Healthc Inform Res.
2021 Oct;27(4):307-314. 10.4258/hir.2021.27.4.307.
Predicting Hospital Readmission in Heart Failure Patients in Iran: A Comparison of Various Machine Learning Methods
- Affiliations
-
- 1Department of Biostatistics, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
- 2Modeling of Noncommunicable Diseases Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
- 3Department of Cardiology, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran
- 4Department of Biostatistics and Epidemiology, Faculty of Health, Alborz University of Medical Sciences, Karaj, Iran
- 5Research Center for Health, Safety and Environment, Alborz University of Medical Sciences, Karaj, Iran
- 6Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran
- KMID: 2522212
- DOI: http://doi.org/10.4258/hir.2021.27.4.307
Abstract
Objectives
Heart failure (HF) is a common disease with a high hospital readmission rate. This study considered class imbalance and missing data, which are two common issues in medical data. The current study’s main goal was to compare the performance of six machine learning (ML) methods for predicting hospital readmission in HF patients.
Methods
In this retrospective cohort study, information of 1,856 HF patients was analyzed. These patients were hospitalized in Farshchian Heart Center in Hamadan Province in Western Iran, from October 2015 to July 2019. The support vector machine (SVM), least-square SVM (LS-SVM), bagging, random forest (RF), AdaBoost, and naïve Bayes (NB) methods were used to predict hospital readmission. These methods’ performance was evaluated using sensitivity, specificity, positive predictive value, negative predictive value, and accuracy. Two imputation methods were also used to deal with missing data.
Results
Of the 1,856 HF patients, 29.9% had at least one hospital readmission. Among the ML methods, LS-SVM performed the worst, with accuracy in the range of 0.57–0.60, while RF performed the best, with the highest accuracy (range, 0.90–0.91). Other ML methods showed relatively good performance, with accuracy exceeding 0.84 in the test datasets. Furthermore, the performance of the SVM and LS-SVM methods in terms of accuracy was higher with the multiple imputation method than with the median imputation method.
Conclusions
This study showed that RF performed better, in terms of accuracy, than other methods for predicting hospital readmission in HF patients.
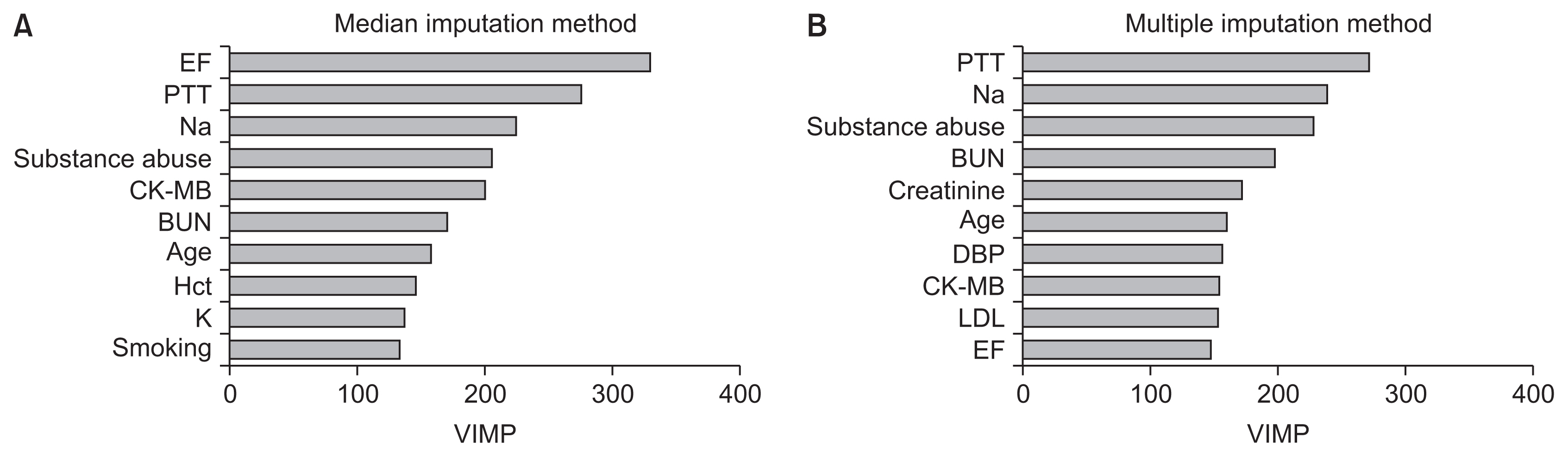
Figure
Reference
-
References
1. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016; 37:2129–200.2. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics-2020 Update: a report from the American Heart Association. Circulation. 2020; 141:e139–e596.
Article3. Braunwald E. The war against heart failure: the Lancet lecture. Lancet. 2015; 385:812–24.
Article4. Rajadurai J, Tse HF, Wang CH, Yang NI, Zhou J, Sim D. Understanding the epidemiology of heart failure to improve management practices: an Asia-Pacific perspective. J Card Fail. 2017; 23:327–39.
Article5. Landicho JA, Esichaikul V, Sasil RM. Comparison of predictive models for hospital readmission of heart failure patients with cost-sensitive approach. Int J Healthc Manag. 2020. Jul. 21. [Epub]. https://doi.org/10.1080/20479700.2020.1797334 .
Article6. Ahmadi A, Soori H, Mobasheri M, Etemad K, Khaledifar A. Heart failure, the outcomes, predictive and related factors in Iran. J Mazandaran Univ Med Sci. 2014; 24:180–8.7. Sahle BW, Owen AJ, Mutowo MP, Krum H, Reid CM. Prevalence of heart failure in Australia: a systematic review. BMC Cardiovasc Disord. 2016; 16:32.
