Ann Rehabil Med.
2021 Oct;45(5):401-409. 10.5535/arm.21092.
A Risk Factor Analysis of Axillary Web Syndrome in Patients After Breast Cancer Surgery: A Single Center Study in Korea
- Affiliations
-
- 1Department of Rehabilitation Medicine, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea
- 2Department of Surgery, Uijeongbu Eulji Medical Center, Eulji University, Uijeongbu, Korea
- 3Department of Surgery, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea
- KMID: 2521912
- DOI: http://doi.org/10.5535/arm.21092
Abstract
Objective
To investigate the prevalence and risk factors of axillary web syndrome (AWS) in Korean patients.
Methods
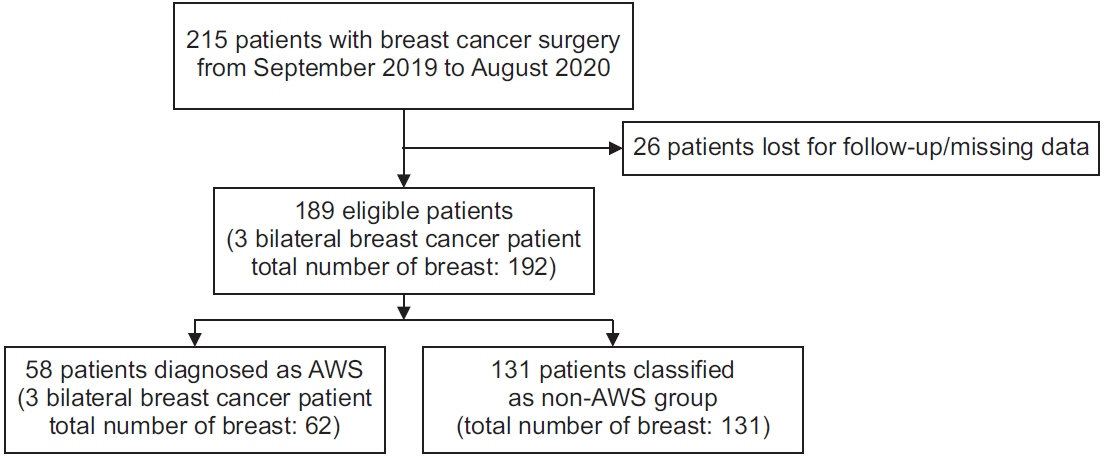
This retrospective study included a total of 189 women who underwent breast cancer surgery and received physical therapy between September 2019 and August 2020. We analyzed AWS and the correlation between the patients’ demographics, underlying disease, type of surgery and chemotherapy or radiation therapy, and lymphedema.
Results
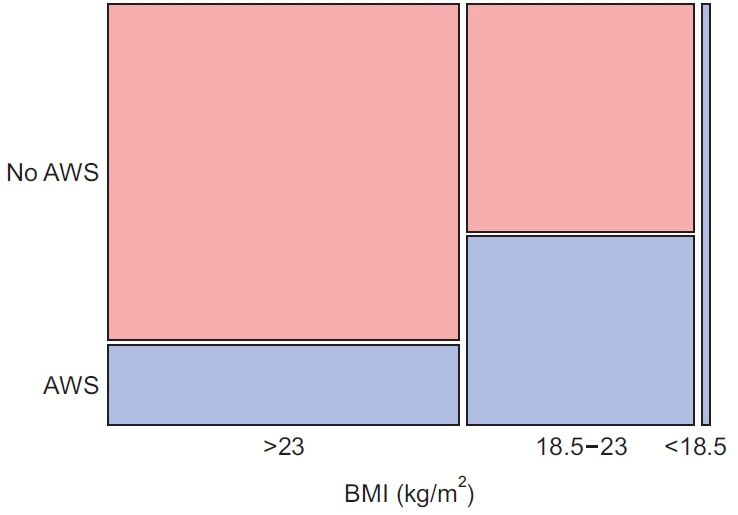
The prevalence of AWS was found to be 30.6%. In the univariable analysis, age, chemotherapy, and hypertension were related to AWS. Finally, the multivariable logistic regression revealed that chemotherapy (odds ratio [OR]=2.84; 95% confidence interval [CI], 1.46–5.53) and HTN (OR=2.72; 95% CI, 1.18–6.30) were the strongest risk factors of AWS.
Conclusion
To the best of our knowledge, this was the first study that explored the risk factors of AWS in a Korean population after breast cancer surgery. As almost one-third of patients suffer from AWS after breast cancer surgery, it is essential to closely monitor the development of AWS in patients with hypertension or undergoing chemotherapy.
Figure
Reference
-
1. Moskovitz AH, Anderson BO, Yeung RS, Byrd DR, Lawton TJ, Moe RE. Axillary web syndrome after axillary dissection. Am J Surg. 2001; 181:434–9.
Article2. Leidenius M, Leppanen E, Krogerus L, von Smitten K. Motion restriction and axillary web syndrome after sentinel node biopsy and axillary clearance in breast cancer. Am J Surg. 2003; 185:127–30.
Article3. Torres Lacomba M, Mayoral Del Moral O, Coperias Zazo JL, Yuste Sanchez MJ, Ferrandez JC, Zapico Goni A. Axillary web syndrome after axillary dissection in breast cancer: a prospective study. Breast Cancer Res Treat. 2009; 117:625–30.
Article4. Figueira P, Haddad C, de Almeida Rizzi S, Facina G, Nazario A. Diagnosis of axillary web syndrome in patients after breast cancer surgery: epidemiology, risk factors, and clinical aspects: a prospective study. Am J Clin Oncol. 2018; 41:992–6.5. Yeung WM, McPhail SM, Kuys SS. A systematic review of axillary web syndrome (AWS). J Cancer Surviv. 2015; 9:576–98.
