J Korean Foot Ankle Soc.
2021 Sep;25(3):117-125. 10.14193/jkfas.2021.25.3.117.
Magnetic Resonance Imaging Analysis of Biological Ligament Healing after Suture-Tape Augmentation for Chronic Lateral Ankle Instability
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Chungbuk National University, Cheongju, Korea
- KMID: 2520102
- DOI: http://doi.org/10.14193/jkfas.2021.25.3.117
Abstract
- Purpose
The aim of this study was to evaluate biological ligament healing quantitatively after suture-tape augmentation for chronic lateral ankle instability.
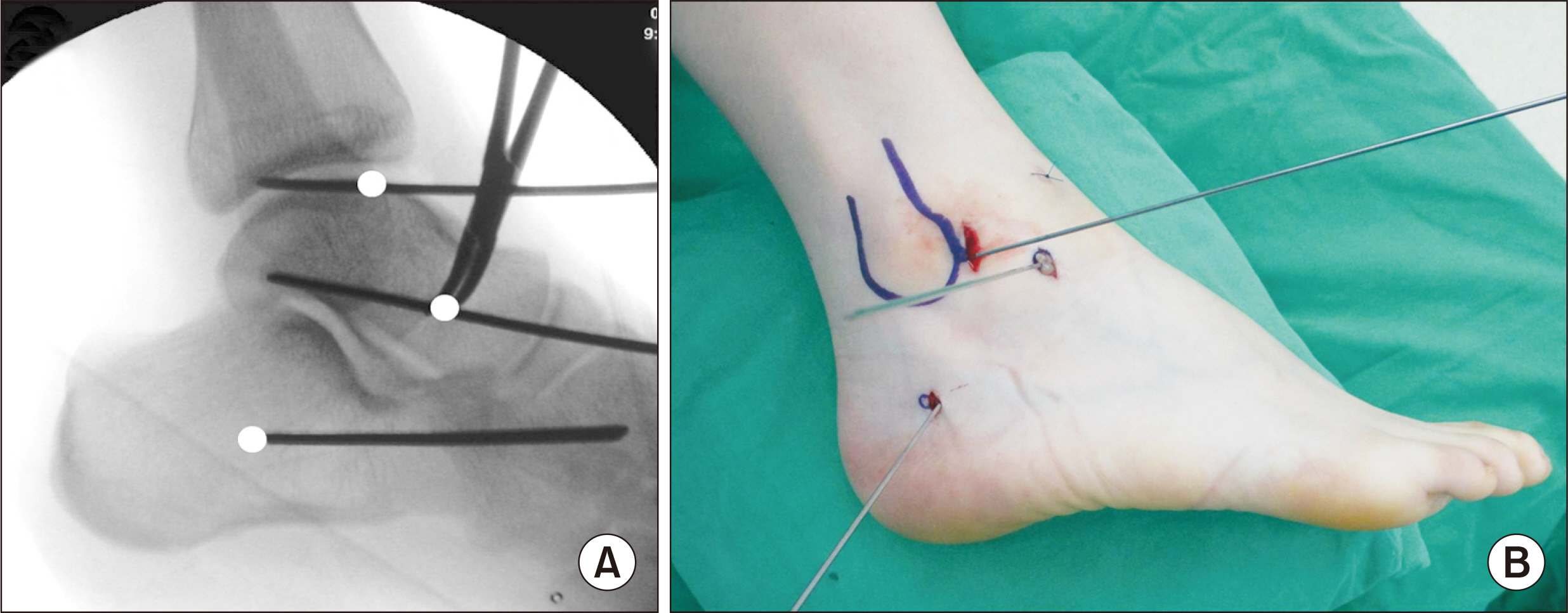
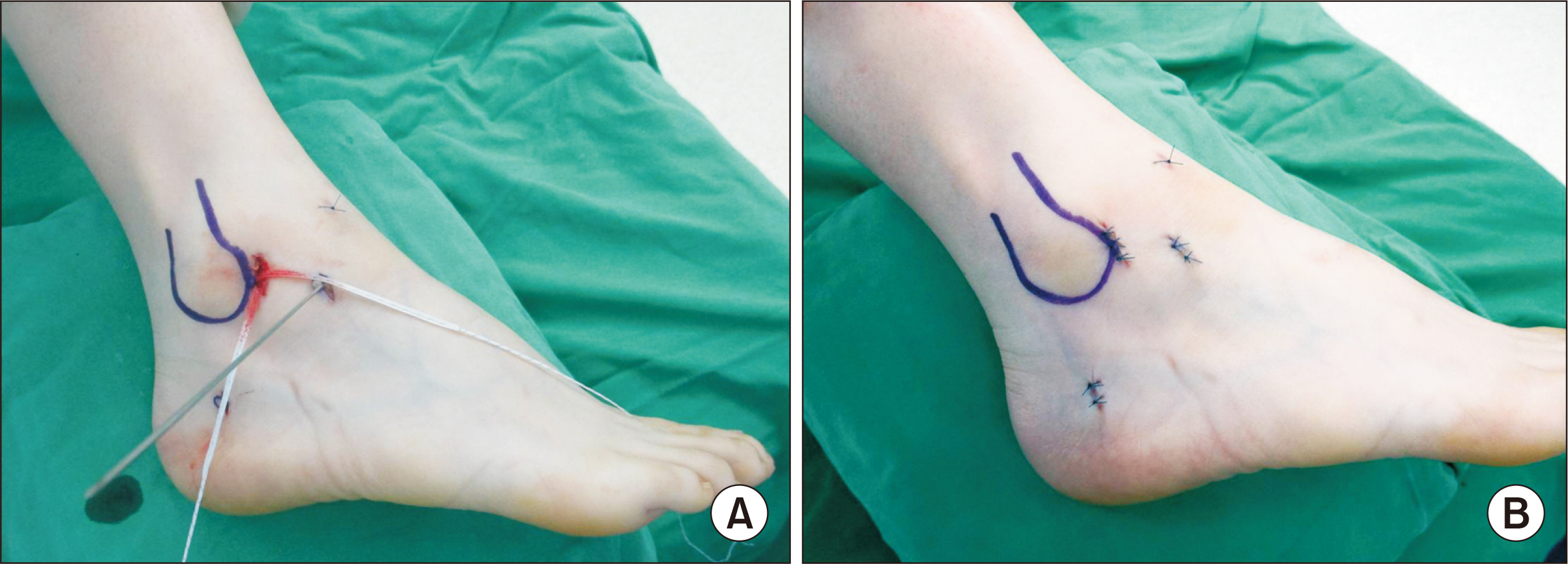
Materials and Methods
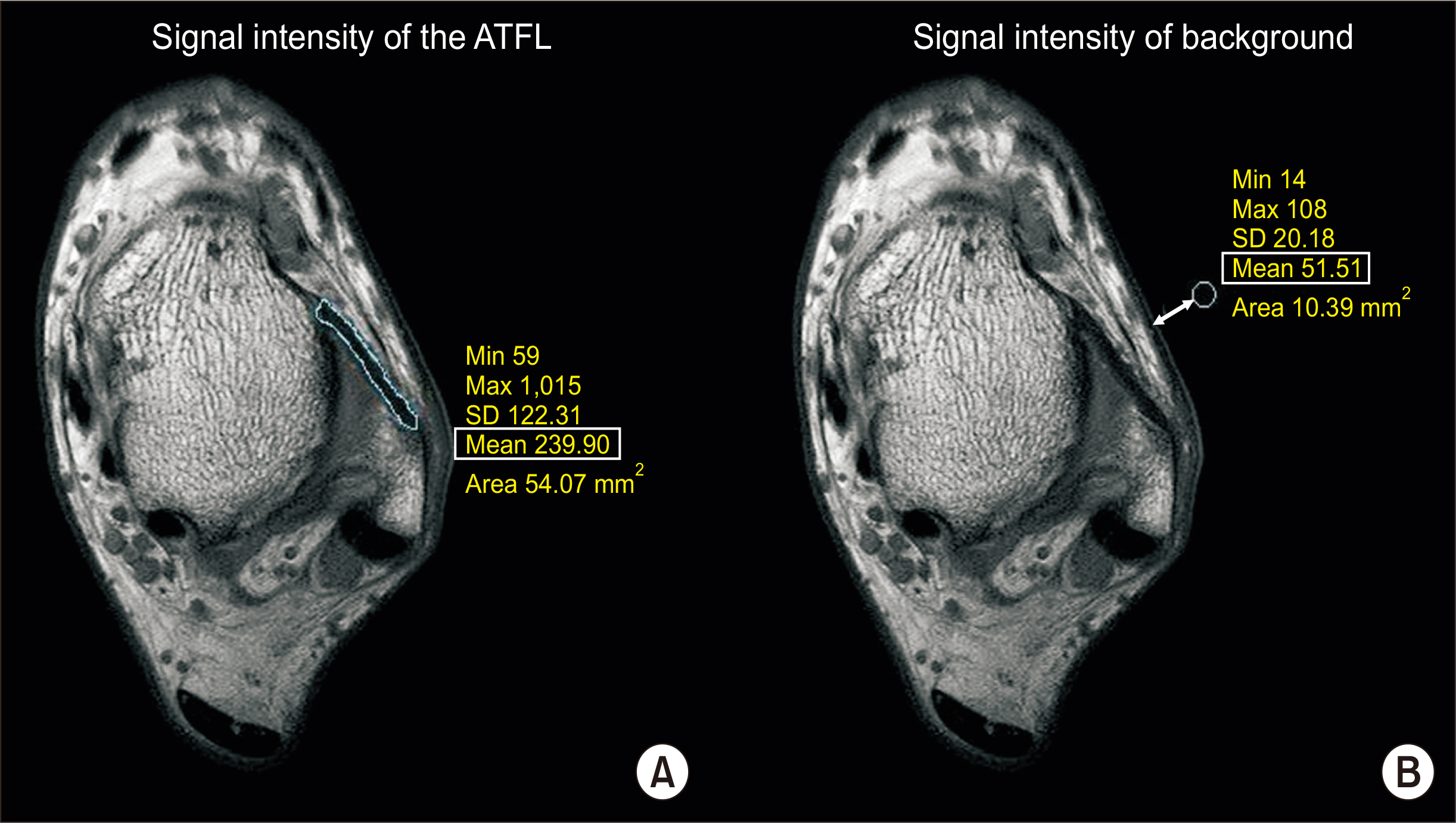
Thirty-two patients underwent magnetic resonance imaging (MRI) at a minimum of 2 years after lateral ligament augmentation using suture-tape. Signal/noise ratios (SNRs) and widths