J Cerebrovasc Endovasc Neurosurg.
2021 Sep;23(3):201-209. 10.7461/jcen.2021.E2020.10.007.
Usefulness of three-dimensional fast imaging employing steady-state acquisition MRI of large vessel occlusion for detecting occluded middle cerebral artery and internal carotid artery before acute mechanical thrombectomy
- Affiliations
-
- 1Department of Neurosurgery, Seijinkai Shimizu Hospital, Kyoto, Japan
- KMID: 2520879
- DOI: http://doi.org/10.7461/jcen.2021.E2020.10.007
Abstract
Objective
Acute mechanical thrombectomy (AMT) in patients with acute ischemic stroke from large vessel occlusion (LVO) is performed without directly identifying the occluded vessels. In this study, we evaluated whether 1.5 T magnetic resonance imaging (MRI) with 3D-fast imaging employing steady-state acquisition (FIESTA) could visualize the occluded intracranial middle cerebral artery (MCA) and internal carotid artery (ICA) before AMT.
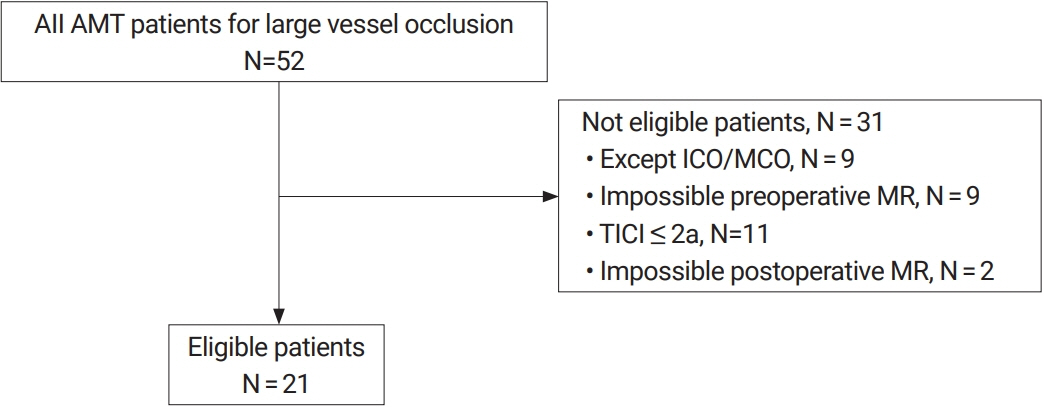
Methods
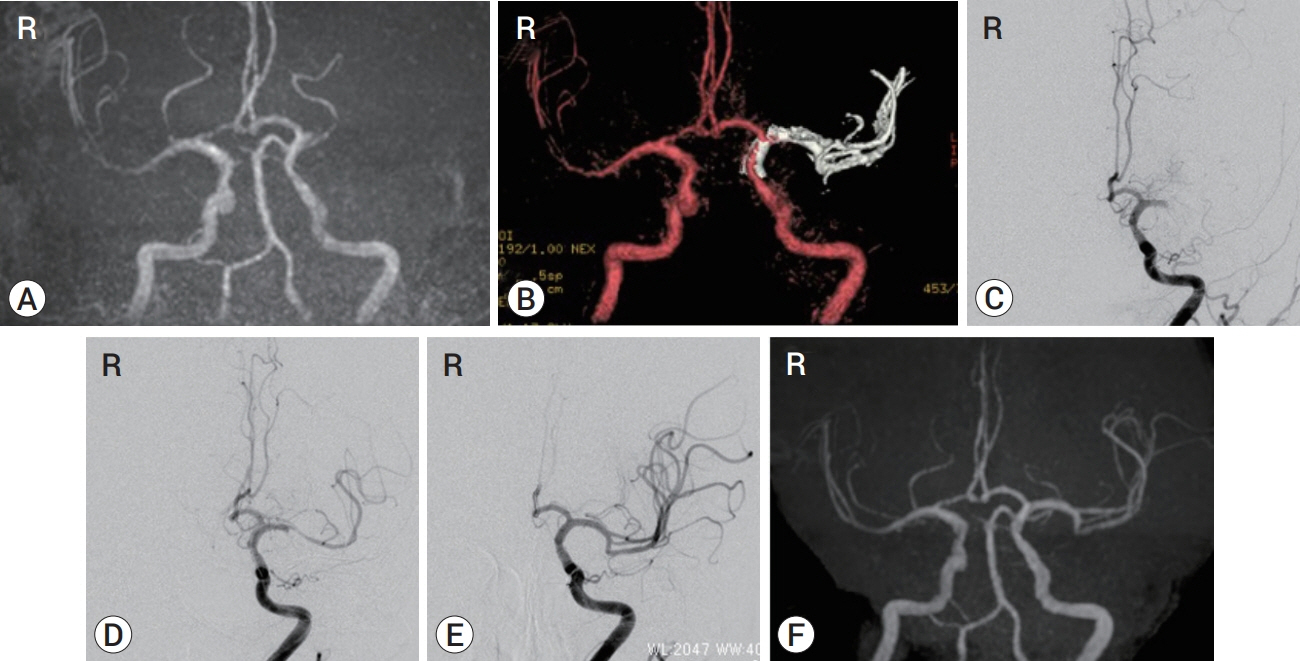
This retrospective study included 21 consecutive patients who underwent time-of-flight magnetic resonance angiography (TOF MRA) and 3D-FIESTA MRI immediately before AMT. The patients also underwent TOF MRA after AMT and achieved TICI 2b or 3 by AMT at our hospital between February 2018 and April 2019. When LVO in the anterior circulation was detected by TOF MRA, 3D-FIESTA MRI was additionally performed. Then, the occluded intracranial MCA and ICA, including their branches, were constructed on the workstation with volume rendering. The obtained images were fused with the TOF MRA images to create combined 3D images.
