Ann Rehabil Med.
2021 Oct;45(5):368-378. 10.5535/arm.21035.
Factors Affecting the Swallowing Dysfunction Following Oral Cancer Surgery
- Affiliations
-
- 1Department of Rehabilitation, Kumamoto Health Science University, Kumamoto, Japan
- 2Department of Otolaryngology Head and Neck Surgery, Nagasaki University Graduate School of Medicine, Nagasaki, Japan
- 3Department of Otolaryngology Head and Neck Surgery, Kumamoto University Graduate School of Medicine, Kumamoto, Japan
- 4Department of Otolaryngology, Kumamoto Kinoh Hospital, Kumamoto, Japan
- KMID: 2521909
- DOI: http://doi.org/10.5535/arm.21035
Abstract
Objective
To investigate the factors affecting the postoperative swallowing dysfunction in patients who underwent oral cancer surgery.
Methods
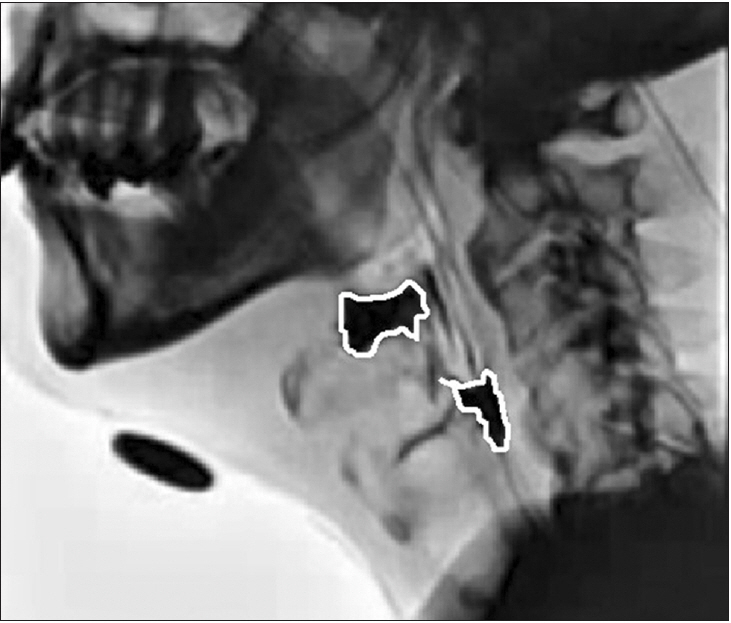
Retrospective review of clinical records of 70 patients (50 males and 20 females) who underwent oral cancer surgeries from July 2007 to April 2015 were enrolled. Multiple regression analysis was performed using the Food Intake LEVEL Scale (FILS) at discharge as the objective variable and age, tumor size, resection of the tongue base, suprahyoid muscle resection, segmental mandibulectomy, neck dissection and radiation therapy as the explanatory variables in 70 patients. In addition, multiple regression analysis was performed between objective variables, which include maximum hyoid bone movement, laryngeal elevation delay time, pharyngeal constriction ratio (PCR), residue in the vallecular and pear-shaped depression (pyriform sinuses), and Penetration-Aspiration Scale score and one of the main factors representing the characteristics of each case as the explanatory variables, and age was treated as an adjustment factor in 23 patients.
Results
The FILS shows significant negative correlation by age and resection of the tongue base. In videofluoroscopic swallowing study, the maximum movement, PCR and residue in the vallecular are significantly correlated with factors demonstrating the characteristic for each case.
Conclusion
It was suggested that in elderly patients, the presence of more than half of the tongue base resection, suprahyoid muscle resection and neck dissection cause severe dysphagia after surgery.
Keyword
Figure
Cited by 1 articles
-
Correlation Between Articulatory Diadochokinetic Parameters and Dysphagia Parameters in Subacute Stroke Patients
Back Min Oh, Hyun Seok, Sang-Hyun Kim, Seung Yeol Lee, Su Jung Park, Beom Jin Kim, Hyun Jung Kim
Ann Rehabil Med. 2023;47(3):192-204. doi: 10.5535/arm.23018.
Reference
-
1. Fujimoto Y, Hasegawa Y, Yamada H, Ando A, Nakashima T. Swallowing function following extensive resection of oral or oropharyngeal cancer with laryngeal suspension and cricopharyngeal myotomy. Laryngoscope. 2007; 117:1343–8.
Article2. Matsunaga K, Mori K, Asamura S, Nagata T, Isogai N. Swallowing function in patients who underwent hemiglossectomy and reconstruction with a pectoralis major myocutaneous flap. Nihon Gekakei Rengo Gakkaishi. 2008; 33:829–36.
Article3. Pauloski BR, Rademaker AW, Logemann JA, Colangelo LA. Speech and swallowing in irradiated and nonirradiated postsurgical oral cancer patients. Otolaryngol Head Neck Surg. 1998; 118:616–24.
Article4. Pauloski BR, Logemann JA, Fox JC, Colangelo LA. Biomechanical analysis of the pharyngeal swallow in postsurgical patients with anterior tongue and floor of mouth resection and distal flap reconstruction. J Speech Hear Res. 1995; 38:110–23.
Article5. Fujishima I. [Textbook of rehabilitation for swallowing disorders associated with stroke]. 3rd ed. Tokyo, Japan: Ishiyaku Publishers;1993. p. 143–52.6. Kunieda K, Ohno T, Fujishima I, Hojo K, Morita T. Reliability and validity of a tool to measure the severity of dysphagia: the Food Intake LEVEL Scale. J Pain Symptom Manag. 2013; 46:201–6.
