Ann Hepatobiliary Pancreat Surg.
2021 Aug;25(3):376-385. 10.14701/ahbps.2021.25.3.376.
“Mesopancreas-first” radical resection of pancreatic head cancer following the Cattell–Braasch–Valdoni maneuver: Appreciating the legacy of pioneers in visceral surgery
- Affiliations
-
- 1Department of Surgery, Papageorgiou Hospital, Thessaloniki, Greece
- KMID: 2519295
- DOI: http://doi.org/10.14701/ahbps.2021.25.3.376
Abstract
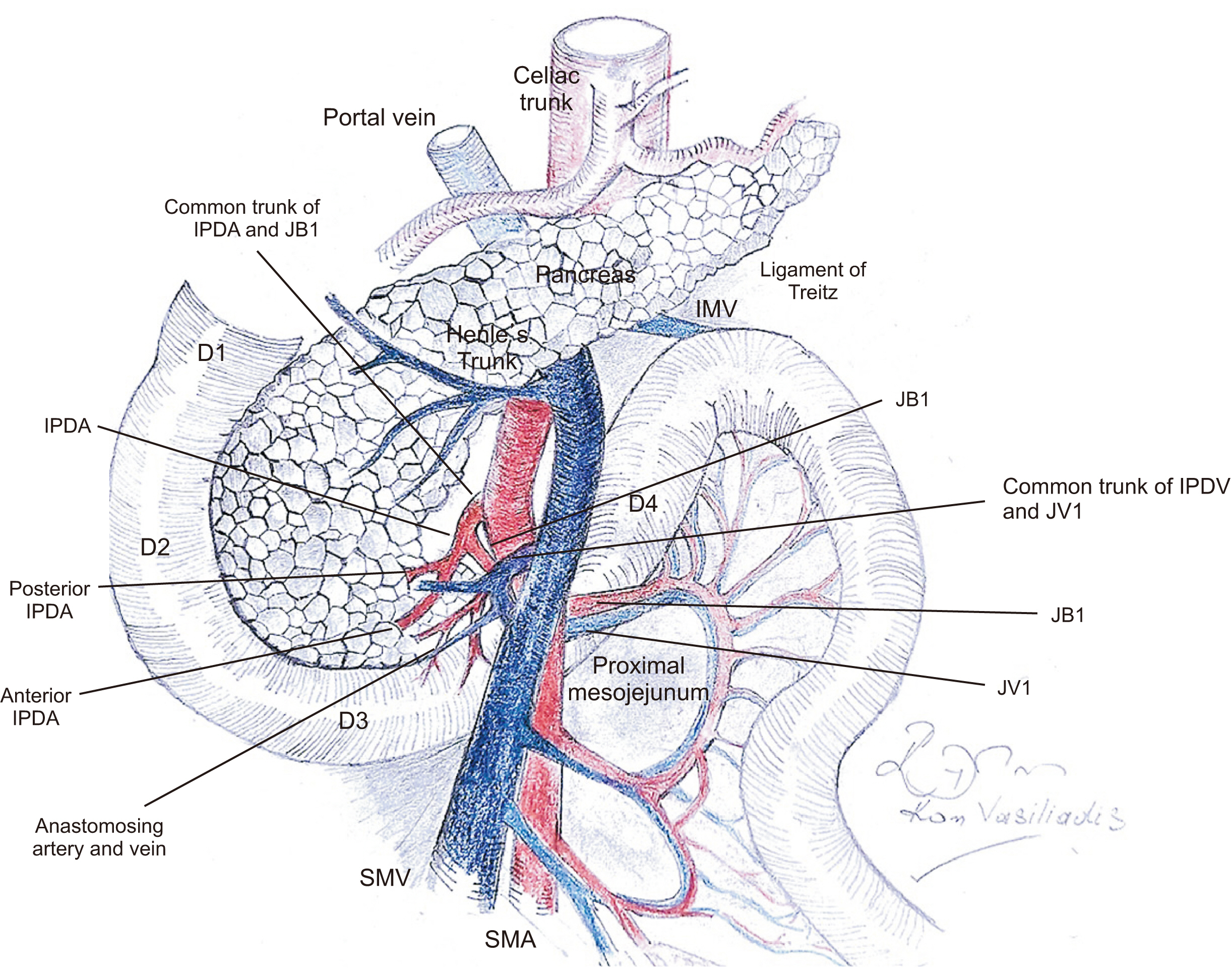
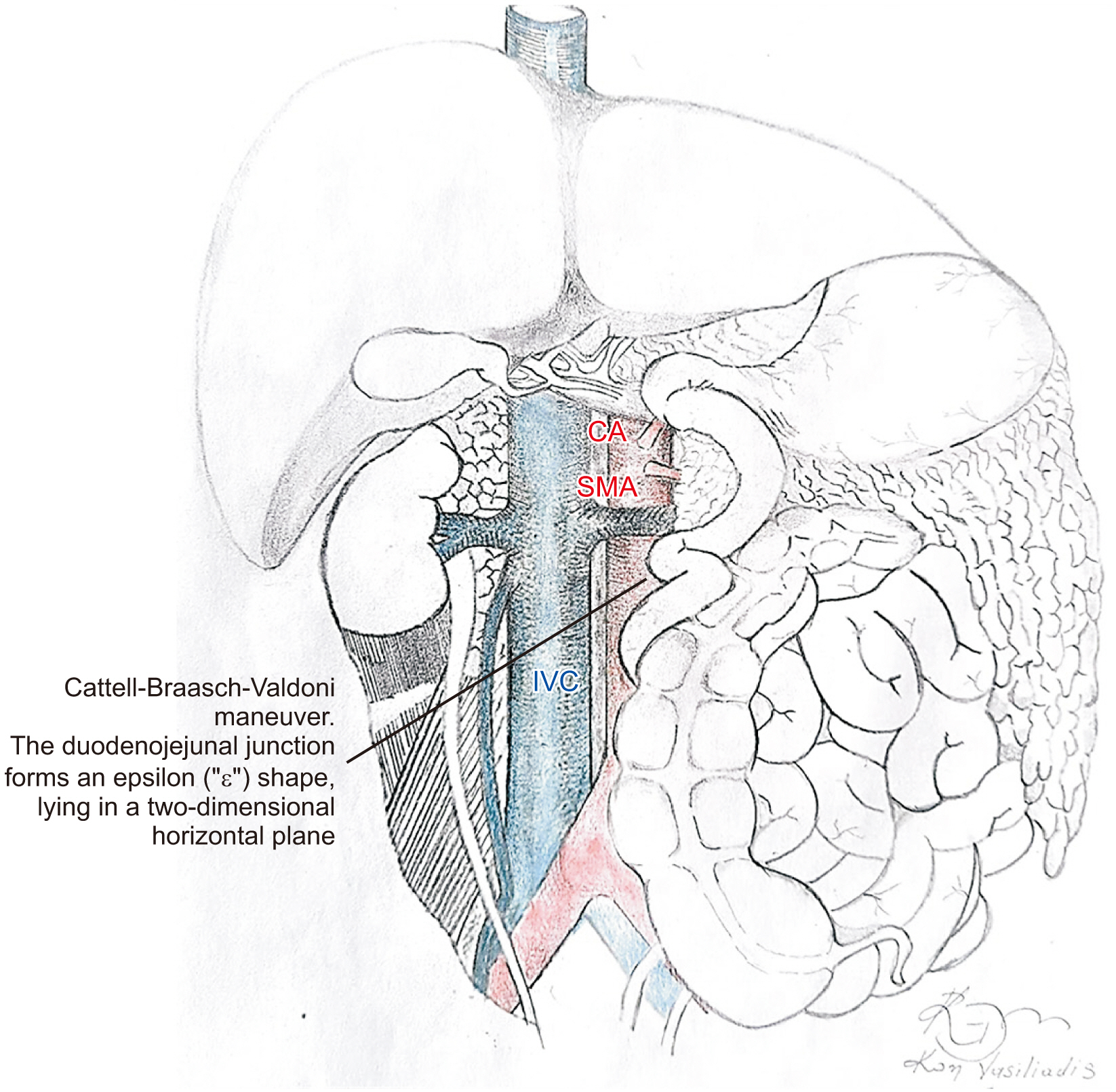
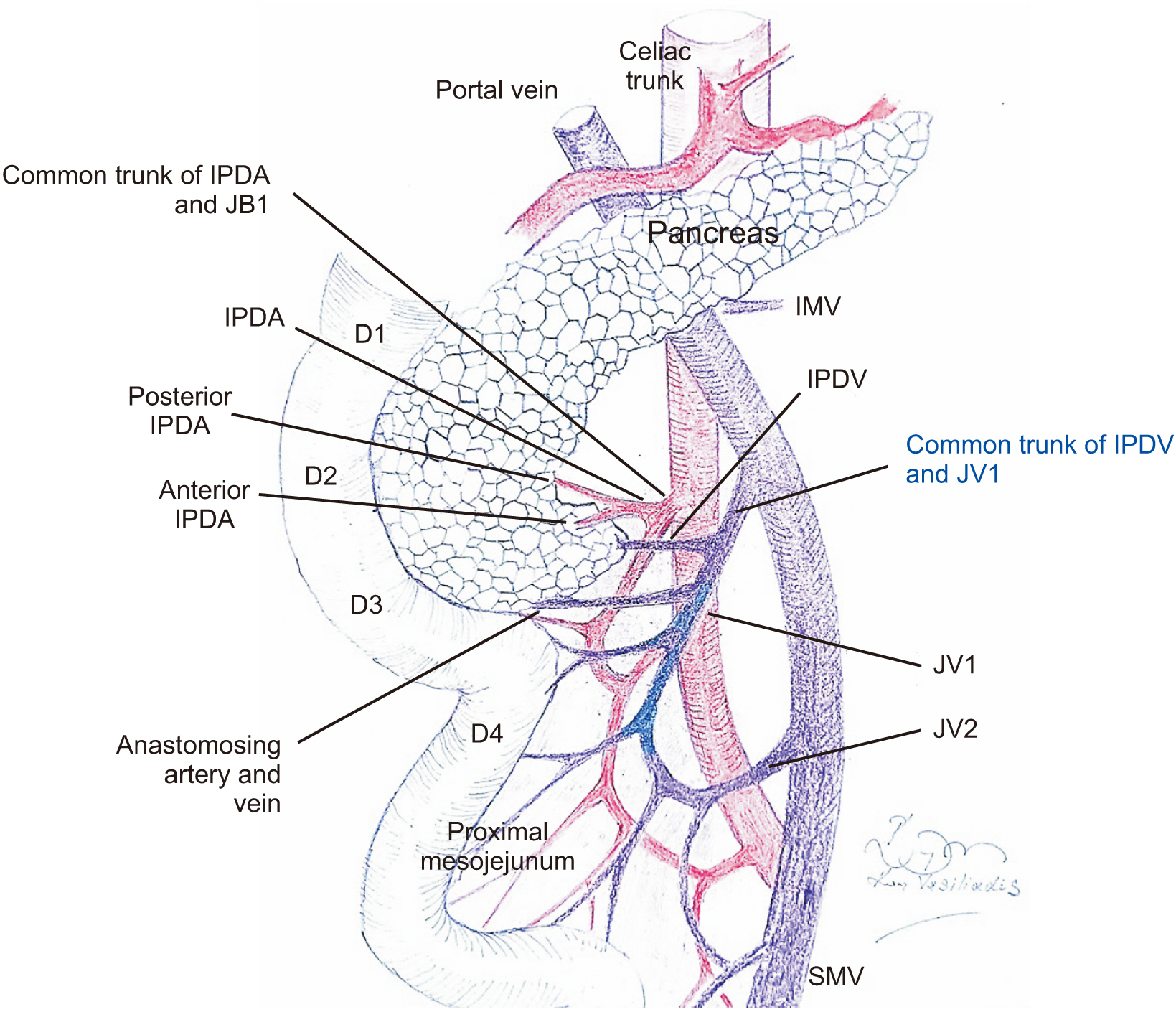
- The “artery-first” approach pancreaticoduodenectomy, with maximal mesopancreas excision and central vascular ligation, represents the current principal determinants of radicality in pancreatic head cancer resection. However, these modifications at the resection stage of pancreaticoduodenectomy constitute extremely demanding and technically complicated procedures. Among the most critical contributing factors in the difficulty of artery-first approaches is the spiral configuration of the mesoduodenum and proximal mesojejunum around the superior mesenteric artery axis. This creates complicated tridimensional anatomy, making surgical dissection in the inferior peripancreatic anatomic area extremely challenging and demanding. The Cattell–Braasch–Valdoni maneuver (right-sided medial visceral mobilization and intestinal derotation maneuver) restores the embryological twist of the duodenojejunal junction, which demystifies the distorted peripancreatic vascular anatomy and facilitates a safe and radical “mesopancreas-first” pancreatic head cancer resection. The aim of this paper was to present the advantages, efficacy, and safety of the Cattell–Braasch–Valdoni maneuver in artery-first approach radical pancreaticoduodenectomy and provide a detailed description of its surgical technique.
