Nutr Res Pract.
2021 Oct;15(5):655-671. 10.4162/nrp.2021.15.5.655.
Plate waste study among hospitalised patients receiving texture-modified diet
- Affiliations
-
- 1Dietetics Programme & Centre for Healthy Aging and Wellness (H-CARE), Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur 50300, Malaysia
- KMID: 2520666
- DOI: http://doi.org/10.4162/nrp.2021.15.5.655
Abstract
- BACKGROUND/OBJECTIVES
While plate waste has been widely investigated in hospitals, there have been minimal studies specific to the texture-modified diet (TMD). This study aims to determine the percentage of plate waste among patients prescribed with TMD and its contributory factors.
SUBJECTS/METHODS
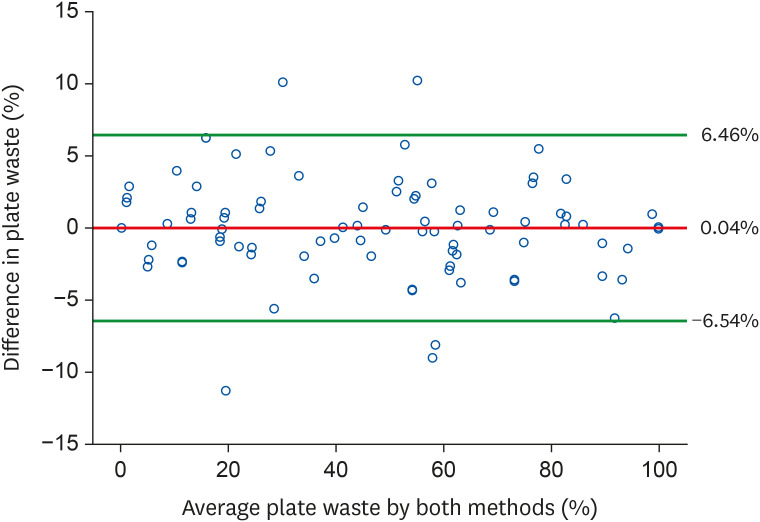
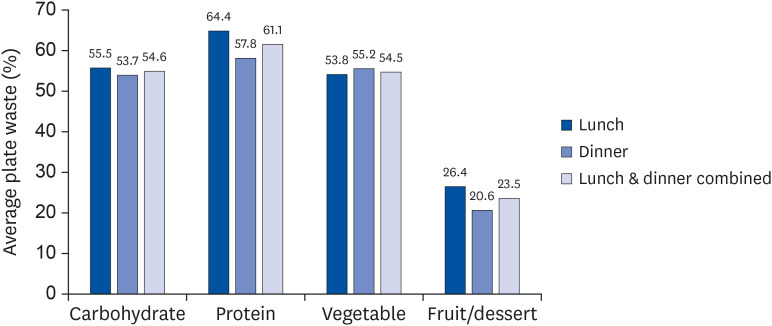
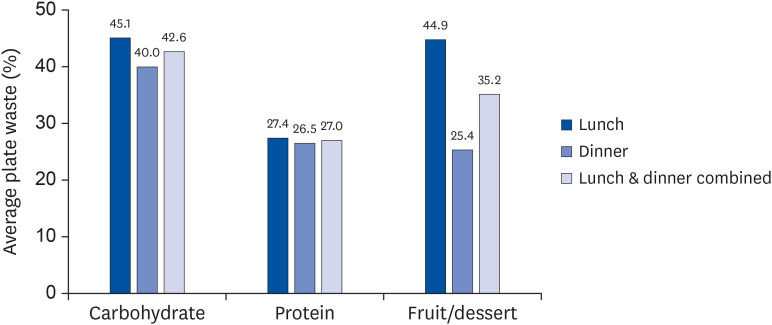
This was a single-centre study conducted in the university hospital on three types of TMD (blended diet, mixed porridge, minced diet) during lunch and dinner meals. Weighing method and visual estimation method assisted by digital photograph were adopted in this study. Face to face interview was carried out to investigate on 1) the food/ food service quality factors in terms of patients' satisfaction level towards sensorial quality of food and food services provided and 2) the clinical/external factors including appetite, the provision of oral nutrition support, time taking the diet, the need for feeding assistance and the length of hospital stay.
