Ann Rehabil Med.
2021 Oct;45(5):393-400. 10.5535/arm.21076.
Sensory Based Feeding Intervention for Toddlers With Food Refusal: A Randomized Controlled Trial
- Affiliations
-
- 1Department of Physical and Rehabilitation Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Rehabilitation Medicine, Seoul Rehabilitation Hospital, Seoul, Korea
- 3Department of Occupational Therapy, Seoul Rehabilitation Hospital, Seoul, Korea
- KMID: 2521911
- DOI: http://doi.org/10.5535/arm.21076
Abstract
Objective
To investigate the effect of sensory-based feeding treatment for toddlers with food refusal compared with only providing nutrition education.
Methods
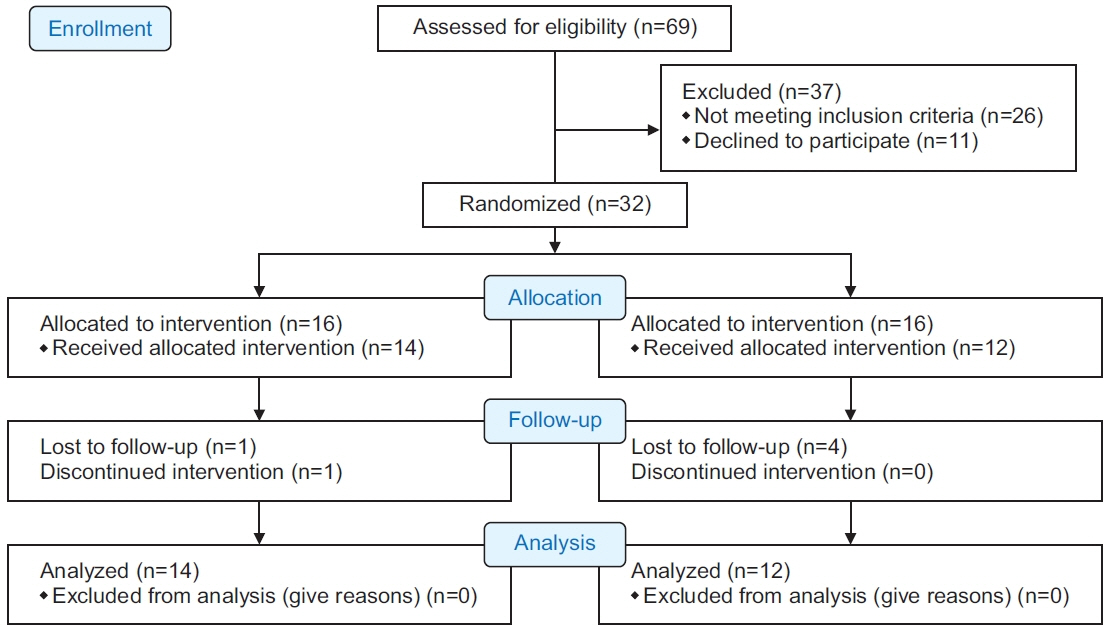
Thirty-two toddlers with food refusal were randomly assigned to an intervention group or the control group. Toddlers in the intervention group received the sensory-based feeding intervention and the duration was for 1 hour for 5 days per week for 4 weeks, and then 1 hour, once a week for 8 weeks. Subjects in both the intervention and control groups received nutritional education once every 4 weeks for 12 weeks. The participants were evaluated at their entry into the study and 12 weeks later based on height, weight, behavior at mealtime using the Behavioral Pediatrics Feeding Assessment Scale (BPFAS), and sensory processing ability using the Infant/Toddler Sensory Profile.
Results
Sixteen toddlers were included in each group. Two subjects in the intervention group and four toddlers in the control group were excluded from the final analysis. Significant improvements in child or parent subscales of the BPFAS were observed in the intervention group. In contrast, there were no significant improvements in any BPFAS scores in the control group.
Conclusion
Sensory-based feeding intervention was effective for improving mealtime behavior in toddlers with food refusal. Therefore, a sensory-based feeding intervention could be considered as an intervention approach to address feeding disorders in toddlers.
