J Korean Neurosurg Soc.
2021 Nov;64(6):995-1003. 10.3340/jkns.2021.0074.
Central Sarcopenia, Frailty and Comorbidity as Predictor of Surgical Outcome in Elderly Patients with Degenerative Spine Disease
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
- KMID: 2521990
- DOI: http://doi.org/10.3340/jkns.2021.0074
Abstract
Objective
: People are living longer and the elderly population continues to increase. The incidence of degenerative spinal diseases (DSDs) in the elderly population is quite high. Therefore, we are facing more cases of DSD and offering more surgical solutions in geriatric patients. Understanding the significance and association of frailty and central sarcopenia as risk factors for spinal surgery in elderly patients will be helpful in improving surgical outcomes. We conducted a retrospective cohort analysis of prospectively collected data to assess the impact of preoperative central sarcopenia, frailty, and comorbidity on surgical outcome in elderly patients with DSD.
Methods
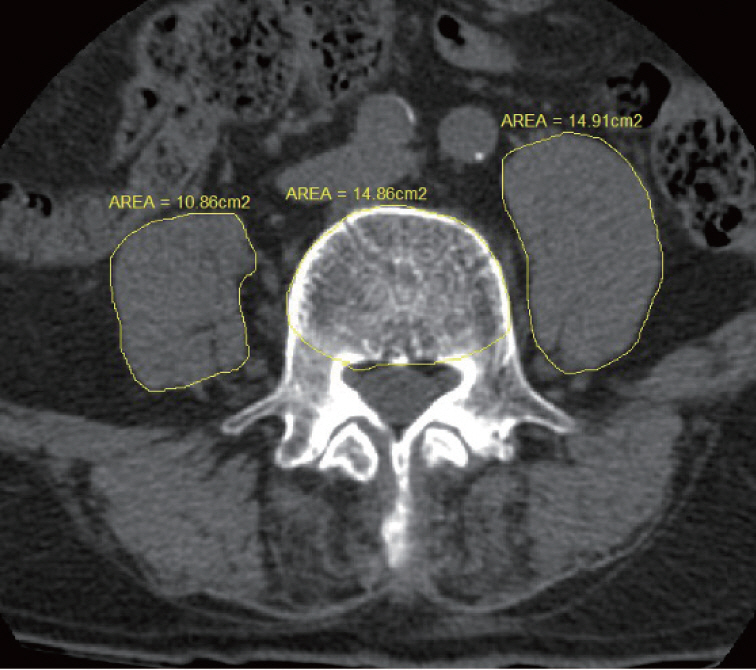
: We conducted a retrospective analysis of patients who underwent elective spinal surgery performed from January 1, 2019 to September 30, 2020 at our hospital. We included patients aged 65 and over who underwent surgery on the thoracic or lumbar spine and were diagnosed as DSD. Central sarcopenia was measured by the 50th percentile of psoas : L4 vertebral index (PLVI) using the cross-sectional area of the psoas muscle. We used the Korean version of the fatigue, resistance, ambulation, illnesses, and loss of weight (K-FRAIL) scale to measure frailty. Comorbidity was confirmed and scored using the Charlson Comorbidity Index (CCI). As a tool for measuring surgical outcome, we used the Clavien-Dindo (CD) classification for postoperative complications and the length of stay (LOS).
Results
: This study included 85 patients (35 males and 50 females). The mean age was 74.05±6.47 years. Using the K-FRAIL scale, four patients were scored as robust, 44 patients were pre-frail and 37 patients were frail. The mean PLVI was 0.61±0.19. According to the CD classification, 50 patients were classified as grade 1, 19 as grade 2, and four as grade 4. The mean LOS was 12.35±8.17 days. Multivariate stepwise regression analysis showed that postoperative complication was significantly associated with surgical invasiveness and K-FRAIL scale. LOS was significantly associated with surgical invasiveness and CCI. K-FRAIL scale showed a significant correlation with CCI and PLVI.
Conclusion
: The present study demonstrates that frailty, comorbidity, and surgical invasiveness are important risk factors for postoperative complications and LOS in elderly patients with DSD. Preoperative recognition of these factors may be useful for perioperative optimization, risk stratification, and patient counseling.