Keyword
Figure
Reference
-
1. Kimura W. 2000; Surgical anatomy of the pancreas for limited resection. J Hepatobiliary Pancreat Surg. 7:473–479. DOI: 10.1007/s005340070017. PMID: 11180873.
Article2. Gaedcke J, Gunawan B, Grade M, Szöke R, Liersch T, Becker H, et al. 2010; The mesopancreas is the primary site for R1 resection in pancreatic head cancer: relevance for clinical trials. Langenbecks Arch Surg. 395:451–458. DOI: 10.1007/s00423-009-0494-8. PMID: 19418067. PMCID: PMC2848727.
Article3. Esposito I, Kleeff J, Bergmann F, Reiser C, Herpel E, Friess H, et al. 2008; Most pancreatic cancer resections are R1 resections. Ann Surg Oncol. 15:1651–1660. DOI: 10.1245/s10434-008-9839-8. PMID: 18351300.
Article4. Adham M, Singhirunnusorn J. 2012; Surgical technique and results of total mesopancreas excision (TMpE) in pancreatic tumors. Eur J Surg Oncol. 38:340–345. DOI: 10.1016/j.ejso.2011.12.015. PMID: 22264964.
Article5. Peparini N, Chirletti P. 2012; Clearance of the retropancreatic margin in pancreatic carcinomas: total mesopancreas excision or extended lymphadenectomy? Eur J Surg Oncol. 38:1146. author reply 1147. DOI: 10.1016/j.ejso.2012.07.004. PMID: 22819328.
Article6. Inoue Y, Saiura A, Yoshioka R, Ono Y, Takahashi M, Arita J, et al. 2015; Pancreatoduodenectomy with systematic mesopancreas dissection using a supracolic anterior artery-first approach. Ann Surg. 262:1092–1101. DOI: 10.1097/SLA.0000000000001065. PMID: 25587814.
Article7. Neoptolemos JP, Palmer DH, Ghaneh P, Psarelli EE, Valle JW, Halloran CM, et al. 2017; Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet. 389:1011–1024. DOI: 10.1016/S0140-6736(16)32409-6. PMID: 28129987.
Article8. Sharma D, Isaji S. 2016; Mesopancreas is a misnomer: time to correct the nomenclature. J Hepatobiliary Pancreat Sci. 23:745–749. DOI: 10.1002/jhbp.402. PMID: 27734589.
Article9. Peparini N. 2015; Mesopancreas: a boundless structure, namely the rationale for dissection of the paraaortic area in pancreaticoduodenectomy for pancreatic head carcinoma. World J Gastroenterol. 21:2865–2870. DOI: 10.3748/wjg.v21.i10.2865. PMID: 25780282. PMCID: PMC4356904.
Article10. Hartwig W, Vollmer CM, Fingerhut A, Yeo CJ, Neoptolemos JP, Adham M, et al. International Study Group on Pancreatic Surgery. 2014; Extended pancreatectomy in pancreatic ductal adenocarcinoma: definition and consensus of the International Study Group for Pancreatic Surgery (ISGPS). Surgery. 156:1–14. DOI: 10.1016/j.surg.2014.02.009. PMID: 24856668.
Article11. Borghi F, Gattolin A, Garbossa D, Bogliatto F, Garavoglia M, Levi AC. 1998; Embryologic bases of extended radical resection in pancreatic cancer. Arch Surg. 133:297–301. DOI: 10.1001/archsurg.133.3.297. PMID: 9517744.