Article7. Cook IJ, Dodds WJ, Dantas RO, Kern MK, Massey BT, Shaker R, et al. Timing of videofluoroscopic, manometric events, and bolus transit during the oral and pharyngeal phases of swallowing. Dysphagia. 1989; 4:8–15.
Article8. Maruo T, Fujimoto Y, Ozawa K, Hiramatsu M, Suzuki A, Nishio N, et al. Laryngeal sensation and pharyngeal delay time after (chemo)radiotherapy. Eur Arch Otorhinolaryngol. 2014; 271:2299–304.
Article9. Miyaji H, Umezaki T, Adachi K, Sawatsubashi M, Kiyohara H, Inoguchi T, et al. Videofluoroscopic assessment of pharyngeal stage delay reflects pathophysiology after brain infarction. Laryngoscope. 2012; 122:2793–9.
Article10. Leonard R, Belafsky PC, Rees CJ. Relationship between fluoroscopic and manometric measures of pharyngeal constriction: the pharyngeal constriction ratio. Ann Otol Rhinol Laryngol. 2006; 115:897–901.
Article11. Logemann JA. Evaluation and treatment of swallowing disorders. Austin, TX: Pro-ED;1998. p. 71–133.12. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–8.
Article13. Kojima A, Imoto Y, Osawa Y, Fujieda S. Predictor of rehabilitation outcome for dysphagia. Auris Nasus Larynx. 2014; 41:294–8.
Article14. Wakabayashi H, Takahashi R, Watanabe N, Oritsu H, Shimizu Y. Prevalence of skeletal muscle mass loss and its association with swallowing function after cardiovascular surgery. Nutrition. 2017; 38:70–3.
Article15. Kaneko I. [A cinefluorographic study of hyoid bone movement during deglutition]. Nihon Jibiinkoka Gakkai Kaiho. 1992; 95:974–87.
Article16. Nishikubo K, Mise K, Ameya M, Hirose K, Kobayashi T, Hyodo M. Quantitative evaluation of age-related alteration of swallowing function: videofluoroscopic and manometric studies. Auris Nasus Larynx. 2015; 42:134–8.
Article17. Pauloski BR, Rademaker AW, Logemann JA, McConnel FM, Heiser MA, Cardinale S, et al. Surgical variables affecting swallowing in patients treated for oral/oropharyngeal cancer. Head Neck. 2004; 26:625–36.
Article18. Chang YC, Chen SY, Lui LT, Wang TG, Wang TC, Hsiao TY, et al. Dysphagia in patients with nasopharyngeal cancer after radiation therapy: a videofluoroscopic swallowing study. Dysphagia. 2003; 18:135–43.
Article19. Jensen K, Lambertsen K, Grau C. Late swallowing dysfunction and dysphagia after radiotherapy for pharynx cancer: frequency, intensity and correlation with dose and volume parameters. Radiother Oncol. 2007; 85:74–82.
Article20. Pearson WG Jr, Langmore SE, Zumwalt AC. Evaluating the structural properties of suprahyoid muscles and their potential for moving the hyoid. Dysphagia. 2011; 26:345–51.
Article21. Ohashi N, Iwai T, Tohara H, Chiba Y, Oguri S, Koizumi T, et al. Swallowing function in advanced tongue cancer patients before and after bilateral neck dissection following superselective intra-arterial chemoradiotherapy for organ preservation: a case-control study. Oral Radiol. 2019; 35:230–8.
Article22. Pauloski BR, Logemann JA. Impact of tongue base and posterior pharyngeal wall biomechanics on pharyngeal clearance in irradiated postsurgical oral and oropharyngeal cancer patients. Head Neck. 2000; 22:120–31.
Article23. Hoffman MR, Mielens JD, Ciucci MR, Jones CA, Jiang JJ, McCulloch TM. High-resolution manometry of pharyngeal swallow pressure events associated with effortful swallow and the Mendelsohn maneuver. Dysphagia. 2012; 27:418–26.
Article24. Mendelsohn MS, Martin RE. Airway protection during breath-holding. Ann Otol Rhinol Laryngol. 1993; 102:941–4.
Article25. Boden K, Hallgren A, Witt Hedstrom H. Effects of three different swallow maneuvers analyzed by videomanometry. Acta Radiol. 2006; 47:628–33.
Article26. Leonard RJ, Kendall KA, McKenzie S, Goncalves MI, Walker A. Structural displacements in normal swallowing: a videofluoroscopic study. Dysphagia. 2000; 15:146–52.
Article27. Wintzen AR, Badrising UA, Roos RA, Vielvoye J, Liauw L. Influence of bolus volume on hyoid movements in normal individuals and patients with Parkinson’s disease. Can J Neurol Sci. 1994; 21:57–9.
Article28. Ohkubo M, Sugiyama T, Ohira M, Yamamoto M, Iguchi T, Shibahara T, et al. Swallowing rehabilitation affects period of hospitalization after surgery for tongue cancer. Bull Tokyo Dent Coll. 2017; 58:19–26.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dysphagia after Oral Cavity and Hypopharyngeal Cancer Surgery
- Anatomy and Physiology of Normal Swallowing
- Dysphagia in Tongue Cancer Patients
- Diet Modification for Dysphagia in Oral Phase Associated with Aging
- Obturator Prosthesis for Velopharyngeal Insufficiency after Treatment of Soft Palate Cancer: A Case Report