Korean J Transplant.
2021 Sep;35(3):195-199. 10.4285/kjt.21.0013.
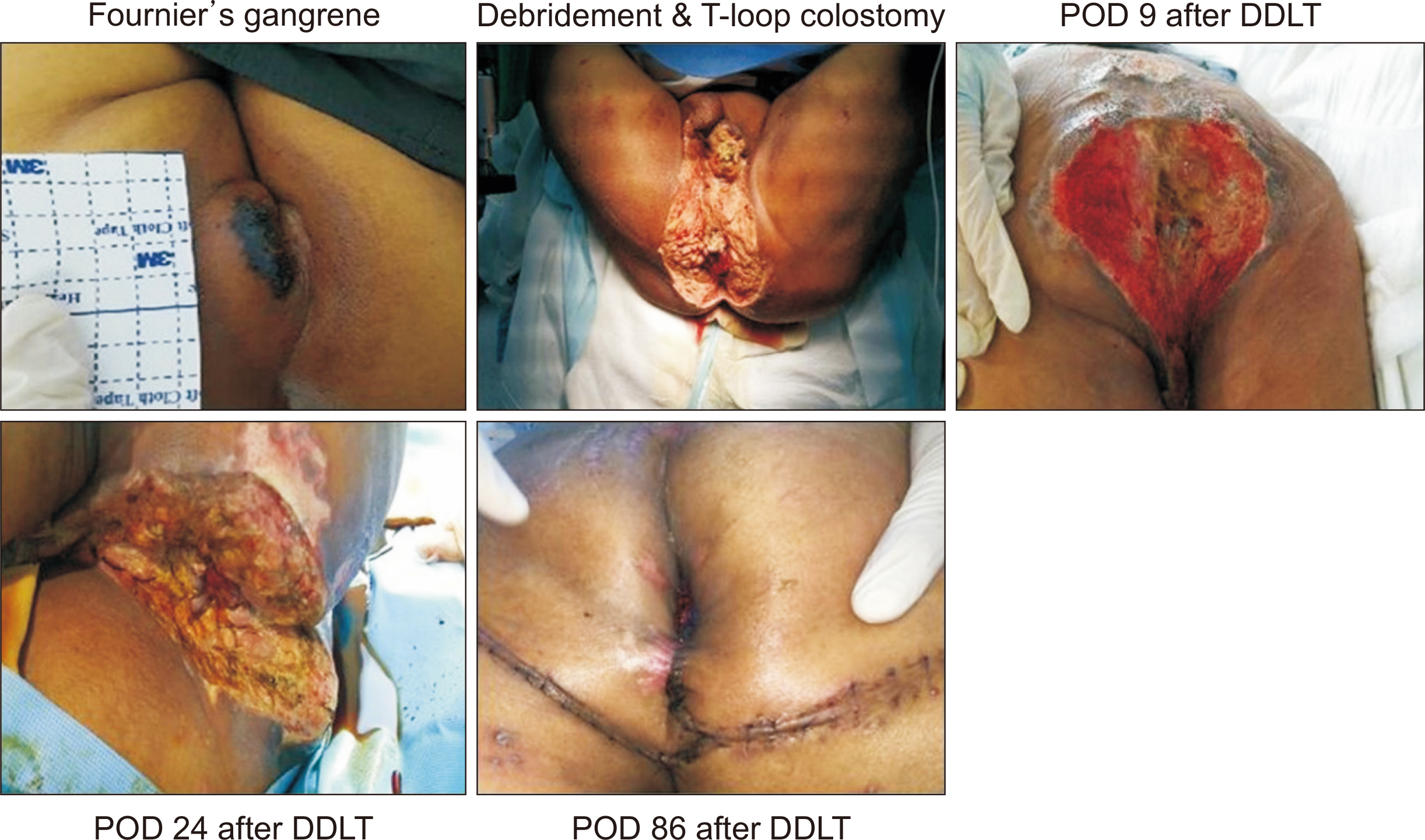
Selected deceased donor liver transplantation in controlled Fournier’s gangrene: a case report
- Affiliations
-
- 1Division of Hepato-Biliary-Pancreatic Surgery and Transplantation, Department of Surgery, Pusan National University Hospital, Busan, Korea
- 2Department of Surgery, Veterans Health Service Medical Center, Seoul, Korea
- 3Division of Colorectal Surgery, Department of Surgery, Pusan National University Hospital, Busan, Korea
- 4Division of Hepato-Biliary-Pancreatic Surgery and Transplantation, Department of Surgery, Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- KMID: 2520688
- DOI: http://doi.org/10.4285/kjt.21.0013
Abstract
- Bacterial infection represents a turning point in the natural history of cirrhosis, causing the development of acute-on-chronic liver failure. It significantly affects the outcome of patients listed for liver transplantation. We report the case of a 57-year-old man who had been regularly treated for hepatitis B virus, alcoholic liver cirrhosis, and hepatic failure. The patient was hospitalized again due to variceal bleeding and hepatic coma. He visited the emergency room with painful anal swelling, dysuria, icteric sclera, and serious abdominal distension. The painful anal swelling and necrosis progressed; thus, he was diagnosed with Fournier’s gangrene. Enterococcus faecium and Candida albicans were detected in the blood. Gangrene wound debris was studied extensively. Despite appropriate antibiotic treatment, vancomycin-resistant enterococcus and C. albicans were continuously present in the blood. Wide debridement of the wound and T-colostomy were performed. After this, norepinephrine and vasopressin were used to maintain stable vital signs. It was difficult to establish a liver transplant operation. Despite repeated bleeding, bacterial infections improved with additional antibiotics. Finally, selected deceased donor liver transplantation in controlled Fournier’s gangrene was successfully performed. Controlled infections may be allowed in transplantation surgery.