Article12. Hagai H. 2003; Configurational anatomy of the pancreas: its surgical relevance from ontogenetic and comparative-anatomical viewpoints. J Hepatobiliary Pancreat Surg. 10:48–56. DOI: 10.1007/s10534-002-0796-6. PMID: 12918457.
Article13. Isaji S, Murata Y, Kishiwada M. Neoptolemos J, Urrutia R, Abbruzzese J, Büchler M, editors. 2018. New Japanese classification of pancreatic cancer. Pancreatic cancer. Springer;New York: p. 1021–1037. DOI: 10.1007/978-1-4939-7193-0_84.
Article14. Schneider M, Strobel O, Hackert T, Büchler MW. 2019; Pancreatic resection for cancer-the Heidelberg technique. Langenbecks Arch Surg. 404:1017–1022. DOI: 10.1007/s00423-019-01839-1. PMID: 31728630.
Article15. Japan Pancreas Society. 2003. Classification of pancreatic carcinoma. 2nd English edition. Kanehara;Tokyo:16. Peparini N. 2016; Para-aortic dissection in pancreaticoduodenectomy with mesopancreas excision for pancreatic head carcinoma: not only an N-staging matter. J Gastrointest Surg. 20:1080–1081. DOI: 10.1007/s11605-016-3131-1. PMID: 27000126.
Article17. Ohigashi H, Ishikawa O, Eguchi H, Yamada T, Sasaki Y, Noura S, et al. 2004; Early ligation of the inferior pancreaticoduodenal artery to reduce blood loss during pancreaticoduodenectomy. Hepatogastroenterology. 51:4–5. PMID: 15011818.18. Weitz J, Rahbari N, Koch M, Büchler MW. 2010; The "artery first" approach for resection of pancreatic head cancer. J Am Coll Surg. 210:e1–e4. DOI: 10.1016/j.jamcollsurg.2009.10.019. PMID: 20113929.
Article19. Hackert T, Werner J, Weitz J, Schmidt J, Büchler MW. 2010; Uncinate process first--a novel approach for pancreatic head resection. Langenbecks Arch Surg. 395:1161–1164. DOI: 10.1007/s00423-010-0663-9. PMID: 20582600.
Article20. Pessaux P, Varma D, Arnaud JP. 2006; Pancreaticoduodenectomy: superior mesenteric artery first approach. J Gastrointest Surg. 10:607–611. DOI: 10.1016/j.gassur.2005.05.001. PMID: 16627229.
Article21. Varty PP, Yamamoto H, Farges O, Belghiti J, Sauvanet A. 2005; Early retropancreatic dissection during pancreaticoduodenectomy. Am J Surg. 189:488–491. DOI: 10.1016/j.amjsurg.2005.01.007. PMID: 15820467.
Article22. Horiguchi A, Ishihara S, Ito M, Nagata H, Shimizu T, Furusawa K, et al. 2007; Pancreatoduodenectomy in which dissection of the efferent arteries of the head of the pancreas is performed first. J Hepatobiliary Pancreat Surg. 14:575–578. DOI: 10.1007/s00534-006-1198-x. PMID: 18040623.
Article23. Xu J, Tian X, Chen Y, Ma Y, Liu C, Tian L, et al. 2017; Total mesopancreas excision for the treatment of pancreatic head cancer. J Cancer. 8:3575–3584. DOI: 10.7150/jca.21341. PMID: 29151943. PMCID: PMC5687173.
Article24. Cattell RB, Braasch JW. 1960; A technique for the exposure of the third and fourth portions of the duodenum. Surg Gynecol Obstet. 111:378–379. PMID: 13808480.25. Sugiyama M, Suzuki Y, Nakazato T, Yokoyama M, Kogure M, Abe N, et al. 2016; Intestinal derotation procedure for facilitating pancreatoduodenectomy. Surgery. 159:1325–1332. DOI: 10.1016/j.surg.2015.11.014. PMID: 26767309.
Article26. Akita M, Yamasaki N, Miyake T, Mimura K, Maeda E, Nishimura T, et al. 2020; Cattell-Braasch maneuver facilitates the artery-first approach and complete excision of the mesopancreas for pancreatoduodenectomy. J Surg Oncol. 121:1126–1131. DOI: 10.1002/jso.25892. PMID: 32141084.