Article8. Negarandeh R, Zolfaghari M, Bashi N, Kiarsi M. Evaluating the effect of monitoring through telephone (tele-monitoring) on self-care behaviors and readmission of patients with heart failure after discharge. Appl Clin Inform. 2019; 10:261–8.
Article9. Gupta A, Fonarow GC. The Hospital Readmissions Reduction Program-learning from failure of a healthcare policy. Eur J Heart Fail. 2018; 20:1169–74.
Article10. Maggioni AP, Orso F, Calabria S, Rossi E, Cinconze E, Baldasseroni S, et al. The real-world evidence of heart failure: findings from 41 413 patients of the ARNO database. Eur J Heart Fail. 2016; 18:402–10.
Article11. Jackson JD, Cotton SE, Bruce Wirta S, Proenca CC, Zhang M, Lahoz R, et al. Burden of heart failure on patients from China: results from a cross-sectional survey. Drug Des Devel Ther. 2018; 12:1659–68.
Article12. Tripoliti EE, Papadopoulos TG, Karanasiou GS, Naka KK, Fotiadis DI. Heart failure: diagnosis, severity estimation and prediction of adverse events through machine learning techniques. Comput Struct Biotechnol J. 2016; 15:26–47.
Article13. Vapnik V. The nature of statistical learning theory. New York (NY): Springer Science & Business Media;2013.14. Tapak L, Shirmohammadi-Khorram N, Amini P, Alafchi B, Hamidi O, Poorolajal J. Prediction of survival and metastasis in breast cancer patients using machine learning classifiers. Clin Epidemiol Glob Health. 2019; 7:293–9.
Article15. Carreira-Perpinan MA, Zharmagambetov A. Ensembles of bagged TAO trees consistently improve over random forests, AdaBoost and gradient boosting. In : FODS ‘20: ACM-IMS Foundations of Data Science Conference; 2020 Oct 19–20; Virtual Event, USA. p. 35–46.
Article16. Mortazavi BJ, Downing NS, Bucholz EM, Dharmarajan K, Manhapra A, Li SX, et al. Analysis of machine learning techniques for heart failure readmissions. Circ Cardiovasc Qual Outcomes. 2016; 9:629–40.
Article17. Awan SE, Bennamoun M, Sohel F, Sanfilippo FM, Dwivedi G. Machine learning-based prediction of heart failure readmission or death: implications of choosing the right model and the right metrics. ESC Heart Fail. 2019; 6:428–35.
Article18. Lorenzoni G, Sabato SS, Lanera C, Bottigliengo D, Minto C, Ocagli H, et al. Comparison of machine learning techniques for prediction of hospitalization in heart failure patients. J Clin Med. 2019; 8:1298.
Article19. Chawla NV, Bowyer KW, Hall LO, Kegelmeyer WP. SMOTE: synthetic minority over-sampling technique. J Artif Intell Res. 2002; 16:321–57.
Article20. Groenwold RHH, Dekkers OM. Missing data: the impact of what is not there. Eur J Endocrinol. 2020; 183:E7–E9.
Article21. Haji-Maghsoudi S, Rastegari A, Garrusi B, Baneshi MR. Addressing the problem of missing data in decision tree modeling. J Appl Stat. 2018; 45:547–57.
Article22. Sohrabi B, Vanani IR, Gooyavar A, Naderi N. Predicting the readmission of heart failure patients through data analytics. J Inf Knowl Manag. 2019; 18:1950012.
Article23. Kalateh Sadati A, Bagheri Lankarani K, Tabrizi R, Rahnavard F, Zakerabasali S. Evaluation of 30-day unplanned hospital readmission in a large teaching hospital in Shiraz, Iran. Shiraz E-Med J. 2017; 18:e39745.
Article24. Mughal MO, Kim S. Signal classification and jamming detection in wide-band radios using Naïve Bayes classifier. IEEE Commun Lett. 2018; 22:1398–401.
Article25. Artetxe A, Larburu N, Murga N, Escolar V, Grana M. Heart failure readmission or early death risk factor analysis: A case study in a telemonitoring program. In : Chen YW, Tanaka S, Howlett R, Jain L, editors. Innovation in Medicine and Healthcare 2017. Cham, Switzerland: Springer;2017. p. 244–53.26. Angraal S, Mortazavi BJ, Gupta A, Khera R, Ahmad T, Desai NR, et al. Machine learning prediction of mortality and hospitalization in heart failure with preserved ejection fraction. JACC Heart Fail. 2020; 8:12–21.
Article27. Frizzell JD, Liang L, Schulte PJ, Yancy CW, Heidenreich PA, Hernandez AF, et al. Prediction of 30-day all-cause readmissions in patients hospitalized for heart failure: comparison of machine learning and other statistical approaches. JAMA Cardiol. 2017; 2:204–9.28. Ouwerkerk W, Voors AA, Zwinderman AH. Factors influencing the predictive power of models for predicting mortality and/or heart failure hospitalization in patients with heart failure. JACC Heart Fail. 2014; 2:429–36.29. Au AG, McAlister FA, Bakal JA, Ezekowitz J, Kaul P, van Walraven C. Predicting the risk of unplanned readmission or death within 30 days of discharge after a heart failure hospitalization. Am Heart J. 2012; 164:365–72.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of Support Vector Machine for Prediction of Medication Adherence in Heart Failure Patients
- Use of Machine Learning in Stroke Rehabilitation: A Narrative Review
- A machine learning model for predicting favorable outcome in severe traumatic brain injury patients after 6 months
- Artificial Intelligence for Adult Spinal Deformity
- Explainable machine learning using perioperative serial laboratory results to predict postoperative mortality in patients with peritonitis-induced sepsis