Clin Endosc.
2021 Sep;54(5):713-721. 10.5946/ce.2021.016.
Endoscopic Stenting for Malignant Biliary Obstruction: Results of a Nationwide Experience
- Affiliations
-
- 1Department of Clinical Sciences, Intervention and Technology, Centre for Digestive Diseases, Karolinska Institutet, Karolinska University Hospital, Stockholm, Sweden
- 2University of Stellenbosch, Department of Surgical Sciences, Division of Surgery, Tygerberg Hospital, Bellville, South Africa
- 3Department of Clinical Science and Education Södersjukhuset, Karolinska Institutet, Department of Surgery, Södersjukhuset, Stockholm, Sweden
- 4Department of Surgical and Perioperative Sciences, Umeå University, Umeå University Hospital, Umeå, Sweden
- 5Department of Surgery, University of Cape Town Faculty of Health Sciences, Surgical Gastroenterology Unit, Groote Schuur Hospital, Cape Town, Bellville, South Africa
- KMID: 2520555
- DOI: http://doi.org/10.5946/ce.2021.016
Abstract
- Background/Aims
Many unanswered questions remain about the treatment of malignant hilar obstruction. We investigated endoscopic stenting for malignant biliary strictures, as reported in a nationwide registry.
Methods
All endoscopic retrograde cholangiopancreatography (ERCP) procedures entered in the Swedish Registry of Gallstone Surgery and ERCP from January 2010 to December 2017 in which stenting was performed for malignant biliary stricture management were included in this study. Patency was estimated by determining the time to reintervention.
Results
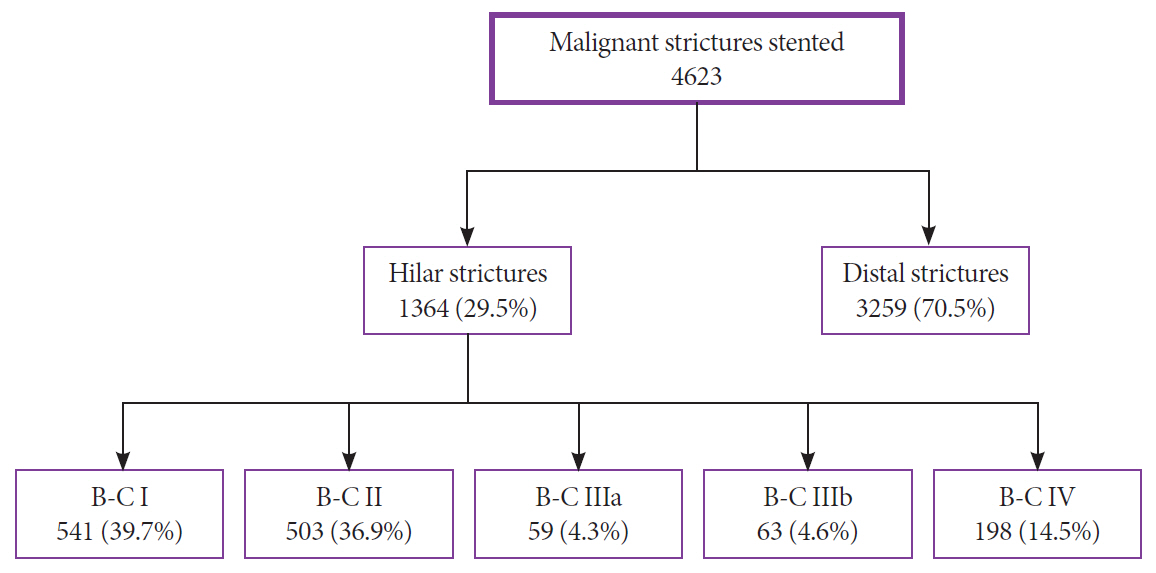
Endoscopic stenting was performed for malignant stricture management in 4623 ERCP procedures, of which 1364 (29.5%) were performed for hilar strictures. Of the hilar strictures, 320 (23.5%) were intrahepatic strictures (Bismuth–Corlette III–IV). Adverse events were more common after hilar stenting than after distal stenting (17.2% vs. 12.0%, p<0.0001). The 6-month reintervention rate was 73.4% after hilar stenting compared with 55.9% after distal stenting (p<0.0001). The 6-month reintervention rates for Bismuth–Corlette types I, II, IIIa, IIIb, and IV were 70.4%, 75.6%, 90.0%, 87.5%, and 85.7%, respectively. In multivariate analysis, the risk for reintervention was three times higher after hilar stenting than after distal stenting (hazard ratio 3.47, 95% confidence interval 2.01–6.00, p<0.001).
