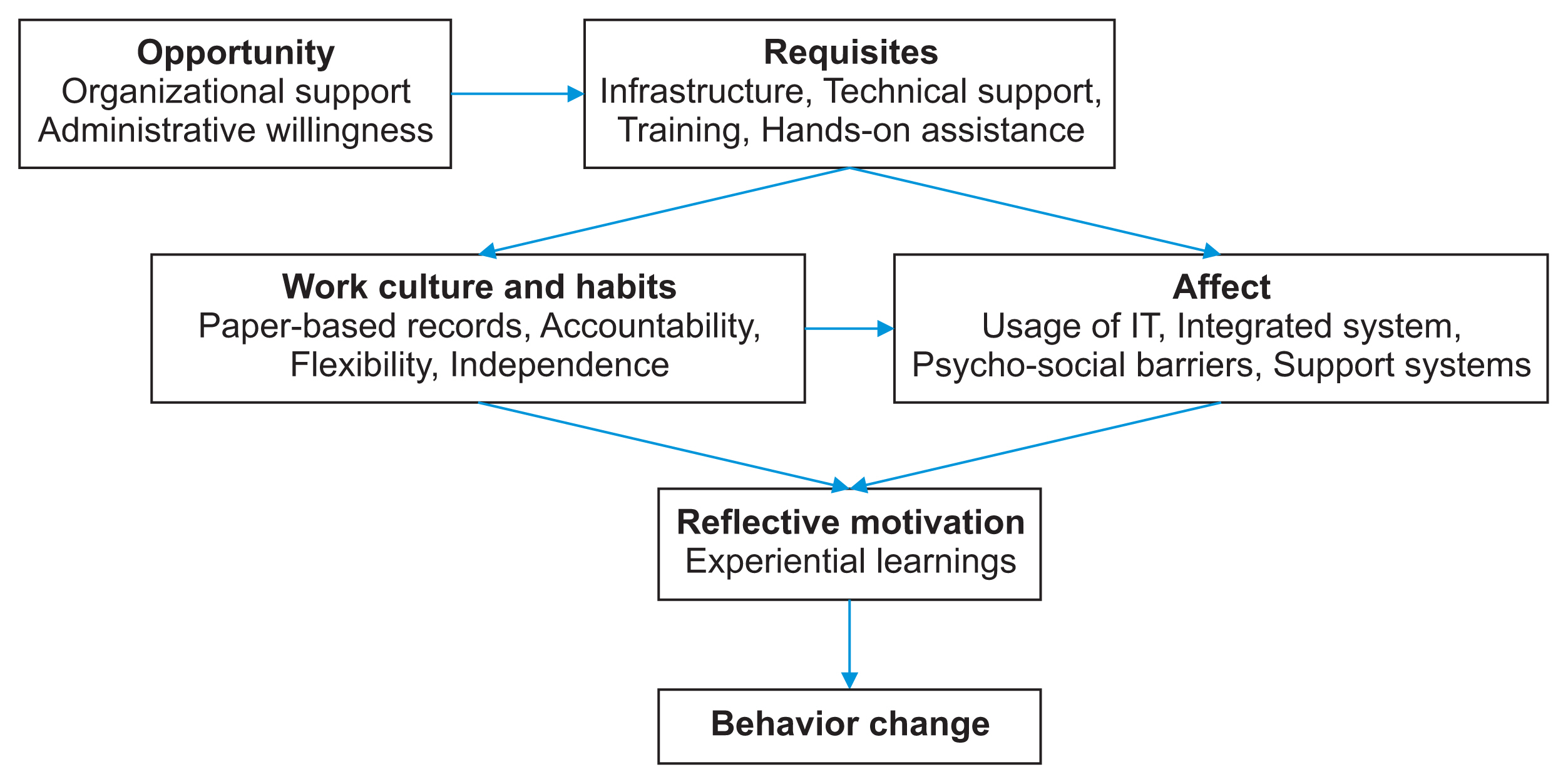
Figure
Reference
-
References
1. Flatley Brennan P, Kuang YS, Volrathongchai K. Patient-centered Information Systems. Yearb Med Inform. 2000; (1):79–86.
Article2. Kotze P, Foster R. A conceptual data model for a primary health care patient-centric electronic medical record system [Internet]. Calgary, Canada: ACTA Press;2014. [cited at 2021 Sep 30]. Available from: https://doi.org/10.2316/p.2014.815-010 .
