J Korean Med Sci.
2021 Aug;36(34):e243. 10.3346/jkms.2021.36.e243.
Association of the COVID-19 Pandemic and Low-rescue Suicide Attempts in Patients Visiting the Emergency Department after Attempting Suicide
- Affiliations
-
- 1Department of Emergency Medicine, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Emergency Medicine, Daejeon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Counseling Psychology, Graduate School of Theology, Seoul Theological University, Bucheon, Korea
- KMID: 2519598
- DOI: http://doi.org/10.3346/jkms.2021.36.e243
Abstract
- Background
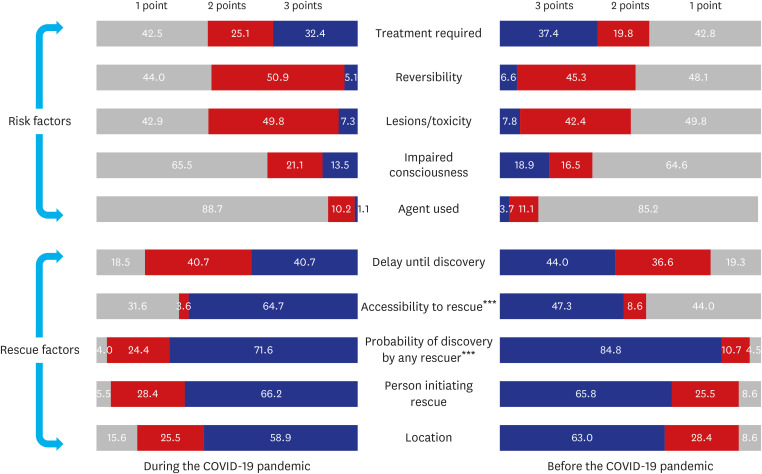
The coronavirus disease 2019 (COVID-19) pandemic may increase the total number of suicide attempts and the proportion of low-rescue attempts. We investigated the factors affecting low-rescue suicide attempts using the risk-rescue rating scale (RRRS) among patients who visited the emergency department (ED) after attempting suicide before or during the COVID-19 pandemic.
Methods
We retrospectively investigated suicide attempts made by patients who visited our ED from March 2019 to September 2020. Patients were classified into two groups based on whether they attempted suicide before or during the COVID-19 pandemic. Data on demographic variables, psychiatric factors, suicide risk factors and rescue factors were collected and compared.
Results
A total of 518 patients were included in the study, 275 (53.1%) of whom attempted suicide during the COVID-19 pandemic. The proportion of patients who made low-rescue suicide attempts differed before and during the COVID-19 pandemic (37.1% vs. 28.8%) (P = 0.046). However, the proportions of patients who made high-risk suicide attempts and high-lethality suicide attempts did not significantly differ between the two periods. The independent risk factors for low-rescue suicide attempts were age and the COVID-19 pandemic (odds ratio [OR], 1.02; 95% confidence interval [CI], 1.00–1.03; P = 0.006) (OR, 1.52; 95% CI, 1.03–2.25; P = 0.034).
Conclusion
The COVID-19 pandemic was associated with low-rescue suicide attempts in patients visiting the ED after attempting suicide. Thus, we need to consider the implementation of measures to prevent low-rescue suicide attempts during similar infectious disease crises.
Keyword
Figure
Reference
-
1. Spiteri G, Fielding J, Diercke M, Campese C, Enouf V, Gaymard A, et al. First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020. Euro Surveill. 2020; 25(9):2000178.
Article2. Bachmann S. Epidemiology of suicide and the psychiatric perspective. Int J Environ Res Public Health. 2018; 15(7):1425.
Article3. Woo S, Lee SW, Lee K, Seo WS, Lee J, Kim HC, et al. Characteristics of high-intent suicide attempters admitted to emergency departments. J Korean Med Sci. 2018; 33(41):e259. PMID: 30288157.
Article4. Statistics Korea. Updated 2019. Accessed July 1, 2021. http://kostat.go.kr/assist/synap/preview/skin/doc.html?fn=synapview385219_2&rs=/assist/synap/preview.5. OECD. Health at a glance 2019. Updated 2019. Accessed July 2, 2021. http://www.oecd.org/health/.6. Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020; 3(7):e2014053. PMID: 32609353.
Article7. Zortea TC, Brenna CT, Joyce M, McClelland H, Tippett M, Tran MM, et al. The impact of infectious disease-related public health emergencies on suicide, suicidal behavior, and suicidal thoughts. Crisis. 2020; 16:1–14.8. Sakamoto H, Ishikane M, Ghaznavi C, Ueda P. Assessment of suicide in Japan during the COVID-19 pandemic vs previous years. JAMA Netw Open. 2021; 4(2):e2037378. PMID: 33528554.
Article9. Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020; 113(10):707–712. PMID: 32539153.
Article10. Ammerman BA, Burke TA, Jacobucci R, McClure K. Preliminary investigation of the association between COVID-19 and suicidal thoughts and behaviors in the U.S. J Psychiatr Res. 2021; 134:32–38. PMID: 33360222.