Figure
Reference
-
1. Field D, Garland M, Williams K. Correlates of specific childhood feeding problems. J Paediatr Child Health. 2003; 39:299–304.
Article2. Staiano A. Food refusal in toddlers with chronic diseases. J Pediatr Gastroenterol Nutr. 2003; 37:225–7.
Article3. Crist W, Napier-Phillips A. Mealtime behaviors of young children: a comparison of normative and clinical data. J Dev Behav Pediatr. 2001; 22:279–86.
Article4. Dahl M, Sundelin C. Early feeding problems in an affluent society. I. Categories and clinical signs. Acta Paediatr Scand. 1986; 75:370–9.5. Dahl M, Sundelin C. Feeding problems in an affluent society: follow-up at four years of age in children with early refusal to eat. Acta Paediatr. 1992; 81:575–9.
Article6. Dahl M, Rydell AM, Sundelin C. Children with early refusal to eat: follow-up during primary school. Acta Paediatr. 1994; 83:54–8.
Article7. Davis AM, Bruce AS, Khasawneh R, Schulz T, Fox C, Dunn W. Sensory processing issues in young children presenting to an outpatient feeding clinic. J Pediatr Gastroenterol Nutr. 2013; 56:156–60.
Article8. Yi SH, Joung YS, Choe YH, Kim EH, Kwon JY. Sensory processing difficulties in toddlers with nonorganic failure-to-thrive and feeding problems. J Pediatr Gastroenterol Nutr. 2015; 60:819–24.
Article9. Williams KE, Field DG, Seiverling L. Food refusal in children: a review of the literature. Res Dev Disabil. 2010; 31:625–33.
Article10. SOS Approach to Feeding [Internet]. [place unknown]: SOS Approach to Feeding;c2021. [cited 2021 Oct 1]. Available from: http://www.sosapproachtofeeding.com/.11. Bayley N. Bayley Scales of Infant Development. 2nd ed. San Antonio, TX: Psychological Corporation;1993.12. Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaign, IL: Human Kinetics;1991.13. Waterlow JC, Buzina R, Keller W, Lane JM, Nichaman MZ, Tanner JM. The presentation and use of height and weight data for comparing the nutritional status of groups of children under the age of 10 years. Bull World Health Organ. 1977; 55:489–98.14. WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006; 450:76–85.15. WHO Working Group. Use and interpretation of anthropometric indicators of nutritional status. Bull World Health Organ. 1986; 64:929–41.16. Powers SW, Mitchell MJ, Patton SR, Byars KC, Jelalian E, Mulvihill MM, et al. Mealtime behaviors in families of infants and toddlers with cystic fibrosis. J Cyst Fibros. 2005; 4:175–82.
Article17. Dunn W. Infant toddler sensory profile. San Antonio, TX: Psychological Corporation;2002.18. Benoit D, Wang EE, Zlotkin SH. Discontinuation of enterostomy tube feeding by behavioral treatment in early childhood: a randomized controlled trial. J Pediatr. 2000; 137:498–503.
Article19. Addison LR, Piazza CC, Patel MR, Bachmeyer MH, Rivas KM, Milnes SM, et al. A comparison of sensory integrative and behavioral therapies as treatment for pediatric feeding disorders. J Appl Behav Anal. 2012; 45:455–71.
Article20. Verbal Beginnings. A behavioral approach to feeding therapy [Internet]. Columbia, MD: Verbal Beginnings; [cited 2021 Oct 1]. Available from: https://www.verbalbeginnings.com/aba-blog/a-behavioral-approach-to-feeding-therapy/.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How to approach feeding difficulties in young children
- Review of Early Intervention for Children with Autism Spectrum Disorder: Focused on Randomized Controlled Trials
- Nutritional Status of Korean Toddlers: From the Korean National Health and Nutrition Examination Survey 2007~2009
- Diet Therapy Using a Small Rice Bowl among Japanese Men with Diabetes: A Randomized Controlled Trial
- Effect of Oropharyngeal Sensory Stimulation Using Capsaicin in Acute Stroke Patients with Dysphagia