Keyword
Figure
Reference
-
References
1. Agarwal N, Goldschmidt E, Taylor T, Roy S, Dunn SCA, Bilderback A, et al. Impact of frailty on outcomes following spine surgery: a prospective cohort analysis of 668 patients. Neurosurgery. 88:552–557. 2021.
Article2. Balsam LB. Psoas muscle area: a new standard for frailty assessment in cardiac surgery? J Thorac Dis. 10(Suppl 33):S3846–S3849. 2018.
Article3. Camino Willhuber G, Elizondo C, Slullitel P. Analysis of postoperative complications in spinal surgery, hospital length of stay, and unplanned readmission: application of Dindo-Clavien classification to spine surgery. Global Spine J. 9:279–286. 2019.
Article4. Cesari M, Calvani R, Marzetti E. Frailty in older persons. Clin Geriatr Med. 33:293–303. 2017.
Article5. Chang SY, Son J, Park SM, Chang BS, Lee CK, Kim H. Predictive value of comprehensive geriatric assessment on early postoperative complications following lumbar spinal stenosis surgery: a prospective cohort study. Spine (Phila Pa 1976). 45:1498–1505. 2020.
Article6. Charest-Morin R, Street J, Zhang H, Roughead T, Ailon T, Boyd M, et al. Frailty and sarcopenia do not predict adverse events in an elderly population undergoing non-complex primary elective surgery for degenerative conditions of the lumbar spine. Spine J. 18:245–254. 2018.
Article7. Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 47:1245–1251. 1994.
Article8. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 40:373–383. 1987.
Article9. Cizik AM, Lee MJ, Martin BI, Bransford RJ, Bellabarba C, Chapman JR, et al. Using the spine surgical invasiveness index to identify risk of surgical site infection: a multivariate analysis. J Bone Joint Surg Am. 94:335–342. 2012.
Article10. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 48:16–31. 2019.
Article11. Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 393:2636–2646. 2019.
Article12. Dagistan Y, Dagistan E, Gezici AR, Cancan SE, Bilgi M, Cakir U. Effects of minimally invasive decompression surgery on quality of life in older patients with spinal stenosis. Clin Neurol Neurosurg. 139:86–90. 2015.
Article13. Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 303:1259–1265. 2010.
Article14. Dhillon RJ, Hasni S. Pathogenesis and management of sarcopenia. Clin Geriatr Med. 33:17–26. 2017.
Article15. Ebbeling L, Grabo DJ, Shashaty M, Dua R, Sonnad SS, Sims CA, et al. Psoas:lumbar vertebra index: central sarcopenia independently predicts morbidity in elderly trauma patients. Eur J Trauma Emerg Surg. 40:57–65. 2014.
Article16. Gibbons D, Ahern DP, Curley AE, Kepler CK, Butler JS. Impact of sarcopenia on degenerative lumbar spondylosis. Clin Spine Surg. 34:43–50. 2021.
Article17. Hannah TC, Neifert SN, Caridi JM, Martini ML, Lamb C, Rothrock RJ, et al. Utility of the hospital frailty risk score for predicting adverse outcomes in degenerative spine surgery cohorts. Neurosurgery. 87:1223–1230. 2020.
Article18. Indrakusuma R, Zijlmans JL, Jalalzadeh H, Planken RN, Balm R, Koelemay MJW. Psoas muscle area as a prognostic factor for survival in patients with an asymptomatic infrarenal abdominal aortic aneurysm: a retrospective cohort study. Eur J Vasc Endovasc Surg. 55:83–91. 2018.
Article19. Jain A, Hassanzadeh H, Puvanesarajah V, Klineberg EO, Sciubba DM, Kelly MP, et al. Incidence of perioperative medical complications and mortality among elderly patients undergoing surgery for spinal deformity: analysis of 3519 patients. J Neurosurg Spine. 27:534–539. 2017.
Article20. Jang HJ, Chin DK, Park JY, Kuh SU, Kim KS, Cho YE, et al. Influence of frailty on life expectancy in octogenarians after lumbar spine surgery. Neurospine. 18:303–310. 2021.
Article21. Jung HW, Yoo HJ, Park SY, Kim SW, Choi JY, Yoon SJ, et al. The Korean version of the FRAIL scale: clinical feasibility and validity of assessing the frailty status of Korean elderly. Korean J Intern Med. 31:594–600. 2016.