RESULTS
The mean percentage of overall plate waste of 95 patients receiving TMD was high (47.5%). Blended diet was identified as the most wasted diet (65%) followed by minced diet (56%) and mixed porridge (35%). Satisfaction level among patients was moderate. Patients on TMD in general had higher satisfaction level on the aspect of food service as compared to food quality. Substantial association between sensorial qualities of food and plate waste were varied according to individual TMD type. A multiple linear regression showed that only the satisfaction level toward the aspects of appearance and variety of foods were the predictors of TMD plate waste (R 2 = 0.254, P < 0.05).
CONCLUSIONS
A significant relationship between the percentage of plate waste and the overall satisfaction level of patients receiving TMD suggests that vigorous strategies are needed to reduce the food waste of TMD which will lead to a better nutritional status and clinical outcomes among the patients.
Figure
Reference
-
1. Gustavsson J, Cederberg C, Sonesson U, Van Otterdijk R, Meybeck A. Global Food Losses and Food Waste. Rome: Food and Agriculture Organization of the United Nations;2011.2. Goonan S, Mirosa M, Spence H. Getting a taste for food waste: a mixed methods ethnographic study into hospital food waste before patient consumption conducted at three New Zealand foodservice facilities. J Acad Nutr Diet. 2014; 114:63–71. PMID: 24231365.
Article3. Comstock EM, St Pierre RG, Mackiernan YD. Measuring individual plate waste in school lunches. Visual estimation and children's ratings vs. actual weighing of plate waste. J Am Diet Assoc. 1981; 79:290–296. PMID: 7264115.4. Yang Z, Koh SK, Ng WC, Lim RCJ, Tan HTW, Tong YW, Dai Y, Chong C, Wang CH. Potential application of gasification to recycle food waste and rehabilitate acidic soil from secondary forests on degraded land in Southeast Asia. J Environ Manage. 2016; 172:40–48. PMID: 26921564.
Article5. Alam MM, Sujauddin M, Iqbal GMA, Huda SMS. Report: healthcare waste characterization in Chittagong Medical College Hospital, Bangladesh. Waste Manag Res. 2008; 26:291–296. PMID: 18649578.
Article6. Williams P, Walton K. Plate Waste in Hospitals and Strategies for Change. Amsterdam: Elsevier;2011.7. Alshqaqeeq F, Twomey JM, Overcash MR. Food waste in hospitals. Int J Healthc Technol Manag. 2018; 17:186–196.8. Ofei KT, Holst M, Rasmussen HH, Mikkelsen BE. How practice contributes to trolley food waste. A qualitative study among staff involved in serving meals to hospital patients. Appetite. 2014; 83:49–56. PMID: 25108237.
Article9. Zakiah L, Saimy I, Hamid MA. Plate waste among hospital inpatients. Malays J Public Health Med. 2005; 5:19–24.10. Edwards JS, Hartwell HJ. Hospital food service: a comparative analysis of systems and introducing the ‘Steamplicity’ concept. J Hum Nutr Diet. 2006; 19:421–430. PMID: 17105539.
Article11. Gomes GS, Jorge MN. Rest-ingestion and waste index assessment at a commercial meal production unit in Ipatinga-MG. Nutri Gerais. 2012; 6:857–868.12. Simzari K, Vahabzadeh D, Nouri Saeidlou S, Khoshbin S, Bektas Y. Food intake, plate waste and its association with malnutrition in hospitalized patients. Nutr Hosp. 2017; 34:1376–1381. PMID: 29280654.
Article13. Sahin B, Demir C, Aycicek H, Cihangiroglu N. Evaluation of factors affecting the food consumption levels of inpatients in a Turkish armed forces training hospital. Food Qual Prefer. 2007; 18:555–559.
Article14. Sahin B, Demir C, Celik Y, Teke AK. Factors affecting satisfaction level with the food services in a military hospital. J Med Syst. 2006; 30:381–387. PMID: 17069001.
Article15. Valero Díaz A, Caracuel García A. Evaluation of factors affecting plate waste of inpatients in different healthcare settings. Nutr Hosp. 2013; 28:419–427. PMID: 23822694.16. Sonnino R, McWilliam S. Food waste, catering practices and public procurement: a case study of hospital food systems in Wales. Food Policy. 2011; 36:823–829.
Article17. Stanga Z, Zurflüh Y, Roselli M, Sterchi AB, Tanner B, Knecht G. Hospital food: a survey of patients' perceptions. Clin Nutr. 2003; 22:241–246. PMID: 12765662.