Conclusions
This study with a relatively large patient cohort undergoing endoscopic stenting confirms that stenting for malignant hilar obstruction has more adverse events and lower patency than stenting for distal malignant obstruction.
Keyword
Figure
Cited by 1 articles
-
Endoscopic Biliary Drainage for Hilar Obstruction: Further Evidence But Still A Long Way To Go
Yousuke Nakai
Clin Endosc. 2021;54(5):629-630. doi: 10.5946/ce.2021.158.
Reference
-
1. Almadi MA, Barkun A, Martel M. Plastic vs. self-expandable metal stents for palliation in malignant biliary obstruction: a series of meta-analyses. Am J Gastroenterol. 2017; 112:260–273.
Article2. Hong W, Chen X, Wu W-Z, Zhu Q, Chen X. Metal versus plastic stents for malignant biliary obstruction: an update meta-analysis. Clin Res Hepatol Gastroenterol. 2013; 37:496–500.
Article3. Tringali A, Hassan C, Rota M, Rossi M, Mutignani M, Aabakken L. Covered vs. uncovered self-expandable metal stents for malignant distal biliary strictures: a systematic review and meta-analysis. Endoscopy. 2018; 50:631–641.
Article4. Baer HU, Rhyner M, Stain SC, et al. The effect of communication between the right and left liver on the outcome of surgical drainage for jaundice due to malignant obstruction at the hilus of the liver. HPB Surg. 1994; 8:27–31.
Article5. Vienne A, Hobeika E, Gouya H, et al. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. Gastrointest Endosc. 2010; 72:728–735.
Article6. Ashat M, Arora S, Klair JS, Childs CA, Murali AR, Johlin FC. Bilateral vs unilateral placement of metal stents for inoperable high-grade hilar biliary strictures: a systemic review and meta-analysis. World J Gastroenterol. 2019; 25:5210–5219.
Article7. Aghaie Meybodi M, Shakoor D, Nanavati J, et al. Unilateral versus bilateral endoscopic stenting in patients with unresectable malignant hilar obstruction: a systematic review and meta-analysis. Endosc Int Open. 2020; 8:E281–E290.
Article8. Rystedt J, Montgomery A, Persson G. Completeness and correctness of cholecystectomy data in a national register--GallRiks. Scand J Surg. 2014; 103:237–244.
Article9. Enochsson L, Blohm M, Sandblom G, et al. Inversed relationship between completeness of follow-up and coverage of postoperative complications in gallstone surgery and ERCP: a potential source of bias in patient registers. BMJ Open. 2018; 8:e019551.
Article10. Bismuth H, Nakache R, Diamond T. Management strategies in resection for hilar cholangiocarcinoma. Ann Surg. 1992; 215:31–38.
Article11. Dumonceau J-M, Kapral C, Aabakken L, et al. ERCP-related adverse events: european society of gastrointestinal endoscopy (ESGE) guideline. Endoscopy. 2020; 52:127–149.
Article12. Isayama H, Hamada T, Yasuda I, et al. TOKYO criteria 2014 for transpapillary biliary stenting. Dig Endosc. 2015; 27:259–264.
Article13. Tyson GL, Ilyas JA, Duan Z, et al. Secular trends in the incidence of cholangiocarcinoma in the USA and the impact of misclassification. Dig Dis Sci. 2014; 59:3103–3110.