Figure
Reference
-
1. Gustot T, Agarwal B. 2017; Selected patients with acute-on-chronic liver failure grade 3 are not too sick to be considered for liver transplantation. J Hepatol. 67:667–8. DOI: 10.1016/j.jhep.2017.07.017. PMID: 28923205.
Article2. Putignano A, Gustot T. 2017; New concepts in acute-on-chronic liver failure: implications for liver transplantation. Liver Transpl. 23:234–43. DOI: 10.1002/lt.24654. PMID: 27750389.
Article3. Bertuzzo VR, Giannella M, Cucchetti A, Pinna AD, Grossi A, Ravaioli M, et al. 2017; Impact of preoperative infection on outcome after liver transplantation. Br J Surg. 104:e172–81. DOI: 10.1002/bjs.10449. PMID: 28121031.
Article4. Artru F, Louvet A, Ruiz I, Levesque E, Labreuche J, Ursic-Bedoya J, et al. 2017; Liver transplantation in the most severely ill cirrhotic patients: a multicenter study in acute-on-chronic liver failure grade 3. J Hepatol. 67:708–15. DOI: 10.1016/j.jhep.2017.06.009. PMID: 28645736.
Article5. Strnad P, Tacke F, Koch A, Trautwein C. 2017; Liver: guardian, modifier and target of sepsis. Nat Rev Gastroenterol Hepatol. 14:55–66. DOI: 10.1038/nrgastro.2016.168. PMID: 27924081.6. Reddy KR, O'Leary JG, Kamath PS, Fallon MB, Biggins SW, Wong F, et al. 2015; High risk of delisting or death in liver transplant candidates following infections: results from the North American Consortium for the Study of End-Stage Liver Disease. Liver Transpl. 21:881–8. DOI: 10.1002/lt.24139. PMID: 25845966.
Article7. Mücke MM, Rumyantseva T, Mücke VT, Schwarzkopf K, Joshi S, Kempf VA, et al. 2018; Bacterial infection-triggered acute-on-chronic liver failure is associated with increased mortality. Liver Int. 38:645–53. DOI: 10.1111/liv.13568. PMID: 28853199.
Article8. Jalan R, Fernandez J, Wiest R, Schnabl B, Moreau R, Angeli P, et al. 2014; Bacterial infections in cirrhosis: a position statement based on the EASL Special Conference 2013. J Hepatol. 60:1310–24. DOI: 10.1016/j.jhep.2014.01.024. PMID: 24530646.
Article9. Oliveira AM, Branco JC, Barosa R, Rodrigues JA, Ramos L, Martins A, et al. 2016; Clinical and microbiological characteristics associated with mortality in spontaneous bacterial peritonitis: a multicenter cohort study. Eur J Gastroenterol Hepatol. 28:1216–22. DOI: 10.1097/MEG.0000000000000700. PMID: 27391170.10. Ihn K, Kang JM, Kim EJ, Lee J, Lee JG, Joo DJ, et al. 2020; Postoperative bacteremia is associated with early vascular complications in pediatric liver transplant recipients with biliary atresia. Korean J Transplant. 34(Suppl 1):S123. DOI: 10.4285/ATW2020.OR-1170.
Article11. Kim T, Yeo HJ, Kim DH, Jang JH, Son E, Jang JO, et al. 2020; Prognostic impact of perioperative sputum colonization on early outcome after lung transplant. Korean J Transplant. 34(Suppl 1):S174. DOI: 10.4285/ATW2020.OP-1155.
Article12. Fernández J, Ruiz del Arbol L, Gómez C, Durandez R, Serradilla R, Guarner C, et al. 2006; Norfloxacin vs ceftriaxone in the prophylaxis of infections in patients with advanced cirrhosis and hemorrhage. Gastroenterology. 131:1049–56. DOI: 10.1053/j.gastro.2006.07.010. PMID: 17030175.
Article13. Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, et al. 2013; Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 144:1426–37. DOI: 10.1053/j.gastro.2013.02.042. PMID: 23474284.
Article14. Bruns T, Zimmermann HW, Stallmach A. 2014; Risk factors and outcome of bacterial infections in cirrhosis. World J Gastroenterol. 20:2542–54. DOI: 10.3748/wjg.v20.i10.2542. PMID: 24627590. PMCID: PMC3949263.
Article15. Arvaniti V, D'Amico G, Fede G, Manousou P, Tsochatzis E, Pleguezuelo M, et al. 2010; Infections in patients with cirrhosis increase mortality four-fold and should be used in determining prognosis. Gastroenterology. 139:1246–56. DOI: 10.1053/j.gastro.2010.06.019. PMID: 20558165.
Article