of anterior talofibular ligaments (ATFLs) were measured on preoperative and postoperative MRI by three researchers. ATFL biological healing degrees were analyzed using changes in SNRs and widths of ATFLs and by comparing these metrics with those of normal contralateral ankles. Clinical evaluations were performed using foot and ankle outcome scores (FAOSs), Foot and Ankle Ability Measure (FAAM) scores, and ankle stress radiographs.
Results
Mean FAOS and FAAM scores improved significantly from 62.4 to 93.6 and 58.3 to 92.3, respectively, at final follow-up (p<0.001). Mean SNRs and ATFL widths improved insignificantly from 8.49 to 8.21 and 2.07 to 2.15 mm, respectively, at final followup (p=0.424, p=0.718). Significant differences in mean SNRs and ATFL widths were found between ipsilateral and contralateral sides (p<0.001, p=0.002). Spearman’s correlation analysis revealed no significant association between clinical outcomes and degrees of biological healing of ATFLs based on MRI findings.
Conclusion
Despite improvements in clinical outcome measures, the effects of suture-tape augmentation for chronic lateral ankle instability on biological ligament healing were insignificant. In addition, no significant correlation was found between clinical outcomes and degrees of biological healing of ATFLs.
Keyword
Figure
Reference
-
1. O'Loughlin PF, Murawski CD, Egan C, Kennedy JG. 2009; Ankle instability in sports. Phys Sportsmed. 37:93–103. doi: 10.3810/psm.2009.06. DOI: 10.3810/psm.2009.06.1715. PMID: 20048515.2. Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT, et al. 2016; Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 50:1496–505. doi: 10.1136/bjsports-2016-096189. DOI: 10.1136/bjsports-2016-096189. PMID: 27259753.