Article11. Weisman AD, Worden JW. Risk-rescue rating in suicide assessment. Arch Gen Psychiatry. 1972; 26(6):553–560. PMID: 5027119.
Article12. Oh SH, Kim HJ, Kim SH, Kim YM, Park KN. Which deliberate self-poisoning patients are most likely to make high-lethality suicide attempts? Int J Ment Health Syst. 2015; 9:35. PMID: 26347801.
Article13. Kim DW, Jeong KY, Kim KS. Psychological scales as predictors of emergency department hospitalizations in suicide attempters. Am J Emerg Med. 2018; 36(1):93–99. PMID: 28743477.
Article14. Misson H, Mathieu F, Jollant F, Yon L, Guillaume S, Parmentier C, et al. Factor analyses of the Suicidal Intent Scale (SIS) and the Risk-Rescue Rating Scale (RRRS): toward the identification of homogeneous subgroups of suicidal behaviors. J Affect Disord. 2010; 121(1-2):80–87. PMID: 19524302.
Article15. Kim DW, Cho SE, Kang JM, Woo SK, Kang SG, Yeon BK, et al. Risk factors for serious suicide attempts: difference between older and younger attempters in the emergency department. Front Psychiatry. 2021; 11:607811. PMID: 33488429.
Article16. Wasserman IM. The impact of epidemic, war, prohibition and media on suicide: United States, 1910–1920. Suicide Life Threat Behav. 1992; 22(2):240–254. PMID: 1626335.17. Yip PS, Cheung YT, Chau PH, Law YW. The impact of epidemic outbreak: the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis. 2010; 31(2):86–92. PMID: 20418214.18. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020; 33(2):e100213. PMID: 32215365.
Article19. Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. Int J Environ Res Public Health. 2020; 17(6):2032.
Article20. Statistics Korea. Updated 2020. Accessed July 3, 2021. http://kostat.go.kr/assist/synap/preview/skin/doc.html?fn=synapview386517_2&rs=/assist/synap/preview.21. Conwell Y, Duberstein PR, Cox C, Herrmann J, Forbes N, Caine ED. Age differences in behaviors leading to completed suicide. Am J Geriatr Psychiatry. 1998; 6(2):122–126. PMID: 9581207.
Article22. Conwell Y, Lyness JM, Duberstein P, Cox C, Seidlitz L, DiGiorgio A, et al. Completed suicide among older patients in primary care practices: a controlled study. J Am Geriatr Soc. 2000; 48(1):23–29. PMID: 10642017.
Article23. Kim H, Ahn JS, Kim H, Cha YS, Lee J, Kim MH, et al. Sociodemographic and clinical characteristics of old-old suicide attempters compared with young-old and middle-aged attempters. Int J Geriatr Psychiatry. 2018; 33(12):1717–1726. PMID: 30264415.
Article24. Wand AP, Zhong BL, Chiu HF, Draper B, De Leo D. COVID-19: the implications for suicide in older adults. Int Psychogeriatr. 2020; 32(10):1225–1230. PMID: 32349837.
Article25. Druss BG. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. 2020; 77(9):891–892. PMID: 32242888.
Article26. Carlin GL, Baumgartner JS, Moftakhar T, König D, Negrin LL. Impact of COVID-19 lockdown on suicide attempts: a retrospective analysis of the springtime admissions to the trauma resuscitation room at the Medical University of Vienna from 2015–2020. Wien Klin Wochenschr. 2021; 1–8.27. Song Y, Rhee SJ, Lee H, Kim MJ, Shin D, Ahn YM. Comparison of suicide risk by mental illness: a retrospective review of 14-year electronic medical records. J Korean Med Sci. 2020; 35(47):e402. PMID: 33289369.
Article28. Santini ZI, Jose PE, York Cornwell E, Koyanagi A, Nielsen L, Hinrichsen C, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 2020; 5(1):e62–e70. PMID: 31910981.
Article29. Chang SS, Stuckler D, Yip P, Gunnell D. Impact of 2008 global economic crisis on suicide: time trend study in 54 countries. BMJ. 2013; 347:f5239. PMID: 24046155.
Article30. Milner A, Page A, LaMontagne AD. Long-term unemployment and suicide: a systematic review and meta-analysis. PLoS One. 2013; 8(1):e51333. PMID: 23341881.
Article31. Nordt C, Warnke I, Seifritz E, Kawohl W. Modelling suicide and unemployment: a longitudinal analysis covering 63 countries, 2000–11. Lancet Psychiatry. 2015; 2(3):239–245. PMID: 26359902.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Monthly Characteristics of Adolescent Suicide Attempts Before, During and After COVID-19
- Comparison of Suicide Attempt by Generation During the COVID-19 Pandemic: Focusing on the Younger Generation
- Assessment of geriatric suicidal attempts in Korea during the COVID-19 pandemic: comparison with previous years
- Factors affecting patients who attempted suicide in the emergency department due to the prolonged pandemic of COVID-19
- Suicide attempts presenting to the emergency department before and during the COVID-19 pandemic: a comparative study