Article18. Kandiah J, Stinnett L, Lutton D. Visual plate waste in hospitalized patients: length of stay and diet order. J Am Diet Assoc. 2006; 106:1663–1666. PMID: 17000200.
Article19. Walton K, Williams P, Tapsell L. What do stakeholders consider the key issues affecting the quality of foodservice provision for long-stay patients? J Foodserv. 2006; 17:212–225.
Article20. Royal College of Speech and Language Therapists. Communicating Quality 3: RCSLT's Guidance on Best Practice in Service Organisation and Provision. 2nd ed. London: Royal College of Speech and Language Therapists;2006.21. Aguilera JM, Park DJ. Texture-modified foods for the elderly: status, technology and opportunities. Trends Food Sci Technol. 2016; 57:156–164.
Article22. Cichero JA, Steele C, Duivestein J, Clavé P, Chen J, Kayashita J, Dantas R, Lecko C, Speyer R, Lam P, Murray J. The need for international terminology and definitions for texture-modified foods and thickened liquids used in dysphagia management: foundations of a global initiative. Curr Phys Med Rehabil Rep. 2013; 1:280–291. PMID: 24392282.
Article23. Yoshioka K, Yamamoto A, Matsushima Y, Hachisuka K, Ikeuchi Y. Effects of high pressure on the textural and sensory properties of minced fish meat gels for the dysphagia diet. Food Nutr Sci. 2016; 7:732–742.24. Wright L, Cotter D, Hickson M, Frost G. Comparison of energy and protein intakes of older people consuming a texture modified diet with a normal hospital diet. J Hum Nutr Diet. 2005; 18:213–219. PMID: 15882384.
Article25. Puruhita N, Armeidani R, Kusumadewi A. Modifikasi tekstur makanan dan minuman pasien disfagia. Med Hosp. 2016; 3:207–212.
Article26. Goes VF, Mello-Carpes PB, de Oliveira LO, Hack J, Magro M, Bonini JS. Evaluation of dysphagia risk, nutritional status and caloric intake in elderly patients with Alzheimer's. Rev Lat Am Enfermagem. 2014; 22:317–324. PMID: 26107841.
Article27. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–2763. PMID: 16269630.28. Ministry of Health Malaysia. Manual Diet Hospital. Kuala Lumpur: Dietetics and Food Service Unit, Ministry of Health Malaysia;2016.29. Cichero JA, Lam P, Steele CM, Hanson B, Chen J, Dantas RO, Duivestein J, Kayashita J, Lecko C, Murray J, Pillay M, Riquelme L, Stanschus S. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: the IDDSI framework. Dysphagia. 2017; 32:293–314. PMID: 27913916.
Article30. IDDSI. International Dysphagia Diet Standardization Initiative [Internet]. place unknown: IDDSI;2016. cited 2019 August 3. Available from:https://iddsi.org.31. Massoulard A, Bonnabau H, Gindre-Poulvelarie L, Baptistev A, Preux PM, Villemonteix C, Javerliat V, Fraysse JL, Desport JC. Analysis of the food consumption of 87 elderly nursing home residents, depending on food texture. J Nutr Health Aging. 2011; 15:192–195. PMID: 21369666.
Article32. Bannerman E, McDermott K. Dietary and fluid intakes of older adults in care homes requiring a texture modified diet: the role of snacks. J Am Med Dir Assoc. 2011; 12:234–239. PMID: 21333927.
Article33. Germain I, Dufresne T, Gray-Donald K. A novel dysphagia diet improves the nutrient intake of institutionalized elders. J Am Diet Assoc. 2006; 106:1614–1623. PMID: 17000194.
Article34. Dahl WJ, Whiting SJ, Tyler RT. Protein content of puréed diets: implications for planning. Can J Diet Pract Res. 2007; 68:99–102. PMID: 17553196.
Article35. Shahar S, Pooy NS. Predictive equations for estimation of stature in Malaysian elderly people. Asia Pac J Clin Nutr. 2003; 12:80–84. PMID: 12737015.36. Ross Laboratories. The Ross Knee Height Caliper. The IP com Prior Art Database. Columbus (OH): Ross Laboratories;2002.37. Joung HW, Kim HS, Yuan JJ, Huffman L. Service quality, satisfaction, and behavioral intention in home delivered meals program. Nutr Res Pract. 2011; 5:163–168. PMID: 21556231.