Article3. DiGiovanni CW, Brodsky A. 2006; Current concepts: lateral ankle instability. Foot Ankle Int. 27:854–66. doi: 10.1177/107110070602701019. DOI: 10.1177/107110070602701019. PMID: 17054892.
Article4. Guelfi M, Zamperetti M, Pantalone A, Usuelli FG, Salini V, Oliva XM. 2018; Open and arthroscopic lateral ligament repair for treatment of chronic ankle instability: a systematic review. Foot Ankle Surg. 24:11–8. doi: 10.1016/j.fas.2016.05.315. DOI: 10.1016/j.fas.2016.05.315. PMID: 29413768.
Article5. Cho BK, Kim YM, Kim DS, Choi ES, Shon HC, Park KJ. 2012; Comparison between suture anchor and transosseous suture for the modified-Broström procedure. Foot Ankle Int. 33:462–8. doi: 10.3113/FAI.2012.0462. DOI: 10.3113/FAI.2012.0462. PMID: 22735317.
Article6. Baumhauer JF, O'Brien T. 2002; Surgical considerations in the treatment of ankle instability. J Athl Train. 37:458–62.7. Cho BK, Kim YM, Choi SM, Park HW, SooHoo NF. 2017; Revision anatomical reconstruction of the lateral ligaments of the ankle augmented with suture tape for patients with a failed Broström procedure. Bone Joint J. 99:1183–9. doi: 10.1302/0301-620X.99B9.BJJ-2017-0144.R1. DOI: 10.1302/0301-620X.99B9.BJJ-2017-0144.R1. PMID: 28860398.
Article8. Park KH, Lee JW, Suh JW, Shin MH, Choi WJ. 2016; Generalized ligamentous laxity is an independent predictor of poor outcomes after the modified Broström procedure for chronic lateral ankle instability. Am J Sports Med. 44:2975–83. doi: 10.1177/0363546516656183. DOI: 10.1177/0363546516656183. PMID: 27480980.
Article9. Park JS, Kim BS. 2016; Risk factors for failure after lateral ankle ligament repair. J Korean Foot Ankle Soc. 20:62–6. doi: 10.14193/jkfas.2016.20.2.62. DOI: 10.14193/jkfas.2016.20.2.62.
Article10. Coetzee JC, Ellington JK, Ronan JA, Stone RM. 2018; Functional results of open Broström ankle ligament repair augmented with a suture tape. Foot Ankle Int. 39:304–10. doi: 10.1177/1071100717742363. DOI: 10.1177/1071100717742363. PMID: 29420055.
Article11. Cho BK, Park KJ, Kim SW, Lee HJ, Choi SM. 2015; Minimal invasive suture-tape augmentation for chronic ankle instability. Foot Ankle Int. 36:1330–8. doi: 10.1177/1071100715592217. DOI: 10.1177/1071100715592217. PMID: 26112405.
Article12. Xu DL, Gan KF, Li HJ, Zhou SY, Lou ZQ, Wang Y, et al. 2019; Modified Broström repair with and without augmentation using suture tape for chronic lateral ankle instability. Orthop Surg. 11:671–8. doi: 10.1111/os.12516. DOI: 10.1111/os.12516. PMID: 31456322. PMCID: PMC6712379.
Article13. Porter M, Shadbolt B, Ye X, Stuart R. 2019; Ankle lateral ligament augmentation versus the modified Broström-Gould procedure: a 5-year randomized controlled trial. Am J Sports Med. 47:659–66. doi: 10.1177/0363546518820529. DOI: 10.1177/0363546518820529. PMID: 30699039.
Article14. Cho BK, Kim YM, Shon HC, Park KJ, Cha JK, Ha YW. 2015; A ligament reattachment technique for high-demand athletes with chronic ankle instability. J Foot Ankle Surg. 54:7–12. doi: 10.1053/j.jfas.2014.09.008. DOI: 10.1053/j.jfas.2014.09.008. PMID: 25441285.