Article27. Papavasiliou P, Arrangoiz R, Zhu F, Chun YS, Edwards K, Hoffman JP. 2012; The anatomic course of the first jejunal branch of the superior mesenteric vein in relation to the superior mesenteric artery. Int J Surg Oncol. 2012:538769. DOI: 10.1155/2012/538769. PMID: 22489264. PMCID: PMC3303700.
Article28. Ishikawa Y, Ban D, Matsumura S, Mitsunori Y, Ochiai T, Kudo A, et al. 2017; Surgical pitfalls of jejunal vein anatomy in pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 24:394–400. DOI: 10.1002/jhbp.451. PMID: 28342263.
Article29. Sakaguchi T, Suzuki S, Morita Y, Oishi K, Suzuki A, Fukumoto K, et al. 2010; Analysis of anatomic variants of mesenteric veins by 3-dimensional portography using multidetector-row computed tomography. Am J Surg. 200:15–22. DOI: 10.1016/j.amjsurg.2009.05.017. PMID: 20074695.
Article30. Horiguchi A, Ishihara S, Ito M, Nagata H, Asano Y, Yamamoto T, et al. 2008; Multislice CT study of pancreatic head arterial dominance. J Hepatobiliary Pancreat Surg. 15:322–326. DOI: 10.1007/s00534-007-1261-2. PMID: 18535772.
Article31. Horiguchi A, Ishihara S, Ito M, Asano Y, Yamamoto T, Miyakawa S. 2010; Three-dimensional models of arteries constructed using multidetector-row CT images to perform pancreatoduodenectomy safely following dissection of the inferior pancreaticoduodenal artery. J Hepatobiliary Pancreat Sci. 17:523–526. DOI: 10.1007/s00534-009-0261-9. PMID: 20714842.
Article32. Negoi I, Beuran M, Hostiuc S, Negoi RI, Inoue Y. 2018; Surgical anatomy of the superior mesenteric vessels related to pancreaticoduodenectomy: a systematic review and meta-analysis. J Gastrointest Surg. 22:802–817. DOI: 10.1007/s11605-018-3669-1. PMID: 29363018.
Article33. Kobayashi Y, Sakamoto Y, Arita J, Akamatsu N, Kaneko J, Hasegawa K, et al. 2018; Vascular anatomy of the jejunal mesentery and complications associated with division of the first jejunal venous trunk during pancreaticoduodenectomy. J Surg Oncol. 117:1297–1304. DOI: 10.1002/jso.24948. PMID: 29205361.
Article34. Hongo N, Mori H, Matsumoto S, Okino Y, Ueda S, Shuto R. 2010; Anatomical variations of peripancreatic veins and their intrapancreatic tributaries: multidetector-row CT scanning. Abdom Imaging. 35:143–153. DOI: 10.1007/s00261-007-9195-3. PMID: 17594120.
Article35. Yamada Y, Mori H, Kiyosue H, Matsumoto S, Hori Y, Maeda T. 2000; CT assessment of the inferior peripancreatic veins: clinical significance. AJR Am J Roentgenol. 174:677–684. DOI: 10.2214/ajr.174.3.1740677. PMID: 10701608.36. Kim HJ, Ko YT, Lim JW, Lee DH. 2007; Radiologic anatomy of the superior mesenteric vein and branching patterns of the first jejunal trunk: evaluation using multi-detector row CT venography. Surg Radiol Anat. 29:67–75. DOI: 10.1007/s00276-006-0153-5. PMID: 17033735.
Article37. Valdoni P. 1974. Chirurgia addominale: tecniche operatorie. Casa Editrice Francesco Vallardi;Milano:38. Tocchi A, Mazzoni G, Puma F, Miccini M, Cassini D, Bettelli E, et al. 2003; Adenocarcinoma of the third and fourth portions of the duodenum: results of surgical treatment. Arch Surg. 138:80–85. DOI: 10.1001/archsurg.138.1.80. PMID: 12511157.39. Bechi P, Maltinti G. 2014; A novel "salvage" indication to intestinal derotation procedure: reconstruction after duodenopancreatectomy. Am J Case Rep. 15:322–325. DOI: 10.12659/AJCR.889793. PMID: 25072806. PMCID: PMC4116345.