Article3. Berwick DM. What ‘patient-centered’ should mean: confessions of an extremist. Health Aff (Millwood). 2009; 28(4):w555–65.
Article4. Faujdar DS, Sahay S, Singh T, Jindal H, Kumar R. Public health information systems for primary health care in India: a situational analysis study. J Family Med Prim Care. 2019; 8(11):3640–6.
Article5. Tripathi S, Sharma R, Nagarajan S. Health information systems in India: challenges and way forward [Internet]. Munich, Germany: Munich Personal RePEc Archive (MPRA);2018. [cited at 2021 Sep 30]. Available from: https://mpra.ub.uni-muenchen.de/87067/ .6. Ndabarora E, Chipps JA, Uys L. Systematic review of health data quality management and best practices at community and district levels in LMIC. Inf Dev. 2014; 30(2):103–20.
Article7. Singh T, Roy P, Jamir L, Gupta S, Kaur N, Jain DK, et al. Assessment of universal healthcare coverage in a district of North India: a rapid cross-sectional survey using tablet computers. PLoS One. 2016; 11(6):e0157831.
Article8. Barello S, Triberti S, Graffigna G, Libreri C, Serino S, Hibbard J, et al. eHealth for patient engagement: a systematic review. Front Psychol. 2016; 6:2013.
Article9. Sequist TD, Cullen T, Hays H, Taualii MM, Simon SR, Bates DW. Implementation and use of an electronic health record within the Indian Health Service. J Am Med Inform Assoc. 2007; 14(2):191–7.
Article10. Mannan R, Murphy J, Jones M. Is primary care ready to embrace e-health? A qualitative study of staff in a London primary care trust. Inform Prim Care. 2006; 14(2):121–31.
Article11. Granja C, Janssen W, Johansen MA. Factors determining the success and failure of eHealth interventions: systematic review of the literature. J Med Internet Res. 2018; 20(5):e10235.
Article12. Li J, Talaei-Khoei A, Seale H, Ray P, Macintyre CR. Health care provider adoption of eHealth: systematic literature review. Interact J Med Res. 2013; 2(1):e7.
Article13. Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Q. 2003; 27(3):425–78.
Article14. Faujdar DS, Sahay S, Singh T, Kaur M, Kumar R. Field testing of a digital health information system for primary health care: a quasi-experimental study from India. Int J Med Inform. 2020; 141:104235.
Article15. Lilford RJ, Foster J, Pringle M. Evaluating eHealth: how to make evaluation more methodologically robust. PLoS Med. 2009; 6(11):e1000186.
Article16. Pawson R, Tilley N. Realist evaluation [Internet]. London, UK: Sage;2004. [cited at 2021 Sep 30]. Available from: http://www.communitymatters.com.au/RE_chapter.pdf .17. Gagnon MP, Legare F, Fortin JP, Lamothe L, Labrecque M, Duplantie J. An integrated strategy of knowledge application for optimal e-health implementation: a multi-method study protocol. BMC Med Inform Decis Mak. 2008; 8:17.
Article18. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011; 6:42.
Article19. Foley G, Timonen V. Using grounded theory method to capture and analyze health care experiences. Health Serv Res. 2015; 50(4):1195–210.
Article20. Adane K, Muluye D, Abebe M. Processing medical data: a systematic review. Arch Public Health. 2013; 71(1):27.
Article21. Talboom-Kamp EP, Verdijk NA, Harmans LM, Numans ME, Chavannes NH. An eHealth platform to manage chronic disease in primary care: an innovative approach. Interact J Med Res. 2016; 5(1):e5.
Article22. Peters DH, Kohli M, Mascarenhas M, Rao K. Can computers improve patient care by primary health care workers in India? Int J Qual Health Care. 2006; 18(6):437–45.
Article23. Runz-Jorgensen SM, Schiotz ML, Christensen U. Perceived value of eHealth among people living with multimorbidity: a qualitative study. J Comorb. 2017; 7(1):96–111.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preparing for a New World: Making Friends with Digital Health
- Digital Healthcare Centered on Chronobiology
- Lessons from Use of Continuous Glucose Monitoring Systems in Digital Healthcare
- Adoption of Electronic Health Records: A Roadmap for India
- Evaluation Framework for Telemedicine Using the Logical Framework Approach and a Fishbone Diagram