Article15. Cho BK, Kim YM, Park KJ, Park JK, Kim DK. 2015; A prospective outcome and cost-effectiveness comparison between two ligament reattachment techniques using suture anchors for chronic ankle instability. Foot Ankle Int. 36:172–9. doi: 10.1177/1071100714552079. DOI: 10.1177/1071100714552079. PMID: 25237170.
Article16. Schuh R, Benca E, Willegger M, Hirtler L, Zandieh S, Holinka J, et al. 2016; Comparison of Broström technique, suture anchor repair, and tape augmentation for reconstruction of the anterior talofibular ligament. Knee Surg Sports Traumatol Arthrosc. 24:1101–7. doi: 10.1007/s00167-015-3631-7. DOI: 10.1007/s00167-015-3631-7. PMID: 25957613.
Article17. Viens NA, Wijdicks CA, Campbell KJ, LaPrade RF, Clanton TO. 2014; Anterior talofibular ligament ruptures, part 1: biomechanical comparison of augmented Broström repair techniques with the intact anterior talofibular ligament. Am J Sports Med. 42:405–11. doi: 10.1177/0363546513510141. DOI: 10.1177/0363546513510141. PMID: 24275864.18. Willegger M, Benca E, Hirtler L, Hradecky K, Holinka J, Windhager R, et al. 2016; Biomechanical stability of tape augmentation for anterior talofibular ligament (ATFL) repair compared to the native ATFL. Knee Surg Sports Traumatol Arthrosc. 24:1015–21. doi: 10.1007/s00167-016-4048-7. DOI: 10.1007/s00167-016-4048-7. PMID: 26878851. PMCID: PMC4823330.
Article19. Cho BK, Hong SH, Jeon JH. 2019; Effect of lateral ligament augmentation using suture-tape on functional ankle instability. Foot Ankle Int. 40:447–56. doi: 10.1177/1071100718818554. DOI: 10.1177/1071100718818554. PMID: 30623668.
Article20. DeVries JG, Scharer BM, Romdenne TA. 2019; Ankle stabilization with arthroscopic versus open with suture tape augmentation techniques. J Foot Ankle Surg. 58:57–61. doi: 10.1053/j.jfas.2018.08.011. DOI: 10.1053/j.jfas.2018.08.011. PMID: 30448373.
Article21. Ramírez-Gómez VJ, Gómez-Carlín LA, Ortega-Orozco R, Zazueta-Arnaud CA, Patiño-Fernández JP. 2020; Clinical and functional results of Broström-Gould procedure with suture tape augmentation: an evaluation using three scales. J Foot Ankle Surg. 59:733–8. doi: 10.1053/j.jfas.2020.01.005. DOI: 10.1053/j.jfas.2020.01.005. PMID: 32245739.
Article22. Cho BK, Park JK, Choi SM, SooHoo NF. 2019; A randomized comparison between lateral ligaments augmentation using suture-tape and modified Broström repair in young female patients with chronic ankle instability. Foot Ankle Surg. 25:137–42. doi: 10.1016/j.fas.2017.09.008. DOI: 10.1016/j.fas.2017.09.008. PMID: 29409289.
Article23. Cho BK, Park KJ, Park JK, SooHoo NF. 2017; Outcomes of the modified Broström procedure augmented with suture-tape for ankle instability in patients with generalized ligamentous laxity. Foot Ankle Int. 38:405–11. doi: 10.1177/1071100716683348. DOI: 10.1177/1071100716683348. PMID: 28367693.
Article24. Beighton P, Horan F. 1969; Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br. 51:444–53. doi: 10.1302/0301-620X.51B3.444. DOI: 10.1302/0301-620X.51B3.444.25. Roos EM, Brandsson S, Karlsson J. 2001; Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int. 22:788–94. doi: 10.1177/107110070102201004. DOI: 10.1177/107110070102201004. PMID: 11642530.
Article26. Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. 2005; Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 26:968–83. doi: 10.1177/107110070502601113. DOI: 10.1177/107110070502601113. PMID: 16309613.27. Liu W, Li H, Hua Y. 2017; Quantitative magnetic resonance imaging (MRI) analysis of anterior talofibular ligament in lateral chronic ankle instability ankles pre- and postoperatively. BMC Musculoskelet Disord. 18:397. doi: 10.1186/s12891-017-1758-z. DOI: 10.1186/s12891-017-1758-z. PMID: 28899377. PMCID: PMC5596477.