Article14. Dumonceau J-M, Tringali A, Papanikolaou IS, et al. Endoscopic biliary stenting: indications, choice of stents, and results: european society of gastrointestinal endoscopy (ESGE) clinical guideline - updated october 2017. Endoscopy. 2018; 50:910–930.
Article15. Sofi AA, Nawras A, Alaradi OH, Alastal Y, Khan MA, Lee WM. Does endoscopic sphincterotomy reduce the risk of post-endoscopic retrograde cholangiopancreatography pancreatitis after biliary stenting? A systematic review and meta-analysis. Dig Endosc. 2016; 28:394–404.
Article16. Moses PL, Alnaamani KM, Barkun AN, et al. Randomized trial in malignant biliary obstruction: plastic vs partially covered metal stents. World J Gastroenterol. 2013; 19:8638–8646.17. Schmidt A, Riecken B, Rische S, et al. Wing-shaped plastic stents vs. self-expandable metal stents for palliative drainage of malignant distal biliary obstruction: a randomized multicenter study. Endoscopy. 2015; 47:430–436.
Article18. Sangchan A, Kongkasame W, Pugkhem A, Jenwitheesuk K, Mairiang P. Efficacy of metal and plastic stents in unresectable complex hilar cholangiocarcinoma: a randomized controlled trial. Gastrointest Endosc. 2012; 76:93–99.
Article19. Zorrón Pu L, de Moura EGH, Bernardo WM, Baracat FI, et al. Endoscopic stenting for inoperable malignant biliary obstruction: a systematic review and meta-analysis. World J Gastroenterol. 2015; 21:13374–13385.20. De Palma GD, Galloro G, Siciliano S, Iovino P, Catanzano C. Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc. 2001; 53:547–553.
Article21. Lee TH, Kim TH, Moon JH, et al. Bilateral versus unilateral placement of metal stents for inoperable high-grade malignant hilar biliary strictures: a multicenter, prospective, randomized study (with video). Gastrointest Endosc. 2017; 86:817–827.22. Rerknimitr R, Kladcharoen N, Mahachai V, Kullavanijaya P. Result of endoscopic biliary drainage in hilar cholangiocarcinoma. J Clin Gastroenterol. 2004; 38:518–523.
Article23. Xia M-X, Wang S-P, Wu J, et al. The risk of acute cholangitis after endoscopic stenting for malignant hilar strictures: a large comprehensive study. J Gastroenterol Hepatol. 2020; 35:1150–1157.
Article24. Conio M, Mangiavillano B, Caruso A, et al. Covered versus uncovered self-expandable metal stent for palliation of primary malignant extrahepatic biliary strictures: a randomized multicenter study. Gastrointest Endosc. 2018; 88:283–291.e3.25. Mukai T, Yasuda I, Nakashima M, et al. Metallic stents are more efficacious than plastic stents in unresectable malignant hilar biliary strictures: a randomized controlled trial. J Hepatobiliary Pancreat Sci. 2013; 20:214–222.
Article26. Miura S, Kanno A, Masamune A, et al. Risk factors for recurrent biliary obstruction following placement of self-expandable metallic stents in patients with malignant perihilar biliary stricture. Endoscopy. 2016; 48:536–545.
Article27. Miyazaki M, Ohtsuka M, Miyakawa S, et al. Classification of biliary tract cancers established by the Japanese Society of Hepato-Biliary-Pancreatic Surgery: 3(rd) English edition. J Hepatobiliary Pancreat Sci. 2015; 22:181–196.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic ultrasound-guided biliary drainage in malignant distal biliary obstruction
- Endoscopic Biliary Stenting in Patients with Malignant Biliary Obstruction
- Bilateral Metallic Stenting in Malignant Hilar Obstruction
- Percutaneous Transhepatic Recanalization of Malignant Hilar Obstruction: A Possible Rescue for Early Failure of Endoscopic Y-Stenting
- Management of Malignant Biliary Obstruction Combined with Duodenal Obstruction