Article22. Kang T, Park SY, Lee JS, Lee SH, Park JH, Suh SW. Predicting postoperative complications in patients undergoing lumbar spinal fusion by using the modified five-item frailty index and nutritional status. Bone Joint J. 102-B:1717–1722. 2020.
Article23. Kim JY, Park IS, Kang DH, Lee YS, Kim KT, Hong SJ. Prediction of risk factors after spine surgery in patients aged >75 years using the modified frailty index. J Korean Neurosurg Soc. 63:827–833. 2020.
Article24. Kleczynski P, Tokarek T, Dziewierz A, Sorysz D, Bagienski M, Rzeszutko L, et al. Usefulness of psoas muscle area and volume and frailty scoring to predict outcomes after transcatheter aortic valve implantation. Am J Cardiol. 122:135–140. 2018.
Article25. Kobayashi K, Imagama S, Sato K, Kato F, Kanemura T, Yoshihara H, et al. Postoperative complications associated with spine surgery in patients older than 90 years: a multicenter retrospective study. Global Spine J. 8:887–891. 2018.
Article26. Kweh B, Lee H, Tan T, O’Donohoe T, Mathew J, Fitzgerald M, et al. Spinal surgery in patients aged 80 years and older: risk stratification using the modified frailty index. Global Spine J. 11:525–532. 2021.
Article27. Mannion AF, Bianchi G, Mariaux F, Fekete TF, Reitmeir R, Moser B, et al. Can the Charlson Comorbidity Index be used to predict the ASA grade in patients undergoing spine surgery? Eur Spine J. 29:2941–2952. 2020.
Article28. Matsuo S, Kawakami M, Minetama M, Nakagawa M, Teraguchi M, Kagotani R, et al. Clinical features of sarcopenia in patients with lumbar spinal stenosis. Spine (Phila Pa 1976). 45:E1105–E1110. 2020.
Article29. Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 16:601–608. 2012.
Article30. Paknikar R, Friedman J, Cron D, Deeb GM, Chetcuti S, Grossman PM, et al. Psoas muscle size as a frailty measure for open and transcatheter aortic valve replacement. J Thorac Cardiovasc Surg. 151:745–751. 2016.
Article31. Rodríguez-Mañas L, Féart C, Mann G, Viña J, Chatterji S, Chodzko-Zajko W, et al. Searching for an operational definition of frailty: a Delphi method based consensus statement: the frailty operative definition-consensus conference project. J Gerontol A Biol Sci Med Sci. 68:62–67. 2013.
Article32. Roffman CE, Buchanan J, Allison GT. Charlson comorbidities index. J Physiother. 62:171. 2016.
Article33. Segal DN, Wilson JM, Staley C, Michael KW. The 5-item modified frailty index is predictive of 30-day postoperative complications in patients undergoing kyphoplasty vertebral augmentation. World Neurosurg. 116:e225–e231. 2018.
Article34. Shen W, Punyanitya M, Wang Z, Gallagher D, St-Onge MP, Albu J, et al. Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross-sectional image. J Appl Physiol (1985). 97:2333–2338. 2004.
Article35. Simcox T, Antoku D, Jain N, Acosta F, Hah R. Frailty syndrome and the use of frailty indices as a preoperative risk stratification tool in spine surgery: a review. Asian Spine J. 13:861–873. 2019.
Article36. Watanabe T, Kanayama M, Takahata M, Oda I, Suda K, Abe Y, et al. Perioperative complications of spine surgery in patients 80 years of age or older: a multicenter prospective cohort study. J Neurosurg Spine. 32:554–558. 2020.
Article37. Yoo JI, Ha YC. Review of epidemiology, diagnosis, and treatment of osteosarcopenia in Korea. J Bone Metab. 25:1–7. 2018.
Article38. Zileli M, Dursun E. How to improve outcomes of spine surgery in geriatric patients. World Neurosurg. 140:519–526. 2020.
Article39. Zuckerman J, Ades M, Mullie L, Trnkus A, Morin JF, Langlois Y, et al. Psoas muscle area and length of stay in older adults undergoing cardiac operations. Ann Thorac Surg. 103:1498–1504. 2017.
Article