J Korean Med Sci.
2021 Aug;36(32):e235. 10.3346/jkms.2021.36.e235.
Characteristics and Prognosis of Hospitalized Patients at High Risk of Deterioration Identified by the Rapid Response System: a Multicenter Cohort Study
- Affiliations
-
- 1Division of Pulmonology and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Hallym University Chuncheon Sacred Heart Hospital, Chuncheon, Korea
- KMID: 2519229
- DOI: http://doi.org/10.3346/jkms.2021.36.e235
Abstract
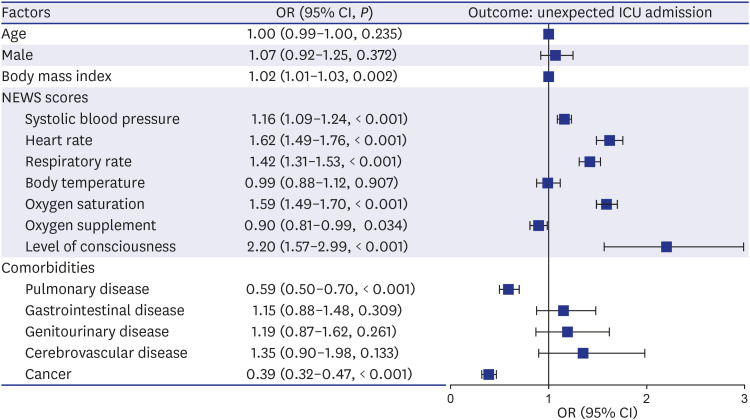
- We aimed to investigate the characteristics and prognosis of high risk hospitalized patients identified by the rapid response system (RRS). A multicentered retrospective cohort study was conducted from June 2019 to December 2020. The National Early Warning Score (NEWS) was used for RRS activation. The outcome was unexpected intensive care unit (ICU) admission within 24 hours after RRS activation. The 11,459 patients with RRS activations were included. We found distinct clinical characteristics in patients who underwent ICU admission. All NEWS parameters were associated with the risk of unexpected ICU admission except body temperature. Body mass index, pulmonary disease, and cancer are related to the decreased risk of unexpected ICU admission. In conclusion, there were differences in clinical characteristics among high risk patients, and those differences were associated with unexpected ICU admissions. Clinicians should consider factors relating to unexpected ICU admission in the management of high risk patients identified by RRS.
Figure
Reference
-
1. Lyons PG, Klaus J, McEvoy CA, Westervelt P, Gage BF, Kollef MH. Factors associated with clinical deterioration among patients hospitalized on the wards at a tertiary cancer hospital. J Oncol Pract. 2019; 15(8):e652–e665. PMID: 31306039.
Article2. Jones DA, DeVita MA, Bellomo R. Rapid-response teams. N Engl J Med. 2011; 365(2):139–146. PMID: 21751906.
Article3. Litvak E, Pronovost PJ. Rethinking rapid response teams. JAMA. 2010; 304(12):1375–1376. PMID: 20858881.
Article4. Lee YJ, Park JJ, Yoon YE, Kim JW, Park JS, Kim T, et al. Successful implementation of a rapid response system in the department of internal medicine. Korean J Crit Care Med. 2014; 29(2):77–82.
Article5. Kim Y, Lee DS, Min H, Choi YY, Lee EY, Song I, et al. Effectiveness analysis of a part-time rapid response system during operation versus nonoperation. Crit Care Med. 2017; 45(6):e592–e599. PMID: 28346260.
Article6. Salvatierra G, Bindler RC, Corbett C, Roll J, Daratha KB. Rapid response team implementation and in-hospital mortality. Crit Care Med. 2014; 42(9):2001–2006. PMID: 24743041.
Article7. Yang E, Lee H, Lee SM, Kim S, Ryu HG, Lee HJ, et al. Effectiveness of a daytime rapid response system in hospitalized surgical ward patients. Acute Crit Care. 2020; 35(2):77–86. PMID: 32506872.
Article8. Lee BY, Hong SB. Rapid response systems in Korea. Acute Crit Care. 2019; 34(2):108–116. PMID: 31723915.
Article9. World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization;1992.10. Kim SH, Choi H, Lee H, Hong JY, Kim Y. Predicting unexpected deterioration of high-risk hospitalized patients during the COVID-19 pandemic: a multicenter cohort study. Resuscitation. 2021; 163:14–15. PMID: 33848582.
Article11. Jensen MT, Marott JL, Lange P, Vestbo J, Schnohr P, Nielsen OW, et al. Resting heart rate is a predictor of mortality in COPD. Eur Respir J. 2013; 42(2):341–349. PMID: 23143550.
Article12. de Miguel Sánchez C, Elustondo SG, Estirado A, Sánchez FV, de la Rasilla Cooper CG, Romero AL, et al. Palliative performance status, heart rate and respiratory rate as predictive factors of survival time in terminally ill cancer patients. J Pain Symptom Manage. 2006; 31(6):485–492. PMID: 16793488.
Article13. Kim JK, Jang SH, Park S, Kim JH, Park JY, Yoo KH, et al. Current situation of home oxygen therapy for chronic obstructive pulmonary disease patients in Korea. J Korean Med Sci. 2020; 35(4):e12. PMID: 31997611.
Article14. Kim HJ, Kim HJ, Yun J, Kim KH, Kim SH, Lee SC, et al. Pathophysiological role of hormones and cytokines in cancer cachexia. J Korean Med Sci. 2012; 27(2):128–134. PMID: 22323858.
Article15. Lee J, Ban WH, Kim SW, Kim EY, Han MR, Kim SC. Utilization of a rapid response team and associated outcomes in patients with malignancy. Acute Crit Care. 2020; 35(1):16–23. PMID: 32131577.
Article16. Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315(8):762–774. PMID: 26903335.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Causes of Neurologic Deterioration before Management in the Patients with a Ruptured Aneurysm
- Development and validation of a novel scoring system to predict the risk of uterine perforation during intracavitary brachytherapy for cervical cancer
- Rapid response systems in Korea
- Risk Factors of FEV 1 /FVC Decline in COPD Patients
- Effects of a Rapid Response Team on the Clinical Outcomes of Cardiopulmonary Resuscitation of Patients Hospitalized in General Wards