Results
The length and top-to-bottom distance of the affected M1 segment (calculated by the ipsilateral-to-contralateral ratio) were 1.29 and 1.17, respectively, on 3D-FIESTA MRI before AMT and 1.34 and 1.24, respectively, on TOF MRA after AMT. We assessed the number of M2 segments branching from the affected M1/M2 junction and visualized the affected anterior temporal artery. The 3D-FIESTA MRI before AMT and TOF MRA after AMT were consistent in all patients, except for two who moved vigorously during imaging.
Conclusions
Images acquired by 1.5T 3D-FIESTA MRI can visualize to predict the existing path of the occluded MCA and ICA before AMT in patients with LVO of the anterior circulation.
Keyword
Figure
Reference
-
1. Abanou A, Lasjaunias P, Manelfe C, Lopez-lbor L. The accessory middle cerebral artery (MCA). diagnostic and therapeutic consequences. Anat Clin. 1984; 6(4):305–9.2. Amano T, Sato M, Matsumaru Y, Sakuma H, Yoda S, Hamada Y. Intra-arterial contrasted cone-beam computed tomography assessment of vessels distal from occluded site in acute ischemic stroke with major vessel occlusion. Neurol Med Chir (Tokyo). 2017; Jun. 57(6):292–8.
Article3. Balami JS, White PM, McMeekin PJ, Ford GA, Buchan AM. Complication of endovascular treatment for acute ischemic stroke: prevention and management. Int J Stroke. 2018; Jun. 13(4):348–61.4. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; Jan. 372(1):11–20.5. Blanc R, Pistocchi S, Babic D, Bartolini B, Obadia M, Alamowitch S, et al. Intravenous flat-detector CT angiography in acute ischemic stroke management. Neuroradiology. 2012; Apr. 54(4):383–91.
Article6. EXTEND- IA TNK Investigators. Tenecteplase versus alteplase before thrombectomy for ischemic stroke. N Engl J Med. 2018; Apr. 378(17):1573–82.7. Gibo H, Carver CC, Rhoton AL Jr, Lenkey C, Mitchell RJ. Microsurgical anatomy of the middle cerebral artery. J Neurosurg. 1981; Feb. 54(2):151–69.
Article8. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; Mar. 372(11):1019–30.9. Hayashi K, Takahashi N, Furuichi S, Yoshioka T, Shibata S. Two cases of cerebral aneurysm detected after recanalization of the middle cerebral artery. No Shinkei Geka. 1998; Dec. 26(12):1103–7.10. Hoelter P, Goelitz P, Lang S, Luecking H, Kalmuenzer B, Struffert T, et al. Visualization of large vessel occlusion, clot extent, and collateral supply using volume perfusion flat detector computed tomography in acute stroke patients. Acta Radiol. 2019; Nov. 60(11):1504–11.
Article11. Iwasaki M, Saito M, Nemoto A, Suzuki T, Hikita C, Fukuta S, et al. Diluted contrast-enhanced cone-beam CT during acutephase recanalization therapy for occlusion of the middle cerebral artery. J Neuroendovascular Therapy. 2019; Feb. 13(2):91–4.
Article12. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; Jun. 372(24):2296–306.