Article40. Del Chiaro M, Segersvärd R, Rangelova E, Coppola A, Scandavini CM, Ansorge C, et al. 2015; Cattell-Braasch maneuver combined with artery-first approach for superior mesenteric-portal vein resection during pancreatectomy. J Gastrointest Surg. 19:2264–2268. DOI: 10.1007/s11605-015-2958-1. PMID: 26423804.
Article41. Virgilio E, Amodio PM, Scorsi A, Goglia A, Macarone Palmieri R. 2016; Advantages of the maneuver of intestinal derotation for pancreaticoduodenectomy. J Invest Surg. 29:359–365. DOI: 10.3109/08941939.2016.1160166. PMID: 27096254.
Article42. Nakamura M, Nakashima H, Tsutsumi K, Matsumoto H, Muta Y, Ueno D, et al. 2013; First jejunal vein oriented mesenteric excision for pancreatoduodenectomy. J Gastroenterol. 48:989–995. DOI: 10.1007/s00535-012-0697-6. PMID: 23076543.
Article43. Katz MH, Fleming JB, Pisters PW, Lee JE, Evans DB. 2008; Anatomy of the superior mesenteric vein with special reference to the surgical management of first-order branch involvement at pancreaticoduodenectomy. Ann Surg. 248:1098–1102. DOI: 10.1097/SLA.0b013e31818730f0. PMID: 19092356.
Article44. Sugiyama M, Suzuki Y, Nakazato T, Yokoyama M, Kogure M, Matsuki R, et al. 2020; Vascular anatomy of mesopancreas in pancreatoduodenectomy using an intestinal derotation procedure. World J Surg. 44:3441–3448. DOI: 10.1007/s00268-020-05605-z. PMID: 32474625.
Article45. Dandekar U, Dandekar K, Chavan S. 2015; Right hepatic artery: a cadaver investigation and its clinical significance. Anat Res Int. 2015:412595. DOI: 10.1155/2015/412595. PMID: 26788371. PMCID: PMC4695647.
Article46. Jah A, Jamieson N, Huguet E, Praseedom R. 2009; The implications of the presence of an aberrant right hepatic artery in patients undergoing a pancreaticoduodenectomy. Surg Today. 39:669–674. DOI: 10.1007/s00595-009-3947-3. PMID: 19639433.
Article47. Takasaki K, Yamamoto M, Tsugita M, Ootsubo T, Imaizumi T, Yoshikawa T. 1997; N Nine-year patency of a vascular prosthesis used for portal vein reconstruction during pancreatoduodenectomy. J Hepatobiliary Pancreat Surg. 4:127–130. DOI: 10.1007/BF01211354.48. Herscu G, Wilson SE. 2009; Prosthetic infection: lessons from treatment of the infected vascular graft. Surg Clin North Am. 89:391–401. viiiDOI: 10.1016/j.suc.2008.09.007. PMID: 19281890.
Article49. Fujisaki S, Tomita R, Fukuzawa M. 2001; Utility of mobilization of the right colon and the root of the mesentery for avoiding vein grafting during reconstruction of the portal vein. J Am Coll Surg. 193:576–578. DOI: 10.1016/S1072-7515(01)01039-0. PMID: 11708518.50. Muttillo EM, Felli E, Pessaux P. 2020; Cattell-Braasch maneuver in pancreatic surgery. No need of venous graft for vascular resection. J Surg Oncol. 122:1612–1615. DOI: 10.1002/jso.26180. PMID: 32820545.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic total pancreatectomy with total mesopancreas dissection using counterclockwise technique and tail-first approach
- Bile duct preserving pancreatic head resection (BDPPHR): Can we conclusively define the extent of head resection in surgery for chronic pancreatitis?
- Adjuvant Therapy of Pancreatic Cancer
- Laparoscopic repeated pancreatectomy for isolated local recurrence in remnant pancreas following laparoscopic radical pancreatectomy for pancreatic ductal adenocarcinoma: Two cases report
- Duodenum-preserving Pancreatic Head Resection for Benign Pancreatic Head Lesion