Anesth Pain Med.
2021 Jul;16(3):299-304. 10.17085/apm.21010.
Diagnosis and treatment of nerve injury following venipuncture - A report of two cases -
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chung-Ang University Hospital, Seoul, Korea
- 2Department of Anesthesiology and Pain Medicine, Chung-Ang University College of Medicine, Seoul, Korea
- 3Department of Radiology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea
- 4Department of Anesthesiology and Pain Medicine, Samsung Medical Center, School of Medicine, Sungkyunkwan University, Seoul, Korea
- KMID: 2519061
- DOI: http://doi.org/10.17085/apm.21010
Abstract
- Background
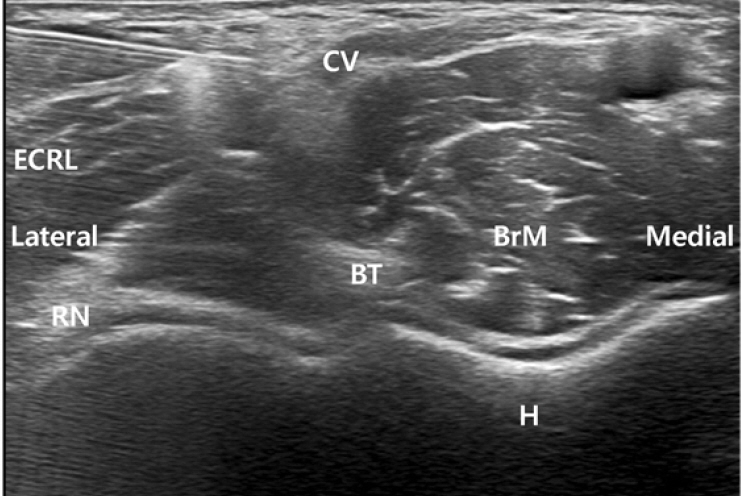
Venipuncture is one of the one of the most commonly performed, minimally-invasive procedures; however, it may lead to peripheral nerve injury. Here, we describe the diagnosis, treatment, and prognosis of two self-reported cases of nerve injury during venipuncture with the aim of drawing attention to possible needle-related nerve injuries. Case: Two anesthesiologists in our hospital experienced an injury of the lateral antebrachial cutaneous branch of the musculocutaneous nerve during venipuncture. Immediately, they underwent ultrasound examinations and nerve blocks with oral medication, resulting in full recovery.
Conclusions
Ultrasonography is important for the early and confirmative diagnosis of a nerve injury during venipuncture, and for immediate treatment with a nerve block. Moreover, it is imperative for both the practitioner and the patient to be aware of the possible complication of nerve injury after venipuncture.
Figure
Reference
-
1. Horowitz SH. Peripheral nerve injury and causalgia secondary to routine venipuncture. Neurology. 1994; 44:962–4.2. Newman BH, Waxman DA. Blood donation-related neurologic needle injury: evaluation of 2 years' worth of data from a large blood center. Transfusion. 1996; 36:213–5.3. Ialongo C, Bernardini S. Phlebotomy, a bridge between laboratory and patient. Biochem Med (Zagreb). 2016; 26:17–33.4. Kim HJ, Park SK, Park SH. Upper limb nerve injuries caused by intramuscular injection or routine venipuncture. Anesth Pain Med. 2017; 12:103–10.5. Berry PR, Wallis WE. Venepuncture nerve injuries. Lancet. 1977; 309:1236–7.6. Tsukuda Y, Funakoshi T, Nasuhara Y, Nagano Y, Shimizu C, Iwasaki N. Venipuncture nerve injuries in the upper extremity from more than 1 million procedures. J Patient Saf. 2019; 15:299–301.7. Yamada K, Yamada K, Katsuda I, Hida T. Cubital fossa venipuncture sites based on anatomical variations and relationships of cutaneous veins and nerves. Clin Anat. 2008; 21:307–13.8. Mikuni Y, Chiba S, Tonosaki Y. Topographical anatomy of superficial veins, cutaneous nerves, and arteries at venipuncture sites in the cubital fossa. Anat Sci Int. 2013; 88:46–57.9. Fuller G. How to get the most out of nerve conduction studies and electromyography. J Neurol Neurosurg Psychiatry. 2005; 76(Suppl 2):ii41–6.10. Kim S, Choi JY, Huh YM, Song HT, Lee SA, Kim SM, et al. Role of magnetic resonance imaging in entrapment and compressive neuropathy--what, where, and how to see the peripheral nerves on the musculoskeletal magnetic resonance image: part 2. Upper extremity. Eur Radiol. 2007; 17:509–22.11. Singh RK, Sinha VP, Pal US, Yadav SC, Singh MK. Pregabalin in post traumatic neuropathic pain: case studies. Natl J Maxillofac Surg. 2012; 3:91–5.12. Lewis SR, Price A, Walker KJ, McGrattan K, Smith AF. Ultrasound guidance for upper and lower limb blocks. Cochrane Database Syst Rev. 2015; 9:CD006459.13. Eker HE, Cok OY, Aribogan A, Arslan G. Management of neuropathic pain with methylprednisolone at the site of nerve injury. Pain Med. 2012; 13:443–51.14. Kim HJ, Park SH, Shin HY, Choi YS. Brachial plexus injury as a complication after nerve block or vessel puncture. Korean J Pain. 2014; 27:210–8.15. Ryan JA Jr, Abel RM, Abbott WM, Hopkins CC, Chesney TM, Colley R, et al. Catheter complications in total parenteral nutrition. A prospective study of 200 consecutive patients. N Engl J Med. 1974; 290:757–61.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Upper limb nerve injuries caused by intramuscular injection or routine venipuncture
- Sural nerve grafts in subacute facial nerve injuries: a report of two cases
- Recurrent Asystoles Associated with Vasovagal Reaction during Venipuncture
- Nerve Injury in Posterior Hip Fracture-Dislocation
- Successful Treatment of Vasovagal Syncope Due to Blood-Injury Phobia by Physical Maneuvering