Article28. Park HJ, Lee SY, Park NH, Rho MH, Chung EC, Park JH, et al. 2016; Three-dimensional isotropic T2-weighted fast spin-echo (VISTA) ankle MRI versus two-dimensional fast spin-echo T2-weighted sequences for the evaluation of anterior talofibular ligament injury. Clin Radiol. 71:349–55. doi: 10.1016/j.crad.2015.12.007. DOI: 10.1016/j.crad.2015.12.007. PMID: 26774370.
Article29. Waldrop NE 3rd, Wijdicks CA, Jansson KS, LaPrade RF, Clanton TO. 2012; Anatomic suture anchor versus the Broström technique for anterior talofibular ligament repair: a biomechanical comparison. Am J Sports Med. 40:2590–6. doi: 10.1177/0363546512458420. DOI: 10.1177/0363546512458420. PMID: 22962291.30. Park HJ, Cha SD, Kim SS, Rho MH, Kwag HJ, Park NH, et al. 2012; Accuracy of MRI findings in chronic lateral ankle ligament injury: comparison with surgical findings. Clin Radiol. 67:313–8. doi: 10.1016/j.crad.2011.08.025. DOI: 10.1016/j.crad.2011.08.025. PMID: 22078461.
Article31. Kanamoto T, Shiozaki Y, Tanaka Y, Yonetani Y, Horibe S. 2014; The use of MRI in pre-operative evaluation of anterior talofibular ligament in chronic ankle instability. Bone Joint Res. 3:241–5. doi: 10.1302/2046-3758.38.2000295. DOI: 10.1302/2046-3758.38.2000295. PMID: 25085232. PMCID: PMC4127656.
Article32. Biercevicz AM, Miranda DL, Machan JT, Murray MM, Fleming BC. 2013; In situ, noninvasive, T2*-weighted MRI-derived parameters predict ex vivo structural properties of an anterior cruciate ligament reconstruction or bioenhanced primary repair in a porcine model. Am J Sports Med. 41:560–6. doi: 10.1177/0363546512472978. DOI: 10.1177/0363546512472978. PMID: 23348076. PMCID: PMC3593999.
Article33. Dimmick S, Kennedy D, Daunt N. 2008; Evaluation of thickness and appearance of anterior talofibular and calcaneofibular ligaments in normal versus abnormal ankles with MRI. J Med Imaging Radiat Oncol. 52:559–63. doi: 10.1111/j.1440-1673.2008.02018.x. DOI: 10.1111/j.1440-1673.2008.02018.x. PMID: 19178629.
Article34. Boonthathip M, Chen L, Trudell D, Resnick D. 2011; Lateral ankle ligaments: MR arthrography with anatomic correlation in cadavers. Clin Imaging. 35:42–8. doi: 10.1016/j.clinimag.2009.12.022. DOI: 10.1016/j.clinimag.2009.12.022. PMID: 21237417.
Article35. Teramoto A, Akatsuka Y, Takashima H, Shoji H, Sakakibara Y, Watanabe K, et al. 2020; 3D MRI evaluation of morphological characteristics of lateral ankle ligaments in injured patients and uninjured controls. J Orthop Sci. 25:183–7. doi: 10.1016/j.jos.2019.02.018. DOI: 10.1016/j.jos.2019.02.018. PMID: 30885728.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Unrestricted Weight-Bearing in a Stirrup Brace Following the Broström Procedure with Suture Tape for Chronic Lateral Ankle Instability
- Diagnosis of Lateral Ankle Ligament Injury in the Evaluation of Chronic Lateral Ankle Instability
- Surgical Treatment for Simultaneous Medial and Lateral Ankle Instability in a Young Patient Engaged in High Physical Activities: A Case Report
- Are Magnetic Resonance Imaging Findings of Ankle Instability Always Correlated with Operative and Physical Examination Findings?
- Chronic Lateral Ankle Instability