Korean J Transplant.
2021 Sep;35(3):183-188. 10.4285/kjt.20.0059.
Hepatic artery reconstruction using interposition of autologous saphenous vein conduit for living donor liver transplantation: a case report
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2520684
- DOI: http://doi.org/10.4285/kjt.20.0059
Abstract
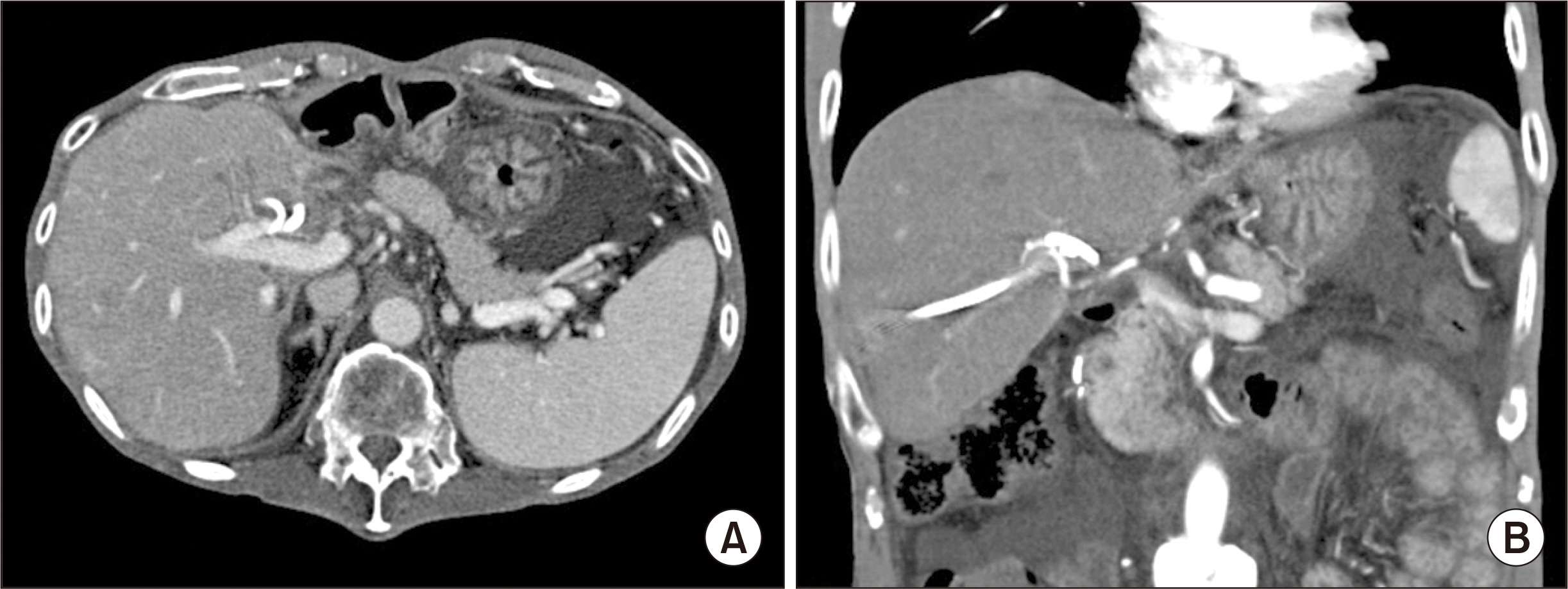
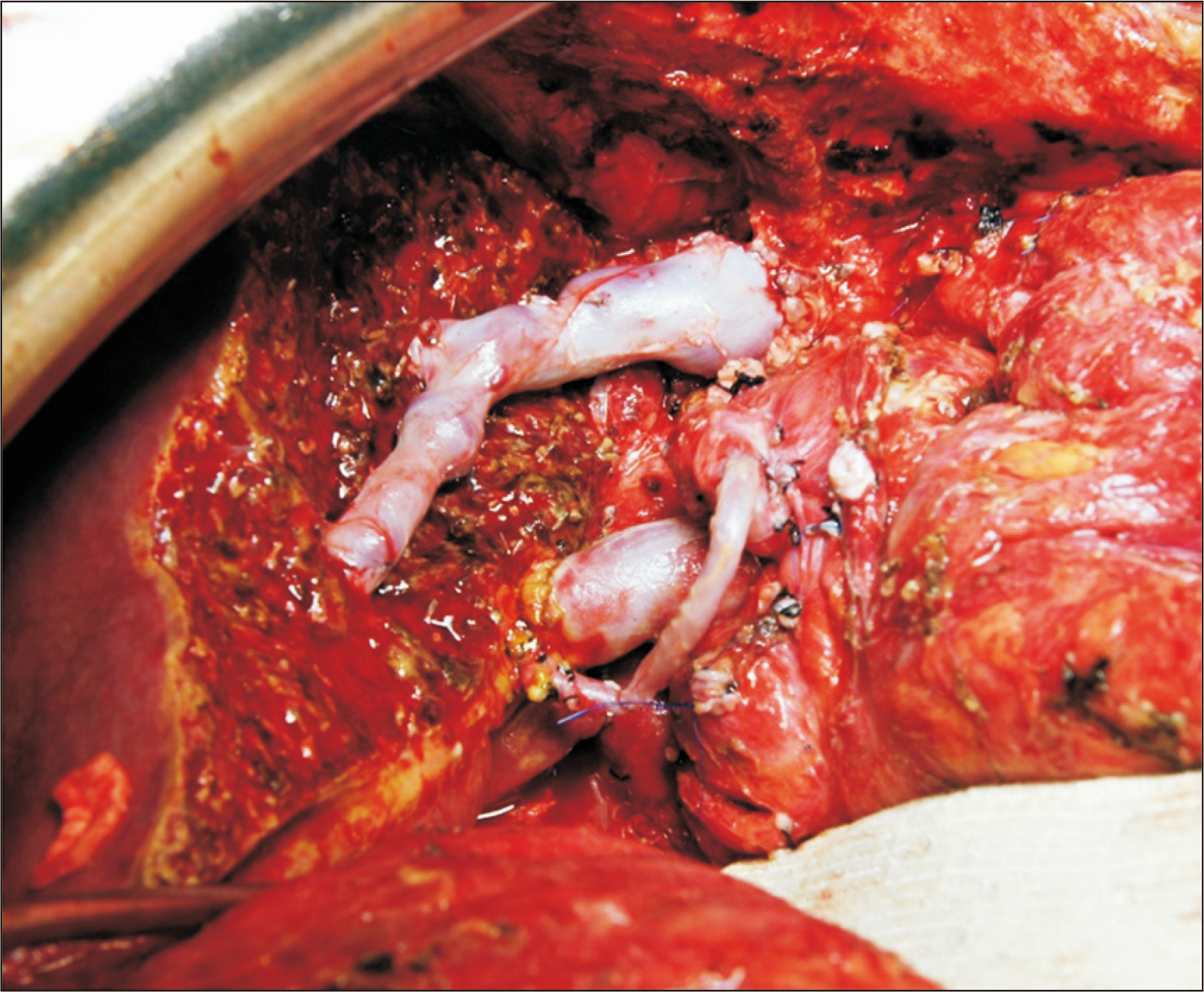
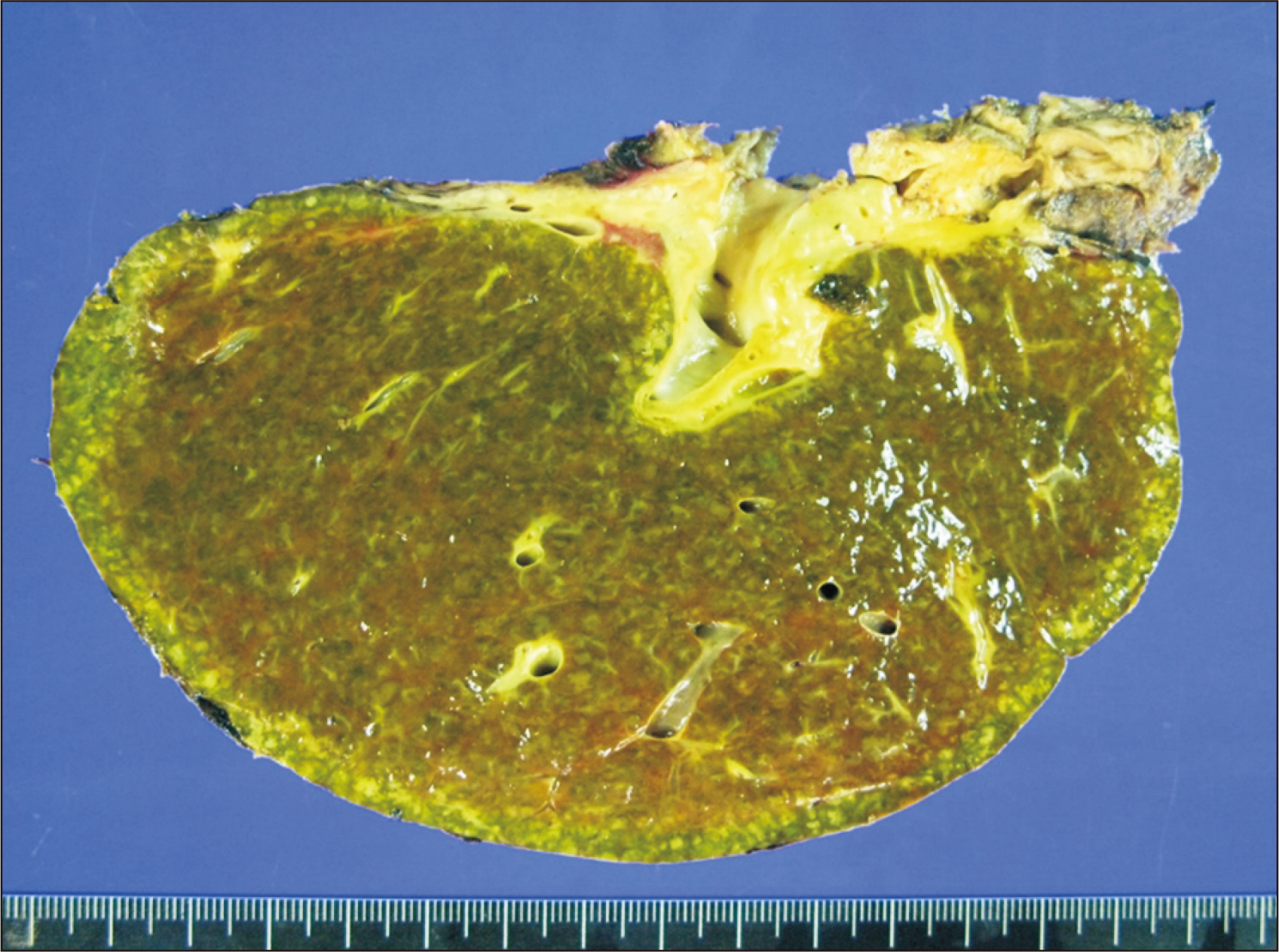
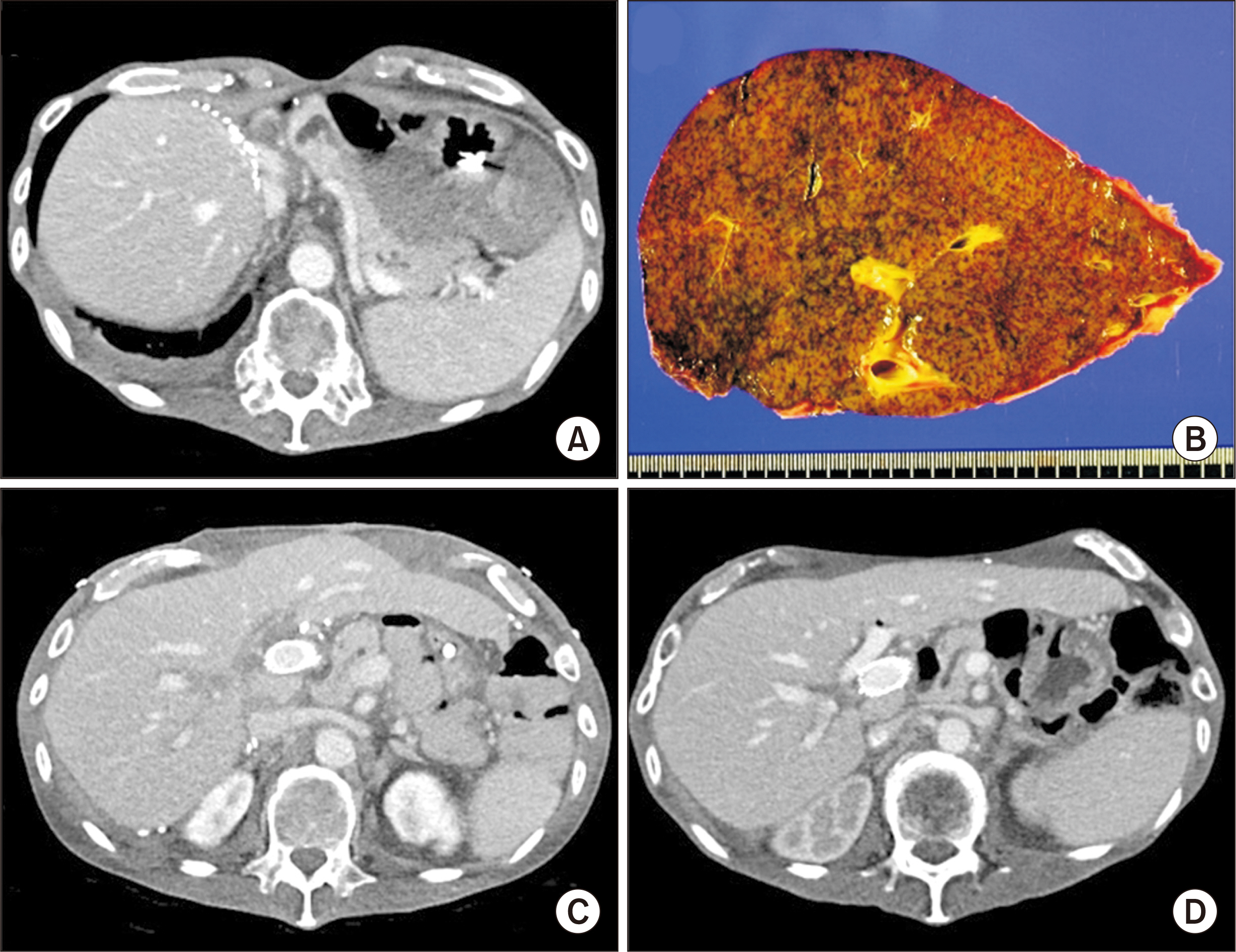
- We have preferentially used the right gastroepiploic artery (RGEA) as an alternative for the recipient hepatic artery (HA) inflow during living donor liver transplantation (LDLT), but