Article6. de Sire A, Losco L, Cisari C, Gennari A, Boldorini R, Fusco N, et al. Axillary web syndrome in women after breast cancer surgery referred to an Oncological Rehabilitation Unit: which are the main risk factors? A retrospective case-control study. Eur Rev Med Pharmacol Sci. 2020; 24:8028–35.7. Brunelle CL, Roberts SA, Shui AM, Gillespie TC, Daniell KM, Naoum GE, et al. Patients who report cording after breast cancer surgery are at higher risk of lymphedema: results from a large prospective screening cohort. J Surg Oncol. 2020; 122:155–63.
Article8. Huang HC, Liu HH, Yin LY, Weng CH, Fang CL, Yang CS. High incidence of axillary web syndrome among breast cancer survivors after breast reconstruction. Breast Care (Basel). 2020; 15:366–71.
Article9. Fukushima KF, Carmo LA, Borinelli AC, Ferreira CW. Frequency and associated factors of axillary web syndrome in women who had undergone breast cancer surgery: a transversal and retrospective study. Springerplus. 2015; 4:112.
Article10. Severeid K, Simpson J, Templeton B, York R, Hummel- Berry K, Leiserowitz A. Lymphatic cording among patients with breast cancer or melanoma referred to physical therapy. Rehabil Oncol. 2007; 25:8–13.
Article11. Mullen LA, Harvey SC. Review of axillary web syndrome: What the radiologist should know. Eur J Radiol. 2019; 113:66–73.
Article12. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–63.13. Townsend CM, Beauchamp DR, Evers MB, Mattox KL. Sabiston textbook of surgery: the biological basis of modern surgical practice. 20th ed. Philadelphia, PA: Elsevier;2016.14. Jones C, Lancaster R. Evolution of operative technique for mastectomy. Surg Clin North Am. 2018; 98:835–44.
Article15. Bland KI, Suzanne Klimberg V. Master techniques in general surgery: breast surgery. Philadelphia, PA: Lippincott Williams & Wilkins;2011.16. Wyrick SL, Waltke LJ, Ng AV. Physical therapy may promote resolution of lymphatic cording in breast cancer survivors. Rehabil Oncol. 2006; 24:29–34.17. Huh SJ, Yang JH, Park W, Nam SJ, Kim JH. Axillary web syndrome after sentinel node biopsy and axillary lymph node dissection during the conservative treatment of early breast cancer. J Breast Cancer. 2005; 8:94–98.
Article18. Ramirez-Parada K, Garay-Acevedo D, Mella-Abarca W, Petric-Guajardo M, Sanchez-Rojel C, McNeely ML, et al. Axillary web syndrome among Chilean women with breast cancer: incidence and possible predisposing factors. Support Care Cancer. 2020; 28:2941–7.
Article19. Bergmann A, Mendes VV, de Almeida Dias R, do Amaral E Silva B, da Costa Leite Ferreira MG, Fabro EA. Incidence and risk factors for axillary web syndrome after breast cancer surgery. Breast Cancer Res Treat. 2012; 131:987–92.
Article20. Ryans K, Davies CC, Gaw G, Lambe C, Henninge M, VanHoose L. Incidence and predictors of axillary web syndrome and its association with lymphedema in women following breast cancer treatment: a retrospective study. Support Care Cancer. 2020; 28:5881–8.
Article21. Furlan C, Matheus CN, Jales RM, Derchain S, Sarian LO. Vascular alterations in axillary and brachial vessels in patients with axillary web syndrome after breast cancer surgery. Lymphat Res Biol. 2018; 16:287–93.
Article22. Schiffrin EL. Vascular remodeling in hypertension: mechanisms and treatment. Hypertension. 2012; 59:367–74.23. Kim JH, Park JW, Gong HS. Axillary web syndrome after transaxillary robotic thyroidectomy. J Robot Surg. 2014; 8:281–3.
Article24. Rashtak S, Gamble GL, Gibson LE, Pittelkow MR. From furuncle to axillary web syndrome: shedding light on histopathology and pathogenesis. Dermatology. 2012; 224:110–4.
Article25. Nakagawa A, Fujimoto H, Nagashima T, Sangai T, Takada M, Masuda T, et al. Histological features of skin and subcutaneous tissue in patients with breast cancer who have received neoadjuvant chemotherapy and their relationship to post-treatment edema. Breast Cancer. 2020; 27:77–84.
Article26. Lee KW, Kim SB, Lee JH, Kim YS. Effects of extracorporeal shockwave therapy on improvements in lymphedema, quality of life, and fibrous tissue in breast cancer-related lymphedema. Ann Rehabil Med. 2020; 44:386–92.
Article27. Wariss BR, Costa RM, Pereira AC, Koifman RJ, Bergmann A. Axillary web syndrome is not a risk factor for lymphoedema after 10 years of follow-up. Support Care Cancer. 2017; 25:465–70.28. Grada AA, Phillips TJ. Lymphedema: pathophysiology and clinical manifestations. J Am Acad Dermatol. 2017; 77:1009–20.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Axillary Web Syndrome after Sentinel Node Biopsy and Axillary Lymph Node Dissection during the Conservative Treatment of Early Breast Cancer
- Patterns of Axillary Lymph Node Metastasis in Breast Cancer: A Prospective Single-Center Study
- A Clinical Case of Axillary Web Syndrome after Glandular Tissue and Skin Removal for Axillary Osmidrosis
- Clinical Significance of the Axillary Arch in Sentinel Lymph Node Biopsy
- Clinically Positive Axillary Lymphadenopathy May Lead to False Diagnosis of Overstaged Breast Cancer in Patients with Sjogren's Syndrome: A Case Report