Article13. Kahilogullari G, Ugur HC, Comert A, Tekdemir I, Kanpolat Y. The branching pattern of the middle cerebral artery: is the intermediate trunk real or not? An anatomical study correlating with simple angiography. J Neurosurg. 2012; May. 116(5):1024–34.
Article14. Kaku Y, Morioka M, Ohmori Y, Kawano T, Kai Y, Fukuoka H, et al. Outer-diameter narrowing of the internal carotid and middle cerebral arteries in moyamoya disease detected on 3D constructive interference in steady-state MR image: is arterial constrictive remodeling a major pathogenesis? Acta Neurochir (Wien). 2012; Dec. 154(12):2151–7.
Article15. Kimura T, Morita A. Treatment of unruptured aneurysm of duplication of the middle cerebral artery--case report. Neurol Med Chir (Tokyo). 2010; 50(2):124–6.16. Komiyama M, Nakajima H, Nishikawa M, Yasui T. Middle cerebral artery variations: duplicated and accessory arteries. AJNR Am J Neuroradiol. 1998; Jan. 19(1):45–9.17. Kuribara T, Haraguchi K, Ogane K, Matsuura N, Ito T. 3D-FIESTA magnetic resonance angiography fusion imaging of distal segment of occluded middle cerebral artery. Neurol Med Chir (Tokyo). 2015; 55(10):805–8.
Article18. Mokin M, Fargen KM, Primiani CT, Ren Z, Dumont TM, Brasiliense LBC, et al. Vessel perforation during stent retriever thrombectomy for acute ischemic stroke: technical details and clinical outcomes. J Neurointerv Surg. 2017; Oct. 9(10):922–8.
Article19. Nikoubashman O, Dekeyzer S, Riabikin A, Keulers A, Reich A, Mpotsaris A, et al. True first-pass effect. Stroke. 2019; Aug. 50(8):2140–6.
Article20. Saber H, Narayanan S, Palla M, Saver JL, Nogueira RG, Yoo AJ, et al. Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: a meta-analysis. J Neurointerv Surg. 2018; Jul. 10(7):620–4.
Article21. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, HERMES Collaborators, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016; Sep. 316(12):1279–88.
Article22. Schwaiger BJ, Gersing AS, Zimmer C, Prothmann S. The Curved MCA: Influence of vessel anatomy on recanalization results of mechanical thrombectomy after acute ischemic stroke. AJNR Am J Neuroradiol. 2015; May. 36(5):971–6.
Article23. Shirakawa M, Yoshimura S, Uchida K, Shindo S, Yamada K, Kuroda J, et al. Relationship between hemorrhagic complications and target vessels in acute thrombectomy. J Stroke Cerebrovasc Dis. 2017; Aug. 26(8):1732–8.
Article24. Smit EJ, Vonken EJ, van Seeters T, Dankbaar JW, van der Schaaf IC, Kappelle LJ, et al. Timing-invariant imaging of collateral vessels in acute ischemic stroke. Stroke. 2013; Aug. 44(8):2194–9.
Article25. Teal JS, Rumbaugh CL, Bergeron RT, Segall HD. Anomalies of the middle cerebral artery: accessory artery, duplication, and early birfurcation. Am J Roentgenol Radium Ther Nucl Med. 1973; Jul. 118(3):567–75.26. Turk AS, Frei D, Fiorella D, Mocco J, Baxter B, Siddiqui A, Spiotta A, et al. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. 2014; May. 6(4):260–4.
Article27. Umansky F, Juarez SM, Dujovny M, Ausman JI, Diaz FG, Gomes F, et al. Microsurgical anatomy of the proximal segments of the middle cerebral artery. J Neurosurg. 1984; Sep. 61(3):458–67.
Article28. Yamamoto S, Yamagami H, Todo K, Kuramoto Y, Ishikawa T, Imamura H, et al. Correlation of middle cerebral artery tortuosity with successful recanalization using the Merci retrieval system with or without adjunctive treatments. Neurol Med Chir (Tokyo). 2014; 54(2):113–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How to Escape Stentriever Wedging in an Open-cell Carotid Stent during Mechanical Thrombectomy for Tandem Cervical Internal Carotid Artery and Middle Cerebral Artery Occlusion
- Transcarotid Mechanical Thrombectomy for Embolic Intracranial Large Vessel Occlusion after Endovascular Deconstructice Embolization for Carotid Blowout Syndrome
- Aspiration Clot Removal by Mannual Compression of Common Carotid Artery for Acute Internal Carotid Occlusion: a Case Report
- Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: A literature review
- Emergency Microsurgical Embolectomy for the Treatment of Acute Intracranial Artery Occlusion: Report of Two Cases