it was not always available. We herein present a case of adult LDLT with HA reconstruction using a greater saphenous vein (GSV) conduit because of the absence of the RGEA due to prior subtotal gastrectomy. A 55-year-old male patient diagnosed with hepatitis B virus-associated liver cirrhosis and secondary biliary cirrhosis underwent LDLT using a modified right liver graft. The upper abdominal cavity was heavily adhered due to prior abdominal surgeries, thus we had to sacrifice the common bile duct and the right HA completely. A 6-cm-long GSV segment was harvested from the left ankle and interposed between the recipient gastroduodenal artery and the graft HA. The patient recovered from LDLT and HA complications did not occur. However, 8 years after LDLT, chronic rejection occurred, thus repeated deceased donor liver transplantation was performed. This patient has been doing well for 2 years after retransplantation. In conclusion, we suggest that interposition of an autologous GSV conduit can be an alternative for establishing HA inflow in LDLT when other inflow source is not available.
Keyword
Figure
Reference
-
1. Ahn CS, Hwang S, Moon DB, Song GW, Ha TY, Park GC, et al. 2012; Right gastroepiploic artery is the first alternative inflow source for hepatic arterial reconstruction in living donor liver transplantation. Transplant Proc. 44:451–3. DOI: 10.1016/j.transproceed.2012.01.057. PMID: 22410041.
Article2. Park GC, Moon DB, Kang SH, Ahn CS, Hwang S, Kim KH, et al. 2019; Overcoming hepatic artery thrombosis after living donor liver transplantations: an experience from Asan Medical Center. Ann Transplant. 24:588–93. DOI: 10.12659/AOT.919650. PMID: 31672958. PMCID: PMC6857352.
Article3. Uchiyama H, Shirabe K, Taketomi A, Soejima Y, Ninomiya M, Kayashima H, et al. 2010; Extra-anatomical hepatic artery reconstruction in living donor liver transplantation: can this procedure save hepatic grafts? Liver Transpl. 16:1054–61. DOI: 10.1002/lt.22119. PMID: 20818743.