Article38. Khalib MKN, Manaf ZA, Shahar S, Ludin AFM. Delivery of healthy lunch to worksites: a two weeks pilot study in a sample of working adults in Selangor, Malaysia. Malays J Nutr. 2018; 24:575–585.39. Amano N, Nakamura T. Accuracy of the visual estimation method as a predictor of food intake in Alzheimer's patients provided with different types of food. Clin Nutr ESPEN. 2018; 23:122–128. PMID: 29460787.
Article40. Bjornsdottir R, Oskarsdottir ES, Thordardottir FR, Ramel A, Thorsdottir I, Gunnarsdottir I. Validation of a plate diagram sheet for estimation of energy and protein intake in hospitalized patients. Clin Nutr. 2013; 32:746–751. PMID: 23305605.
Article41. Holdt CS, Sitter K, Gates GE. Comparison of plate waste estimation measures in a pediatric hospital. Food Res Int. 1993; 7:81–91.
Article42. Anasako Y, Akamatsu R. A systematic review of the reliability and validity of the visual estimation method to measure plate waste in food service facilities. Jpn J Nutr Diet. 2014; 72:181–192.
Article43. Edwards J, Nash A. Catering services. Measuring the wasteline. Health Serv J. 1997; 107:26–27.44. Dias-Ferreira C, Santos T, Oliveira V. Hospital food waste and environmental and economic indicators--a Portuguese case study. Waste Manag. 2015; 46:146–154. PMID: 26427934.45. Aminuddin NF, Vijayakumaran RK, Abdul Razak S. Patient satisfaction with hospital foodservice and its impact on plate waste in public hospitals in East Malaysia. Hosp Pract Res. 2018; 3:90–97.46. Nowson CA, Sherwin AJ, McPhee JG, Wark JD, Flicker L. Energy, protein, calcium, vitamin D and fibre intakes from meals in residential care establishments in Australia. Asia Pac J Clin Nutr. 2003; 12:172–177. PMID: 12810407.47. Keawkaika S, Suzuki K, Hagura Y. Determination of viscoelastic properties of rice porridge by the non-rotational concentric cylinder method. Food Sci Technol Res. 2010; 16:23–30.
Article48. Shahar S, Chee KY, Wan Chik WC. Food intakes and preferences of hospitalised geriatric patients. BMC Geriatr. 2002; 2:3. PMID: 12165100.
Article49. Tamby Chik C, Adilah Zulkiply N, Bachok S, Mohi Z, Mohd Shahril A. Plate waste in public hospitals foodservice management in Selangor, Malaysia. Indian J Sci Technol. 2019; 11:1–5.50. Ballou Stahlman L, Mertz Garcia J, Hakel M, Chambers E 4th. Comparison ratings of pureed versus molded fruits: preliminary results. Dysphagia. 2000; 15:2–5. PMID: 10594251.
Article51. Donini LM, Castellaneta E, De Guglielmi S, De Felice MR, Savina C, Coletti C, Paolini M, Cannella C. Improvement in the quality of the catering service of a rehabilitation hospital. Clin Nutr. 2008; 27:105–114. PMID: 18063444.
Article52. Valero Díaz A, Caracuel García Á. Evaluation of factors affecting plate waste of inpatients in different healthcare settings. Nutr Hosp. 2013; 28:419–427. PMID: 23822694.53. Cereda E, Pedrolli C. Food waste: other issues and settings should be considered. Nutr Bull. 2009; 34:238–239.54. Abdelhafez AM, Al Qurashi L, Al Ziyadi R, Kuwair A, Shobki M, Mograbi H. Analysis of factors affecting the satisfaction levels of patients toward food services at general hospitals in Makkah, Saudi Arabia. Am J Med Med Sci. 2012; 2:123–130.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Factors Affecting Plate Waste and Its Effects in Normal & Soft Diets Provided from Hospital Foodservice
- Elementary School Students' Perception of Food Waste and Factors Affecting Plate Waste Rate of School Foodservice in the Gyeongnam Area
- Dieticians' Perception of Current Status of No-plate-waste Day in School Lunch
- Generation of Food Waste and Plate Waste Reduction Strategies in School Food Services in Gyeonggi Province
- Assessment of the nutritional value of the plate waste generated in School Foodservices in Kyungbuk Area