Article4. Bhatti AB, Dar FS, Qureshi AI, Haider S, Khan NA. 2019; Saphenous vein conduits for hepatic arterial reconstruction in living donor liver transplantation. Langenbecks Arch Surg. 404:293–300. DOI: 10.1007/s00423-019-01774-1. PMID: 30859361.
Article5. Tranbaugh RF, Schwann TA, Swistel DG, Dimitrova KR, Al-Shaar L, Hoffman DM, et al. 2017; Coronary artery bypass graft surgery using the radial artery, right internal thoracic artery, or saphenous vein as the second conduit. Ann Thorac Surg. 104:553–9. DOI: 10.1016/j.athoracsur.2016.11.017. PMID: 28215422.6. Gaudino M, Taggart D, Suma H, Puskas JD, Crea F, Massetti M. 2015; The choice of conduits in coronary artery bypass surgery. J Am Coll Cardiol. 66:1729–37. DOI: 10.1016/j.jacc.2015.08.395. PMID: 26449144.
Article7. Furukawa H, Yamane N, Honda T, Yamasawa T, Kanaoka Y, Tanemoto K. 2019; Angiographic appearance of patent saphenous vein graft 32 years after coronary artery bypass grafting. Circ J. 83:840. DOI: 10.1253/circj.CJ-18-0851. PMID: 30224588.
Article8. Queiroz RM, Nastri R Filho, Ferez MA, Costa MJ, Laguna CB, Valentin MV. 2017; Thrombosed aneurysm of saphenous vein coronary artery bypass grafting. Rev Assoc Med Bras (1992). 63:488–91. DOI: 10.1590/1806-9282.63.06.488. PMID: 28876423.
Article9. Dubois CL, Vandervoort PM. 2001; Aneurysms and pseudoaneurysms of coronary arteries and saphenous vein coronary artery bypass grafts: a case report and literature review. Acta Cardiol. 56:263–7. DOI: 10.2143/AC.56.4.2005656. PMID: 11573835.10. Li PC, Thorat A, Jeng LB, Yang HR, Li ML, Yeh CC, et al. 2017; Successful application of supraceliac aortohepatic conduit using saphenous venous graft in right Lobe living donor liver transplantation. Liver Transpl. 23:976–80. DOI: 10.1002/lt.24720. PMID: 28073174.
Article11. Baimakhanov Z, Magauina A, Matkerimov A, Kaniev S, Doskhanov M, Serikuly E, et al. 2019; Extra-anatomic jump graft arterial reconstruction using a great saphenous vein autograft during living donor liver transplantation. Transplant Proc. 51:3120–3. DOI: 10.1016/j.transproceed.2019.07.004. PMID: 31611118.
Article12. de Rueda F, Souza D, Lima Rde C, Menezes A, Johansson B, Dashwood M, et al. 2008; Novel no-touch technique of harvesting the saphenous vein for coronary artery bypass grafting. Arq Bras Cardiol. 90:356–62.13. Kan CD, Luo CY, Yang YJ. 1999; Endoscopic saphenous vein harvest decreases leg wound complication in coronary artery bypass grafting patients. J Card Surg. 14:157–62. DOI: 10.1111/j.1540-8191.1999.tb00969.x. PMID: 10789700.
Article14. Felisky CD, Paull DL, Hill ME, Hall RA, Ditkoff M, Campbell WG, et al. 2002; Endoscopic greater saphenous vein harvesting reduces the morbidity of coronary artery bypass surgery. Am J Surg. 183:576–9. DOI: 10.1016/S0002-9610(02)00835-8.
Article15. Bitondo JM, Daggett WM, Torchiana DF, Akins CW, Hilgenberg AD, Vlahakes GJ, et al. 2002; Endoscopic versus open saphenous vein harvest: a comparison of postoperative wound complications. Ann Thorac Surg. 73:523–8. DOI: 10.1016/S0003-4975(01)03334-3.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical applicability of autologous great saphenous vein for living donor liver transplantation
- Usability of cryopreserved homologous great saphenous vein for hepatobiliarypancreatic surgery and living donor liver transplantation
- Hepatic Artery Reconstruction Using the Right Gastroepiploic Artery for Hepatic Artery Inflow in a Living Donor Liver Transplantation
- Experience with Microsurgical Reconstruction of the Hepatic Artery in 100 Living Donor Liver Transplantation
- Standardized surgical techniques for adult living donor liver transplantation using a modified right lobe graft: a video presentation from bench to reperfusion